Gas is a normal part of digestion—everyone produces and expels it daily. But when you're struggling to pass gas, the result can be uncomfortable bloating, sharp cramps, and even chest tightness that mimics more serious conditions. This condition, often dismissed as minor, affects millions and can significantly impact quality of life. Understanding why it's hard to fart and what you can do about it isn’t just about comfort—it’s about gut health and digestive function.
The inability to release gas, sometimes called \"trapped wind,\" occurs when intestinal motility slows or when posture, diet, or stress interferes with natural expulsion. While occasional gas retention is common, chronic difficulty passing gas may point to underlying issues like irritable bowel syndrome (IBS), constipation, or pelvic floor dysfunction.
The Science Behind Gas Build-Up
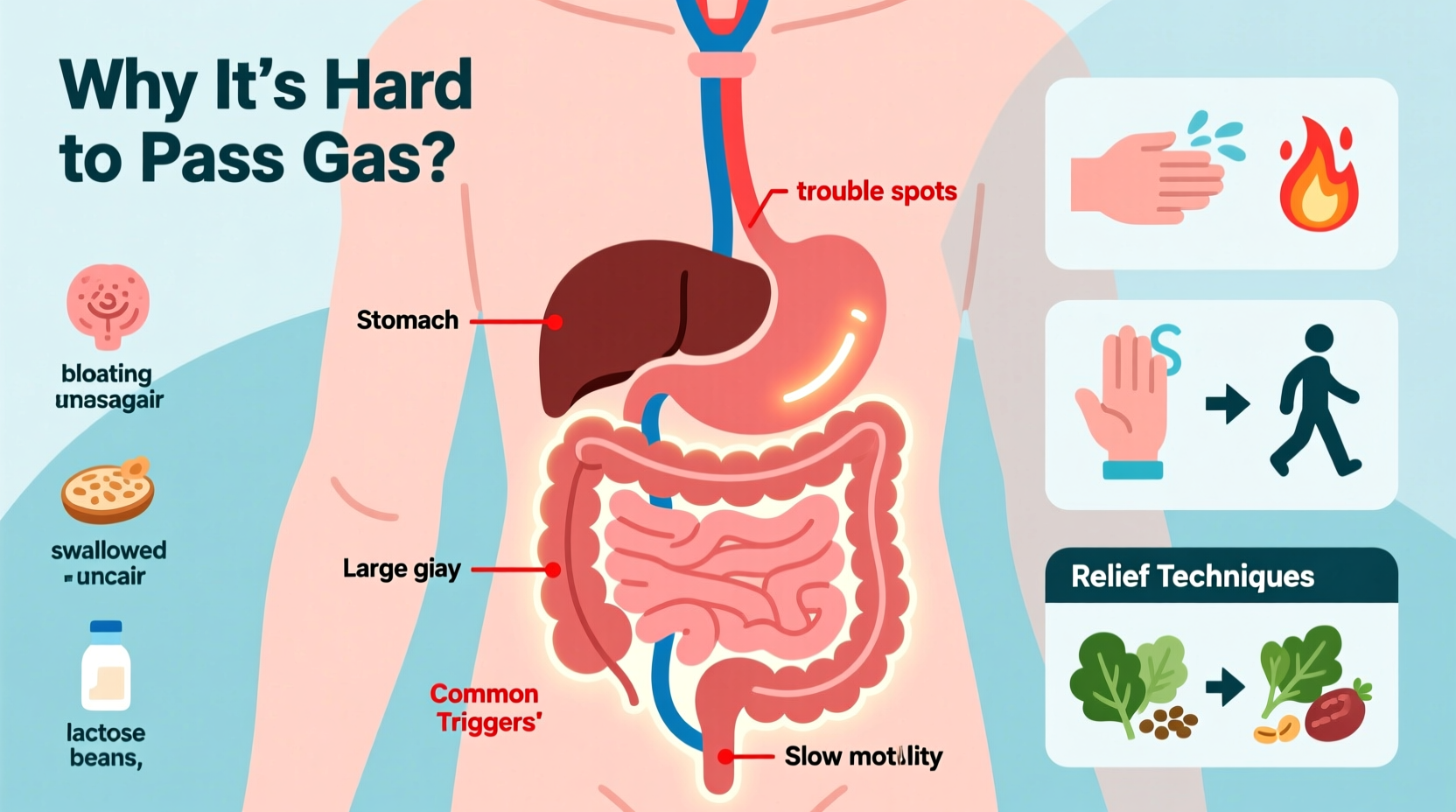
Intestinal gas comes from two main sources: swallowed air and bacterial fermentation in the colon. On average, a person passes gas 13 to 21 times per day. When gas accumulates but cannot escape, pressure builds in the intestines, leading to distension, pain, and a sensation of fullness.
Several physiological factors influence whether gas moves smoothly through the digestive tract:
- Peristalsis: The wave-like muscle contractions that move food and gas through the intestines. Slowed peristalsis delays gas transit.
- Sphincter control: The anal sphincter must relax appropriately to allow gas to pass. Nervous tension or pelvic floor disorders can inhibit this reflex.
- Posture: Sitting for long periods compresses the abdomen, making it harder for gas to rise and exit.
