Experiencing nausea or vomiting shortly after eating can be unsettling and, in some cases, a sign of an underlying health issue. While occasional post-meal discomfort may result from overeating or food intolerance, persistent or severe vomiting should never be ignored. Understanding the potential causes and knowing when to seek medical attention can prevent complications and improve long-term outcomes.
Common Causes of Vomiting After Eating
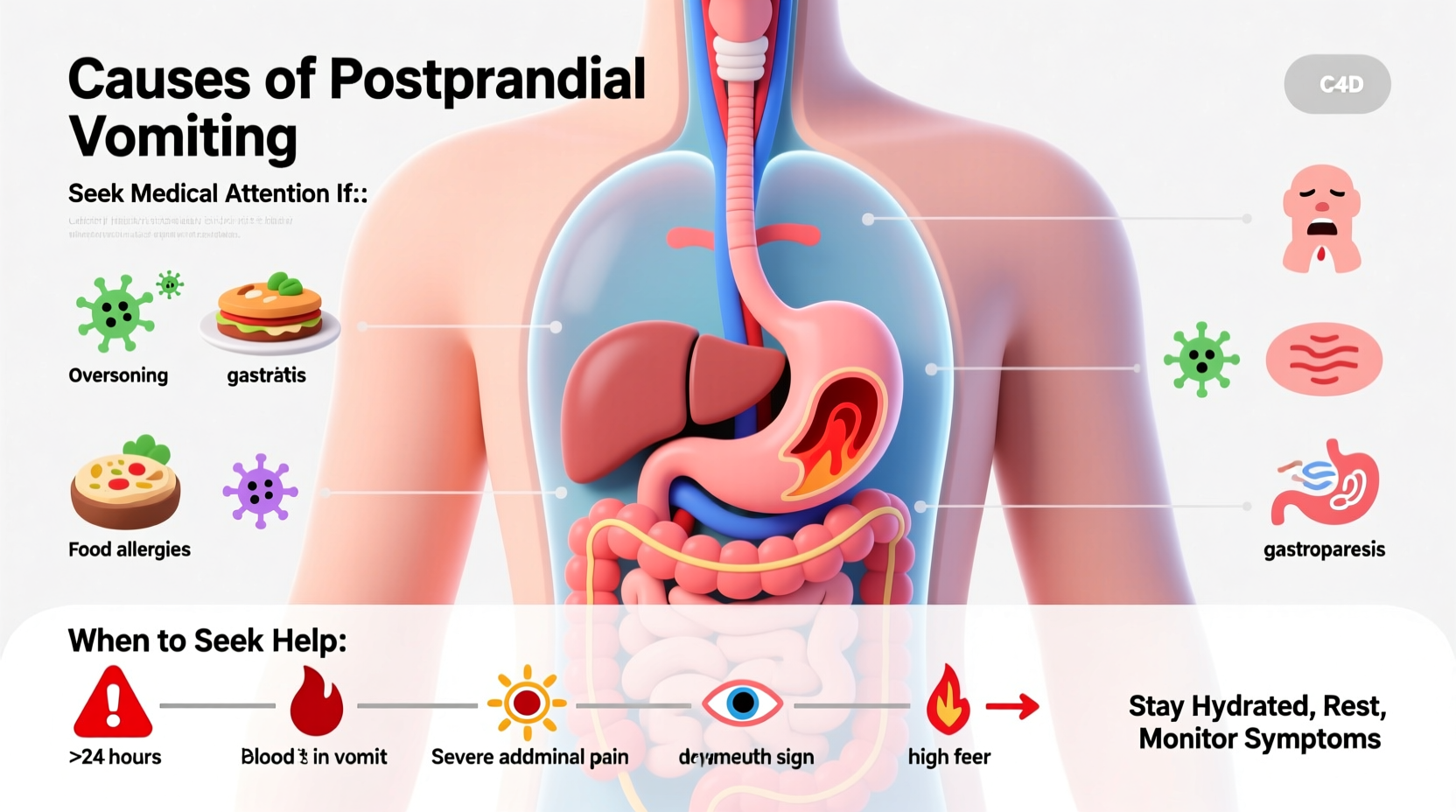
Vomiting after meals can stem from a variety of factors, ranging from mild digestive disturbances to more serious medical conditions. Some of the most frequent causes include:
- Overeating: Consuming large portions stretches the stomach, triggering nausea and sometimes vomiting.
- Food poisoning: Bacteria like Salmonella or E. coli can cause rapid-onset vomiting within hours of eating contaminated food.
- Gastroesophageal reflux disease (GERD): Stomach acid flows back into the esophagus, causing irritation and regurgitation.
- Food intolerances: Lactose intolerance or gluten sensitivity can lead to bloating, cramps, and vomiting after consuming trigger foods.
- Pregnancy: Morning sickness often includes nausea and vomiting, especially in the first trimester.
- Alcohol consumption: Drinking on an empty or full stomach can irritate the stomach lining and induce vomiting.
