Occasionally, people notice they're bringing up thick saliva or mucus without actual vomiting. While this may seem minor, frequent or persistent episodes of \"throwing up spit\" can signal underlying health conditions. Understanding the difference between normal postnasal drip and more serious digestive or neurological issues is key to knowing when to seek medical help.
This condition—often described as regurgitating clear or white frothy liquid, phlegm, or stringy mucus—is not typical vomiting but rather a reflexive expulsion of oral or esophageal contents. It can occur upon waking, after meals, or during moments of nausea. Recognizing the root cause helps determine whether it's a temporary irritation or something requiring treatment.
Common Causes of Spitting Up Saliva or Mucus
The sensation of needing to expel saliva or mucus frequently may stem from several sources, ranging from mild allergies to chronic gastrointestinal disorders.
- Postnasal Drip: Excess mucus from the sinuses draining into the throat often leads to frequent throat clearing or spitting, especially in the morning.
- Gastroesophageal Reflux Disease (GERD): Stomach acid backing up into the esophagus can stimulate excess saliva production as a protective mechanism, leading to spitting or regurgitation of foamy fluid.
- Nausea and Morning Sickness: Pregnant individuals or those with motion sickness may produce excessive saliva (a condition called ptyalism) and feel compelled to spit it out.
- Dental or Oral Infections: Gum disease, abscesses, or tonsillitis can increase saliva viscosity and volume, making spitting more common.
- Dehydration: Paradoxically, dry mouth due to dehydration can trigger overproduction of thick, sticky saliva that feels unpleasant and prompts spitting.
When Digestive Issues Are to Blame
The digestive tract plays a major role in saliva regulation. Conditions like GERD and gastroparesis disrupt normal motility and can lead to unusual oral secretions.
In GERD, stomach acid irritates the lower esophagus, prompting the salivary glands to release more saliva to neutralize the acid—a response known as “water brash.” This results in a sudden flood of watery or frothy saliva that some people spit out rather than swallow.
Gastroparesis, a disorder where the stomach empties too slowly, often seen in diabetics, can also cause nausea and hypersalivation. Delayed gastric emptying increases pressure in the stomach, pushing fluids upward and triggering the urge to spit.
“Excessive spitting of saliva, particularly when associated with heartburn or regurgitation, should prompt evaluation for acid reflux,” says Dr. Lena Torres, gastroenterologist at Midwest Digestive Health Center.
Symptoms That Suggest a GI Origin
- Burning sensation in the chest (heartburn)
- Regurgitation of sour liquid or food
- Frequent burping or bloating
- Worsening symptoms after eating or lying down
Respiratory and Sinus-Related Triggers
Chronic sinusitis, allergies, and respiratory infections are among the most common non-digestive reasons for increased mucus production and spitting.
When allergens or viruses inflame nasal passages, the body produces extra mucus that drips down the back of the throat. This postnasal drip accumulates overnight or after exposure, causing a constant need to clear the throat or spit out phlegm.
| Cause | Typical Symptoms | Duration |
|---|---|---|
| Allergic Rhinitis | Itchy eyes, sneezing, runny nose, clear mucus | Seasonal or year-round |
| Viral Sinus Infection | Thick yellow/green mucus, facial pain, congestion | 7–14 days |
| Chronic Bronchitis | Persistent cough with mucus, especially in smokers | At least 3 months per year for two consecutive years |
Neurological and Hormonal Factors
Less commonly, neurological conditions or hormonal shifts can influence saliva control.
Pregnancy-induced nausea, particularly in the first trimester, is frequently accompanied by ptyalism—excessive saliva production. Though not harmful, it can be distressing and lead to repeated spitting.
Neurological disorders such as Parkinson’s disease impair swallowing reflexes, resulting in drooling or unintentional spitting. Similarly, stroke survivors may experience difficulty managing oral secretions due to muscle weakness.
