Difficulty starting or maintaining urine flow is more than just a minor inconvenience—it can signal underlying health issues that require attention. Urinary hesitancy and retention affect millions of people, particularly as they age, yet many suffer in silence due to embarrassment or lack of awareness. Recognizing the signs early and understanding potential causes can lead to timely intervention and better outcomes.
This article explores urinary hesitancy and retention in depth, covering their definitions, common causes, risk factors, diagnostic approaches, and evidence-based treatments. Whether you're experiencing mild delays in urination or complete inability to void, this guide provides practical insights to help you navigate the condition with confidence.
What Are Urinary Hesitancy and Retention?
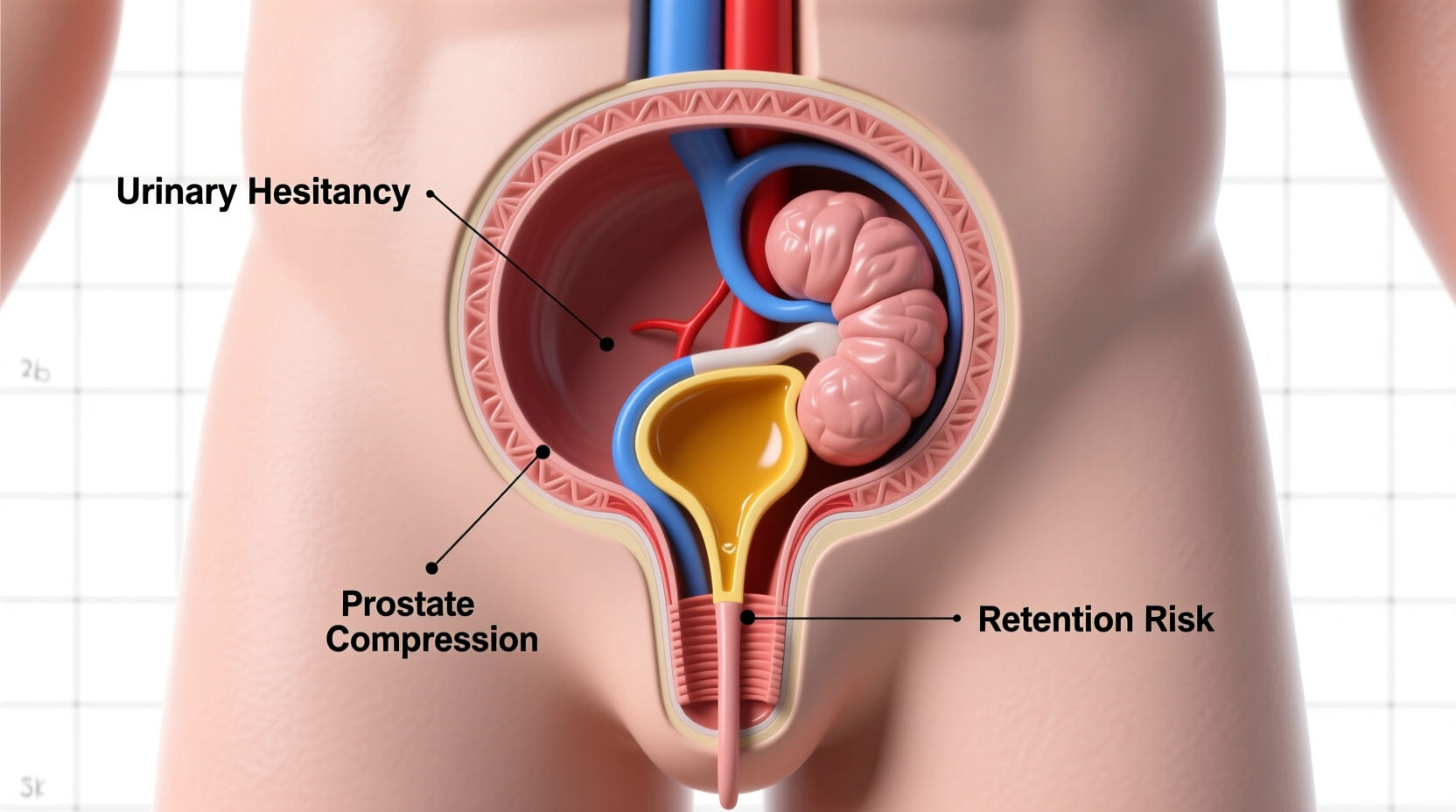
Urinary hesitancy refers to difficulty initiating urination. Individuals may feel the urge to go but experience a delay before the stream begins, often accompanied by straining or weak flow. Over time, this can progress to urinary retention—the inability to empty the bladder completely or at all.
Retention is classified into two types:
- Acute urinary retention: Sudden and painful inability to urinate. This is a medical emergency requiring immediate treatment.
- Chronic urinary retention: A long-term condition where the bladder doesn’t fully empty. Symptoms may be subtle, such as frequent urination or a constant feeling of fullness.
Both conditions disrupt quality of life and increase the risk of complications like urinary tract infections (UTIs), bladder damage, and kidney problems if left untreated.
Common Causes and Risk Factors
Multiple physiological and pathological factors contribute to urinary hesitancy and retention. The most prevalent causes vary by gender and age.
