When blood tests reveal a high Total Iron-Binding Capacity (TIBC), it often points to a deeper imbalance within the body’s iron metabolism. This finding is especially common in individuals diagnosed with iron deficiency anemia. While the term may sound technical, understanding what TIBC measures—and why it increases—can empower patients and caregivers to make informed decisions about treatment and lifestyle adjustments. This article explores the physiological mechanisms behind elevated TIBC, its clinical significance, and how it fits into the broader picture of diagnosing and managing iron deficiency.
What Is TIBC and How Does It Relate to Iron?
Total Iron-Binding Capacity (TIBC) is a laboratory test that estimates the maximum amount of iron your blood can bind to proteins, primarily transferrin. Transferrin, produced by the liver, is the main protein responsible for transporting iron through the bloodstream to tissues like bone marrow, where it's used to produce hemoglobin.
TIBC doesn't measure iron directly. Instead, it reflects how much transferrin is available to carry iron. When iron levels drop, the liver responds by producing more transferrin in an effort to scavenge whatever iron is available. This increase in transferrin leads to a higher TIBC.
In iron deficiency anemia, this mechanism becomes a key diagnostic clue. A high TIBC signals that the body is attempting to compensate for low iron stores—a sort of biological \"search and rescue\" operation for missing iron.
Why Is TIBC High in Iron Deficiency Anemia?
The elevation of TIBC in iron deficiency anemia is a compensatory response driven by hormonal and genetic regulation. When iron stores fall—often due to chronic blood loss, poor dietary intake, or increased demand (such as during pregnancy)—the hormone hepcidin decreases. Low hepcidin allows more iron absorption from the gut and increased release of stored iron, but when reserves are depleted, the body turns to another strategy: boosting iron transport capacity.
The liver senses low iron and upregulates the production of transferrin. More transferrin means higher iron-binding potential, hence a higher TIBC. This adaptive response aims to maximize the capture and delivery of any available iron to red blood cell precursors in the bone marrow.
This phenomenon distinguishes iron deficiency anemia from other types of anemia, such as anemia of chronic disease, where TIBC is typically low or normal due to inflammation suppressing transferrin synthesis.
“Elevated TIBC is one of the most reliable indirect markers of iron deficiency. It reflects the body’s attempt to correct a deficit even before symptoms become severe.” — Dr. Lena Patel, Hematology Specialist
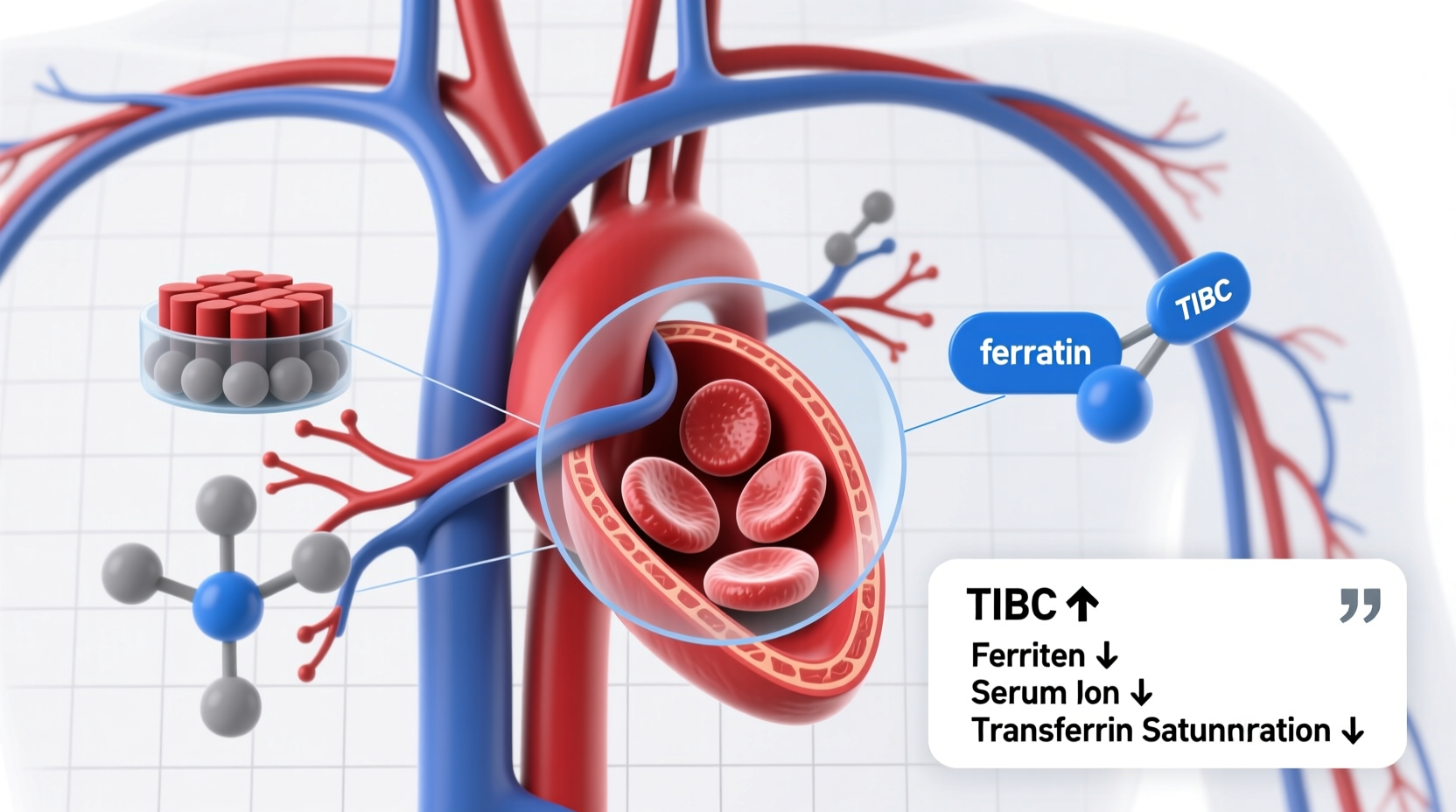
Interpreting TIBC in Context: Key Lab Values Compared
Understanding TIBC requires looking at it in conjunction with other iron studies. The table below outlines typical lab patterns in different conditions:
| Condition | Serum Iron | TIBC | Transferrin Saturation | Ferritin |
|---|---|---|---|---|
| Iron Deficiency Anemia | Low | High | Low (<16%) | Low |
| Anemia of Chronic Disease | Low | Low/Normal | Low | Normal/High |
| Iron Overload (Hemochromatosis) | High | Low/Normal | High (>45%) | High |
As shown, a high TIBC combined with low serum iron and low ferritin strongly supports iron deficiency anemia. Transferrin saturation—calculated as (serum iron ÷ TIBC) × 100—is particularly useful; values below 16% are indicative of inadequate iron delivery to tissues.