Red Flags Indicating Neurological Involvement
- Tremors or stiffness
- Difficulty speaking or swallowing
- Unexplained weight loss
- Muscle weakness or coordination problems
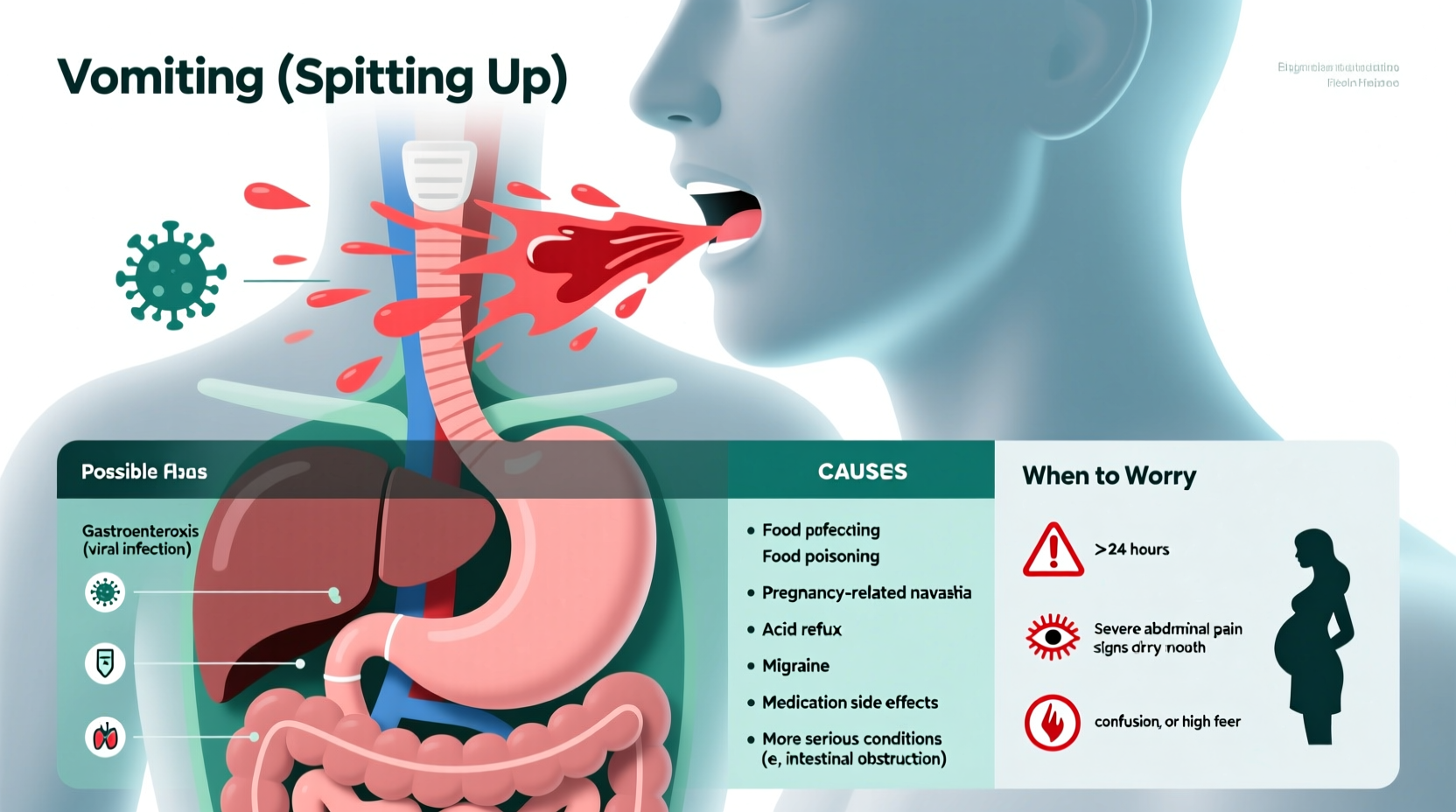
When to Worry: Warning Signs That Need Medical Attention
While occasional spitting of saliva or mucus is usually benign, certain symptoms indicate a need for professional evaluation.
Seek immediate medical care if you experience:
- Blood in the expelled fluid – Could indicate ulceration, severe inflammation, or malignancy.
- Persistent vomiting or retching – May point to bowel obstruction or severe gastroparesis.
- Unintentional weight loss – A potential sign of chronic illness or cancer.
- Dysphagia (painful or difficult swallowing) – Suggests structural or neuromuscular issues.
- Fever with colored phlegm lasting over 10 days – May indicate bacterial infection requiring antibiotics.
“If someone suddenly begins spitting up large amounts of frothy saliva and has trouble keeping liquids down, we consider both gastrointestinal and neurological causes until proven otherwise,” notes Dr. Alan Mehta, internal medicine physician.
Step-by-Step Guide to Managing and Monitoring Symptoms
- Track your symptoms: Note when spitting occurs (e.g., after meals, at night), the consistency of the fluid, and any accompanying sensations like heartburn or nausea.
- Adjust lifestyle habits: Avoid late-night eating, elevate your head while sleeping, reduce caffeine and alcohol, and stay well-hydrated.
- Use saline rinses: For postnasal drip, daily nasal irrigation with saline can reduce mucus buildup.
- Try over-the-counter remedies: Antacids or H2 blockers (like famotidine) may help if GERD is suspected. Antihistamines can ease allergy-related mucus.
- Schedule a doctor’s visit: If symptoms persist beyond two weeks or worsen, see a healthcare provider for evaluation.
Mini Case Study: Persistent Morning Spitting
Sarah, a 34-year-old office worker, began noticing she was spitting up thick, clear mucus every morning. She initially dismissed it as seasonal allergies, but after three weeks of worsening congestion and a nagging sore throat, she consulted her doctor.
Upon examination, she was diagnosed with chronic sinusitis complicated by mild GERD. Her nighttime acid reflux was exacerbating postnasal drip. With a regimen of nasal steroids, a proton pump inhibitor, and sleep elevation, her symptoms resolved within six weeks.
Sarah’s case illustrates how overlapping conditions can mimic simple mucus buildup but require targeted treatment.
Checklist: What You Can Do Today
- ✅ Drink plenty of water to thin mucus
- ✅ Avoid lying down within 3 hours of eating
- ✅ Use a humidifier if air is dry
- ✅ Practice good oral hygiene to prevent infections
- ✅ Keep a symptom journal for your doctor
- ✅ Eliminate known allergens (dust, pet dander, smoke)
Frequently Asked Questions
Is spitting up white foam a sign of acid reflux?
Yes, white foamy saliva, especially when accompanied by heartburn or a sour taste, is often linked to GERD. The foam results from air mixing with excess saliva produced to buffer stomach acid.
Can anxiety cause me to spit up saliva?
Indirectly, yes. Anxiety can increase swallowing frequency and awareness of saliva, leading to a perceived need to spit. It may also worsen acid reflux, further stimulating saliva production.
Why do I spit up phlegm only at night?
Lying flat allows mucus to pool in the throat and enables stomach acid to reflux more easily. Elevating your head during sleep can significantly reduce nighttime symptoms.
Conclusion: Know Your Body, Take Action
Spitting up saliva or mucus isn’t always a cause for alarm, but it shouldn’t be ignored if it becomes routine or disruptive. Whether it stems from allergies, reflux, or a deeper health issue, early recognition and intervention make a meaningful difference.
Pay attention to patterns, adjust your habits, and don’t hesitate to reach out to a healthcare provider if something feels off. Your body is sending signals—listening now can prevent complications later.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?