In Men
The leading cause is benign prostatic hyperplasia (BPH)—noncancerous enlargement of the prostate gland. As the prostate grows, it compresses the urethra, obstructing urine flow. Other male-specific contributors include:
- Prostatitis (inflammation of the prostate)
- Prostate cancer or its treatment (e.g., surgery, radiation)
- Urethral strictures from injury or infection
In Women
While less common, women can also experience hesitancy due to pelvic organ prolapse, previous pelvic surgeries, or nerve dysfunction. Conditions like multiple sclerosis or diabetes can impair bladder control regardless of gender.
General Causes Across Genders
| Cause | Description |
|---|---|
| Medications | Antihistamines, decongestants, antidepressants, and antipsychotics can interfere with bladder muscle contraction. |
| Nerve Damage | Spinal cord injuries, stroke, Parkinson’s disease, or diabetic neuropathy disrupt signals between the brain and bladder. |
| Bladder Muscle Weakness | Aging or chronic overdistension can weaken detrusor muscles responsible for expulsion. |
| Constipation | Fecal impaction can press on the bladder or urethra, impairing function. |
| Anesthesia or Surgery | Postoperative urinary retention is common after procedures involving general anesthesia, especially abdominal or pelvic surgeries. |
“Persistent urinary hesitancy should never be dismissed as normal aging. It’s a symptom that warrants evaluation.” — Dr. Alan Weiss, Urologist and Clinical Professor at Johns Hopkins Medicine
Diagnosis: How Doctors Identify the Problem
Accurate diagnosis begins with a thorough medical history and physical exam. Your doctor will ask about medication use, onset of symptoms, frequency, and associated pain. For men, a digital rectal exam assesses prostate size and tenderness.
Diagnostic tests may include:
- Urinalysis: To check for infection, blood, or glucose.
- Post-void residual (PVR) measurement: An ultrasound or catheterization test to determine how much urine remains after voiding. A volume exceeding 100–150 mL suggests incomplete emptying.
- Uroflowmetry: Measures the speed and volume of urine flow.
- Bladder scan: Non-invasive imaging to visualize bladder capacity and retention.
- Cystoscopy or urodynamic testing: In complex cases, these assess internal anatomy and pressure dynamics within the bladder.
These tools help differentiate between obstructive causes (like BPH) and neurogenic or muscular dysfunction, guiding appropriate treatment.
Treatment Options Based on Cause
Effective management depends on identifying the root issue. Treatment ranges from lifestyle adjustments to surgical interventions.
Lifestyle and Behavioral Strategies
- Double voiding: After finishing urination, wait a moment, then try again to expel remaining urine.
- Timed voiding: Schedule bathroom visits every 2–4 hours to prevent overfilling.
- Fluid management: Avoid excessive intake before bedtime; limit caffeine and alcohol, which irritate the bladder.
Medications
For men with BPH:
- Alpha-blockers (e.g., tamsulosin): Relax prostate and bladder neck muscles to improve flow.
- 5-alpha reductase inhibitors (e.g., finasteride): Shrink the prostate over several months.
If medications are the culprit, adjusting dosage or switching drugs under medical supervision may resolve symptoms.
Surgical and Procedural Interventions
When conservative methods fail:
- Transurethral resection of the prostate (TURP): Removes excess prostate tissue blocking the urethra.
- Urethral stents or dilation: Used for strictures.
- Intermittent self-catheterization: For chronic retention, patients learn to insert a catheter periodically to drain the bladder safely.
Mini Case Study: John’s Experience with BPH
John, a 62-year-old teacher, began noticing he had to wait longer to start urinating. He’d wake up three to four times nightly and felt urgency but often passed only small amounts. At first, he attributed it to drinking too much tea. But when he developed mild flank pain and fatigue, his primary care physician ordered a PVR test. Results showed 220 mL of retained urine.
After a referral to urology, John was diagnosed with moderate BPH. He started tamsulosin and noticed improvement within a week. With follow-up care and lifestyle changes—including reduced evening fluids and regular exercise—his symptoms stabilized. Six months later, his PVR dropped to 60 mL, and nocturia decreased to once per night.
John’s case illustrates how early detection and targeted therapy can significantly improve daily functioning and prevent complications like UTIs or kidney strain.
Checklist: When to See a Doctor
Use this checklist to evaluate whether your symptoms warrant medical attention:
- Needing to push or strain to start urination
- Feeling that your bladder isn’t fully empty after going
- Waking frequently at night to urinate (more than twice)
- Pain or discomfort in the lower abdomen or back
- Loss of bladder control or dribbling after urination
- Sudden inability to urinate
- Blood in the urine
If two or more apply, schedule an appointment with your healthcare provider or a urologist.
Frequently Asked Questions
Can urinary retention go away on its own?
Mild, temporary retention—such as after surgery or due to dehydration—may resolve without treatment. However, persistent or recurrent symptoms typically require medical evaluation. Ignoring chronic retention risks bladder damage and infection.
Is urinary hesitancy only a problem for older men?
No. While more common in aging men due to prostate changes, women and younger individuals can also experience hesitancy from nerve disorders, medications, or pelvic floor dysfunction. It’s not exclusively an age- or gender-related issue.
Can drinking more water help with retention?
Yes, staying well-hydrated supports healthy urinary function. However, timing matters. Excessive fluid intake late at night can worsen nocturia. Aim for steady hydration throughout the day and reduce intake 2–3 hours before bed.
Take Control of Your Bladder Health
Urinary hesitancy and retention are treatable conditions—not inevitable parts of aging. Understanding the causes empowers you to take proactive steps, from modifying habits to seeking expert care. Don’t let discomfort or stigma delay action. Early intervention preserves bladder function, prevents complications, and enhances overall well-being.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?