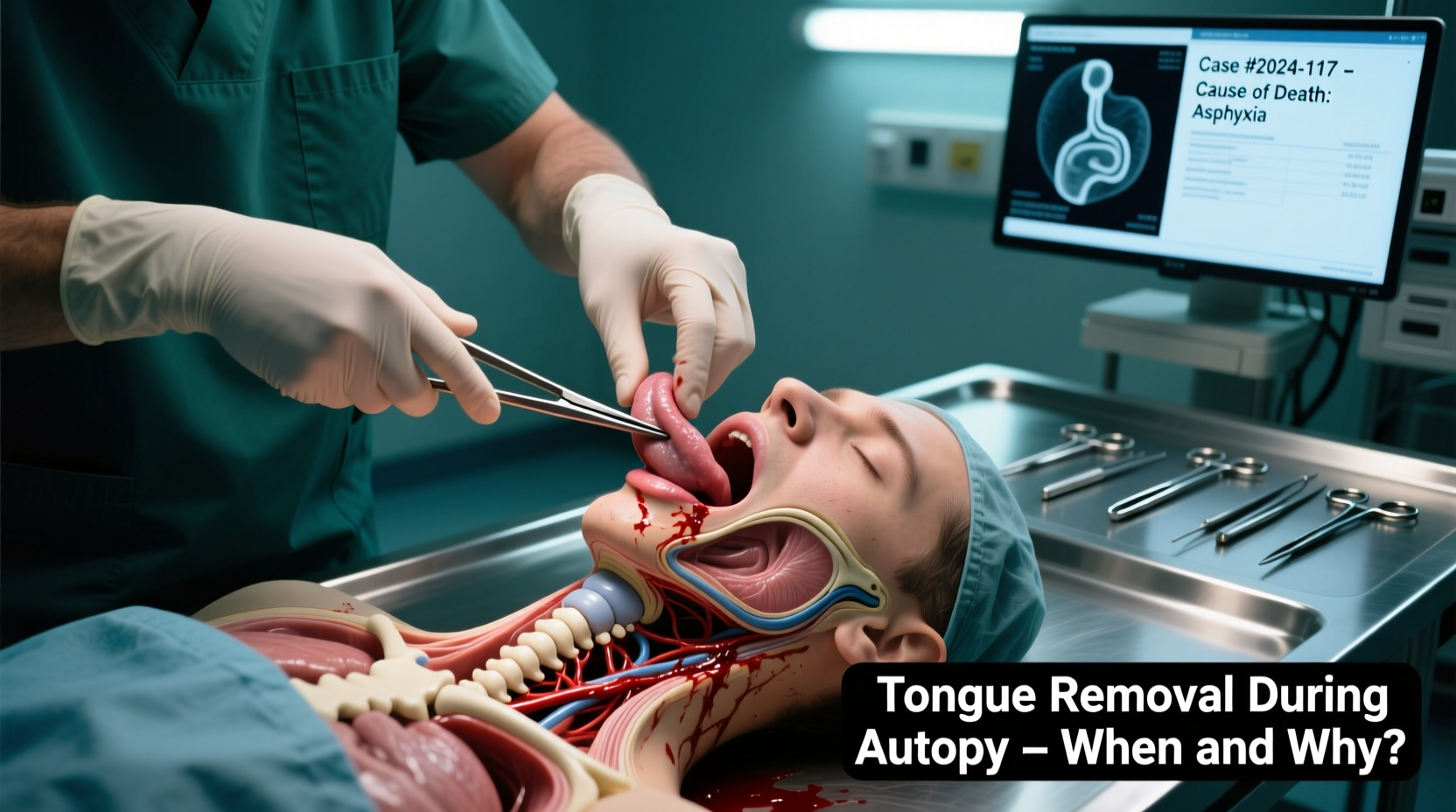
In the course of a forensic or medical autopsy, certain organs are systematically removed, examined, and sometimes retained for further analysis. Among these, the tongue may be one of the less-discussed structures, yet its removal can play a crucial role in determining cause of death, identifying disease, or confirming trauma. While not routinely removed in every case, there are specific circumstances under which pathologists choose to excise the tongue. Understanding when and why this occurs sheds light on the meticulous nature of postmortem examination and the importance of even seemingly minor anatomical structures in forensic diagnostics.
Why the Tongue May Be Removed During Autopsy
The decision to remove the tongue during an autopsy is not arbitrary. It is based on clinical suspicion, observed pathology, or investigative necessity. The tongue, though small, is rich in vascular and lymphatic tissue and serves as a potential indicator of systemic conditions, infections, or traumatic injury. When signs point to oral trauma, poisoning, or diseases affecting soft tissues, the tongue becomes a focal point of interest.
One primary reason for removal is to investigate evidence of asphyxiation. In cases of strangulation or hanging, petechial hemorrhages or ligature marks may extend into the oral cavity. The base of the tongue and the hyoid bone region are particularly scrutinized. If bruising, lacerations, or fractures are suspected, removing the tongue allows for a more thorough inspection of underlying musculature and attachment points.
“Even subtle injuries in the oral cavity can be pivotal in reconstructing the mechanism of death, especially in suspected homicides involving manual strangulation.” — Dr. Lena Patel, Forensic Pathologist, Office of the Chief Medical Examiner
Another significant reason involves toxicological or histopathological analysis. If antemortem reports suggest ingestion of corrosive substances—such as strong acids or alkalis—the tongue may show signs of chemical burns. Removing and preserving the tissue enables microscopic evaluation to confirm exposure and assess the extent of damage.