When Vomiting Signals a Serious Condition
While many cases resolve on their own, certain symptoms indicate a need for prompt medical evaluation. Persistent vomiting may point to more serious disorders such as:
- Gastroparesis: A condition where the stomach empties too slowly due to nerve damage, commonly seen in people with diabetes. Symptoms include early fullness, bloating, and vomiting undigested food hours after eating.
- Pyloric stenosis: Often found in infants but can occur in adults, this narrowing of the stomach’s exit valve blocks food passage, leading to forceful vomiting.
- Peptic ulcers: Open sores in the stomach lining or duodenum can cause pain after eating and vomiting, sometimes with blood.
- Intestinal obstruction: A blockage in the intestines prevents food from moving through, resulting in severe vomiting, abdominal pain, and inability to pass gas or stool.
- Appendicitis: Though typically associated with lower right pain, early stages may involve nausea and vomiting after meals.
- Pancreatitis: Inflammation of the pancreas often follows heavy meals or alcohol use, causing intense upper abdominal pain and recurrent vomiting.
“Recurrent vomiting after eating isn’t something to brush off. It can indicate anything from a minor intolerance to life-threatening conditions like bowel obstruction.” — Dr. Lena Patel, Gastroenterologist at Boston Medical Center
Red Flags: When to Seek Immediate Medical Help
Not all vomiting requires emergency care, but certain warning signs demand urgent attention. Seek immediate medical help if you or someone else experiences any of the following:
| Symptom | Potential Concern | Action Required |
|---|---|---|
| Vomiting blood (bright red or coffee-ground appearance) | Bleeding ulcer or tear in the esophagus | Go to ER immediately |
| Severe, unrelenting abdominal pain | Obstruction, appendicitis, or pancreatitis | Seek emergency evaluation |
| Inability to keep liquids down for 24+ hours | Dehydration risk, especially in children and elderly | Contact doctor or visit clinic |
| Vomiting that occurs consistently after every meal | Possible gastroparesis or structural issue | Schedule gastroenterology consult |
| Fever over 101°F with vomiting | Infection or inflammation | Medical assessment needed |
Real-Life Example: Recognizing Gastroparesis Early
Sarah, a 42-year-old office worker with type 2 diabetes, began experiencing nausea and vomiting 1–2 hours after meals. At first, she assumed it was indigestion. Over several weeks, the episodes worsened, and she lost 10 pounds unintentionally. Her primary care physician referred her to a gastroenterologist, who diagnosed diabetic gastroparesis through a gastric emptying study. With medication, dietary changes, and better blood sugar control, Sarah regained her appetite and stopped vomiting. Her case highlights the importance of not dismissing chronic post-meal vomiting as mere indigestion.
Practical Steps to Manage and Prevent Post-Meal Vomiting
If vomiting after eating is infrequent and mild, lifestyle adjustments may help reduce occurrences. Consider the following strategies:
Dietary Adjustments
- Avoid high-fat, greasy, or spicy foods that delay stomach emptying.
- Limit caffeine and carbonated beverages, which can increase acid reflux.
- Stay upright for at least 30 minutes after eating to prevent regurgitation.
- Chew food thoroughly to aid digestion and reduce stomach workload.
Hydration and Electrolyte Balance
Vomiting leads to fluid loss and electrolyte imbalances. Sip small amounts of clear fluids like water, broth, or oral rehydration solutions. Avoid gulping large volumes, which may trigger further nausea.
Medication Review
Some medications, including opioids, certain antidepressants, and diabetes drugs like exenatide, can slow gastric motility. Discuss side effects with your doctor; alternatives may be available.
Checklist: What to Do If You Vomit After Eating
- Pause eating and rest in an upright position.
- Sip small amounts of clear fluid every 15 minutes.
- Monitor for red flag symptoms (blood, severe pain, dehydration).
- Record frequency, timing, and contents of vomit.
- Avoid solid foods until nausea subsides for several hours.
- Contact a healthcare provider if vomiting persists beyond 24 hours or recurs regularly.
FAQ
Can anxiety cause vomiting after eating?
Yes. Anxiety activates the autonomic nervous system, which can disrupt digestion and trigger nausea or vomiting, especially during or after meals. This is more common in individuals with panic disorder or eating-related stress.
Is it normal to throw up after every meal during pregnancy?
While morning sickness is common, vomiting after every single meal is not considered normal. Hyperemesis gravidarum—a severe form of pregnancy-related nausea—can lead to dehydration and weight loss and requires medical treatment.
How is the cause of post-meal vomiting diagnosed?
Doctors may use endoscopy, gastric emptying studies, blood tests, or imaging (like CT scans) to evaluate the digestive tract. A detailed symptom history is crucial for accurate diagnosis.
Conclusion: Take Action Before It Gets Worse
Vomiting after eating is more than just an unpleasant experience—it can be a signal that your body needs attention. Whether it's a temporary reaction to spoiled food or a symptom of a chronic condition, ignoring repeated episodes can lead to malnutrition, dehydration, or delayed treatment. Pay attention to patterns, document symptoms, and don’t hesitate to reach out to a healthcare professional. Your digestive health is foundational to your overall well-being.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?