Common Causes of Iron Deficiency Leading to High TIBC
While the biochemical response is clear, identifying the underlying cause of iron deficiency is crucial for effective treatment. Common reasons include:
- Chronic blood loss: In men and postmenopausal women, gastrointestinal bleeding (e.g., ulcers, colon cancer) is a leading cause. In premenopausal women, heavy menstrual bleeding is frequent.
- Poor dietary intake: Diets low in heme iron (found in meat) or non-heme iron (plant sources) can contribute, especially in vegetarians or those with malabsorption.
- Inadequate absorption: Conditions like celiac disease, inflammatory bowel disease, or gastric bypass surgery impair iron uptake.
- Increased demand: Pregnancy, lactation, and periods of rapid growth (e.g., adolescence) elevate iron needs.
Each of these triggers the same cascade: falling iron stores → reduced hepcidin → increased transferrin production → elevated TIBC.
Mini Case Study: Identifying Hidden Blood Loss
Sarah, a 42-year-old teacher, presented with fatigue, pallor, and shortness of breath. Her lab results showed:
- Serum iron: 32 µg/dL (low)
- TIBC: 470 µg/dL (high)
- Ferritin: 8 ng/mL (very low)
- Transferrin saturation: 7%
These findings confirmed iron deficiency anemia. Despite a balanced diet, her ferritin remained critically low after oral iron therapy. Further investigation revealed a small colorectal polyp causing slow, chronic bleeding—identified via colonoscopy. After polyp removal and iron repletion, her energy returned and labs normalized.
This case illustrates how a high TIBC guides diagnosis but also underscores the need to investigate root causes beyond supplementation.
Step-by-Step: Evaluating High TIBC in Clinical Practice
When a patient presents with suspected anemia and a high TIBC, a structured approach ensures accurate diagnosis and management:
- Confirm iron deficiency: Check serum ferritin (best indicator of iron stores), serum iron, and calculate transferrin saturation.
- Assess severity: Evaluate hemoglobin levels and red blood cell indices (e.g., MCV—mean corpuscular volume—often low in iron deficiency).
- Identify the cause: Take a detailed history (diet, menstruation, GI symptoms) and consider testing for occult blood in stool, celiac serology, or endoscopic evaluation if indicated.
- Initiate treatment: Oral iron supplements (e.g., ferrous sulfate) are first-line. In cases of malabsorption or intolerance, intravenous iron may be needed.
- Monitor response: Recheck hemoglobin and reticulocyte count after 2–4 weeks. Ferritin should rise after several weeks of therapy.
FAQ: Common Questions About High TIBC and Iron Deficiency
Can TIBC be high without anemia?
Yes. In the early stages of iron depletion, ferritin drops and TIBC rises, but hemoglobin remains normal. This is called “iron deficiency without anemia” and can still cause fatigue and impaired cognition.
Does a high TIBC always mean iron deficiency?
Not always. Pregnancy and estrogen therapy (e.g., birth control pills) can increase transferrin and thus TIBC, even with normal iron stores. Always correlate with ferritin and clinical context.
How long does it take for TIBC to normalize after treatment?
TIBC typically begins to decline within a few weeks of starting iron replacement, as transferrin production decreases once iron status improves. Full normalization may take 2–3 months.
Action Plan: What to Do If Your TIBC Is High
If your lab report shows a high TIBC, follow this checklist to address the issue effectively:
- ✅ Review all iron panel results: Don’t focus on TIBC alone—check ferritin, serum iron, and saturation.
- ✅ Evaluate symptoms: Fatigue, dizziness, brittle nails, and restless legs may point to deficiency.
- ✅ Identify potential causes: Consider diet, blood loss, medications, or underlying conditions.
- ✅ Consult a healthcare provider: Avoid self-treating with iron supplements without confirmation—excess iron can be harmful.
- ✅ Follow up with repeat testing: Monitor progress and ensure the underlying cause is resolved.
Conclusion: Turning Lab Results Into Health Action
A high TIBC in the setting of iron deficiency anemia is not just a lab anomaly—it’s a signal from your body that iron balance is disrupted. Understanding this marker empowers you to seek appropriate care, uncover hidden causes, and restore vitality through targeted treatment. Whether due to nutrition, blood loss, or absorption issues, iron deficiency is treatable when caught early. Use your lab results as a starting point, not an endpoint. Work with your healthcare provider, ask questions, and take proactive steps toward better energy, stronger immunity, and improved overall health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?