Medical Conditions That Prompt Tongue Examination
Certain diseases manifest visibly in the oral mucosa or lingual tissue. When such conditions are suspected, the tongue may be removed for diagnostic confirmation. These include:
- Severe infections: Fungal (e.g., candidiasis), bacterial (e.g., syphilis), or viral (e.g., herpes) infections can leave characteristic lesions.
- Neoplasms: Tumors of the tongue, whether benign or malignant, require histological examination to determine origin, stage, and contribution to death.
- Autoimmune disorders: Conditions like pemphigus vulgaris or lichen planus may present with erosive lesions in the mouth.
- Nutritional deficiencies: Severe vitamin B deficiencies or anemia can alter the tongue’s appearance (e.g., glossitis).
In cases where the deceased had prolonged illness or difficulty swallowing, examining the tongue helps correlate clinical symptoms with pathological findings. For example, muscle atrophy in the tongue might support a diagnosis of motor neuron disease like ALS.
Procedural Steps in Tongue Removal
Tongue removal is typically performed during the dissection of the neck and upper airway. It is not a standalone procedure but part of a broader examination of the oral cavity, pharynx, and larynx. The following steps outline the standard approach:
- External inspection: The mouth is opened, and the tongue is visually assessed for color, lesions, trauma, or foreign material.
- Midsagittal incision: A cut is made down the center of the tongue from tip to base to examine internal structure and symmetry.
- Dissection of attachments: The genioglossus muscles and hyoglossus attachments are carefully severed at the mandible and hyoid bone.
- Separation from pharynx: The posterior aspect of the tongue is freed from the epiglottis and oropharyngeal walls.
- Removal and weighing: The entire tongue is excised, weighed, and documented as part of organ inventory.
- Sampling: Sections are taken for histology; additional portions may be preserved for toxicology or microbiology.
This process ensures that both macroscopic and microscopic features are captured. The weight and consistency of the tongue can also provide clues—edema may indicate systemic fluid imbalance, while atrophy suggests chronic illness.
When Is the Tongue Not Removed?
It's important to clarify that tongue removal is not standard in every autopsy. In routine medicolegal or hospital autopsies where no oral pathology is suspected, the tongue is often left intact after visual inspection. The decision hinges on the autopsy protocol and the case-specific findings.
The table below summarizes common scenarios that influence whether the tongue is removed:
| Scenario | Tongue Removed? | Rationale |
|---|---|---|
| Natural death, no oral symptoms | No | No indication for deeper investigation |
| Suspected strangulation | Yes | To assess deep tissue bruising and muscle trauma |
| Known oral cancer | Yes | To evaluate tumor spread and margins |
| Unexplained coma or poisoning | Possibly | If caustic ingestion is suspected |
| Severe burns or fire victim | Yes | To check for inhalation injury or carbon deposits |
Case Example: Uncovering Hidden Trauma
In a 2021 case reviewed by the Cook County Medical Examiner’s Office, a 34-year-old male was found unconscious in his apartment with no clear signs of trauma. Initial external exam showed only faint redness around the neck. During autopsy, the pathologist noted slight swelling of the tongue and decided to remove it for cross-sectioning. Microscopic analysis revealed diffuse petechial hemorrhages in the intrinsic muscles—indicative of sustained pressure consistent with manual strangulation. Further investigation led to the arrest of a family member who had claimed the death was due to a drug overdose. This case underscores how a seemingly minor decision—to remove the tongue—can be pivotal in uncovering foul play.
Legal and Ethical Considerations
The removal of any organ, including the tongue, must comply with legal and ethical standards. In most jurisdictions, autopsies conducted under coroner or medical examiner authority do not require family consent when deemed necessary for public health or criminal investigation. However, transparency is key. Families may be informed post-examination about which organs were retained, especially if tissue is kept for long-term study or court evidence.
Religious or cultural sensitivities must also be considered. Some belief systems emphasize bodily integrity after death. While the law generally permits necessary procedures, many morgues work to minimize disfigurement and return all tissues when possible after analysis.
Frequently Asked Questions
Is the tongue always removed during an autopsy?
No, the tongue is only removed when clinically indicated—such as in cases of suspected trauma, poisoning, or disease. In routine autopsies, it is typically inspected but left intact.
Can the tongue reveal evidence of poisoning?
Yes. Corrosive poisons like lye or sulfuric acid cause visible burns and tissue necrosis on the tongue. Ingested toxins may also leave residues detectable through chemical analysis of lingual tissue.
Does removing the tongue affect the appearance of the body?
When performed correctly, tongue removal does not alter facial appearance. The procedure is done internally, and the mouth remains closed during viewing. No external scars are visible.
Checklist: When to Consider Tongue Removal in Autopsy
- ☑ Signs of neck compression (ligature marks, bruising)
- ☑ History of difficulty swallowing or oral pain
- ☑ Visible lesions, ulcers, or tumors in the mouth
- ☑ Suspected chemical ingestion
- ☑ Fire or smoke inhalation victims
- ☑ Unexplained sudden death with no clear cause
- ☑ Need for histological confirmation of disease
Conclusion
The removal of the tongue during an autopsy is a targeted, purposeful act—not a routine step, but a critical one when circumstances demand it. Whether revealing hidden trauma, confirming disease, or providing toxicological evidence, the tongue can hold answers that other organs cannot. Forensic pathologists rely on meticulous observation and judgment to decide when deeper investigation is warranted. For families, understanding this process can demystify autopsy procedures and underscore their importance in seeking truth and justice. As medical science advances, even the smallest tissues continue to play outsized roles in solving the mysteries of death.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?