- Dietary triggers: Foods high in fermentable carbohydrates (FODMAPs) produce excess gas, increasing volume and pressure.
“Many patients come in worried about heart or stomach issues, only to discover their real problem is unresolved gas due to poor motility or pelvic floor tension.” — Dr. Lena Patel, Gastroenterologist
Why It’s Hard to Fart: Common Causes
Difficulty passing gas isn't usually dangerous, but identifying the root cause is key to relief. Below are the most frequent contributors:
- Constipation: Stool buildup blocks the path for gas, causing it to pool behind hardened fecal matter.
- Pelvic Floor Dysfunction: Some people struggle to coordinate the muscles needed to release gas. This is especially common after childbirth or in those with chronic straining.
- Irritable Bowel Syndrome (IBS): IBS often involves abnormal gut motility and visceral hypersensitivity, making gas both more painful and harder to expel.
- Swallowed Air (Aerophagia): Rapid eating, chewing gum, or carbonated drinks introduce excess air into the digestive system.
- Post-Surgical Recovery: Abdominal surgeries temporarily slow gut motility, leading to post-op gas pain known as “postoperative ileus.”
- Stress and Anxiety: The gut-brain axis means emotional tension can tighten abdominal muscles and disrupt normal gas passage.
How to Relieve Gas: A Step-by-Step Guide
Natural, immediate strategies can help release trapped gas and prevent future episodes. Follow this sequence for best results:
- Change Your Position: Move from sitting to standing or lying in the fetal position. Gentle rocking or knee-to-chest stretches can encourage gas movement.
- Apply Heat: Place a heating pad on your abdomen for 15–20 minutes. Heat relaxes intestinal muscles and eases spasms.
- Massage Your Abdomen: Use firm, clockwise motions starting near the right hip bone, moving up, across, and down toward the left groin—following the path of the colon.
- Sip Warm Liquids: Herbal teas like peppermint or ginger stimulate digestion and reduce gas-related cramping.
- Try Over-the-Counter Aids: Simethicone (found in Gas-X) breaks up gas bubbles, while activated charcoal may absorb excess gas (use cautiously).
- Use a Rectal Tube or Suppository (if chronic): In severe cases, doctors may recommend short-term use of rectal devices to vent gas.
Long-Term Prevention Strategies
Preventing gas retention requires consistent lifestyle habits. Consider these adjustments:
| Strategy | Action | Expected Benefit |
|---|---|---|
| Diet Modification | Reduce high-FODMAP foods (onions, beans, dairy, apples) | Lowers gas production at the source |
| Eat Slowly | Chew thoroughly, avoid talking while eating | Reduces swallowed air |
| Stay Active | Walk daily, avoid prolonged sitting | Encourages intestinal motility |
| Hydration | Drink 6–8 glasses of water daily | Prevents constipation-related blockage |
| Probiotics | Consume fermented foods or supplements | Balances gut bacteria to improve digestion |
Mini Case Study: Recovering from Post-Surgical Gas Pain
Sarah, a 42-year-old office worker, underwent laparoscopic gallbladder surgery. In the days following, she experienced severe bloating and an inability to pass gas, despite feeling intensely gassy. Her surgeon explained that anesthesia and abdominal inflation during surgery had temporarily paralyzed her bowel function.
Following medical advice, Sarah began gentle walking three times a day, drank warm lemon water, and applied a heating pad. By day three, she passed gas and felt immediate relief. She later incorporated daily abdominal massage and mindful eating to prevent recurrence during recovery.
This case highlights how temporary disruptions in gut function can cause significant gas retention—and how simple physical interventions often provide fast relief.
Checklist: What to Do When You Can’t Fart
- ✅ Stand up and walk for 5–10 minutes
- ✅ Lie on your left side with knees drawn to chest
- ✅ Apply a heating pad to lower abdomen
- ✅ Massage abdomen in clockwise motion
- ✅ Sip warm peppermint or chamomile tea
- ✅ Avoid carbonated drinks and gum
- ✅ Practice diaphragmatic breathing to relax pelvic floor
Frequently Asked Questions
Is it dangerous if I can’t fart?
Occasional difficulty passing gas is not dangerous, but persistent inability—especially with vomiting, fever, or severe pain—can indicate bowel obstruction and requires medical evaluation.
Can anxiety really stop me from farting?
Yes. Anxiety activates the sympathetic nervous system, which slows digestion and tenses pelvic floor muscles, making it physically harder to release gas. Mindfulness and breathing exercises can counteract this effect.
Are there exercises to help release gas?
Yes. Yoga poses like Child’s Pose, Seated Forward Bend, and Wind-Relieving Pose (Pavanamuktasana) apply gentle pressure to the abdomen and stimulate gas movement. Pelvic floor relaxation exercises also help if muscle tension is the issue.
When to See a Doctor
While most gas issues resolve with home care, seek medical attention if you experience:
- Severe or worsening abdominal pain
- Inability to pass stool or gas for over 24 hours
- Vomiting, fever, or blood in stool
- Unexplained weight loss or changes in bowel habits
These symptoms could signal conditions like intestinal obstruction, diverticulitis, or colorectal issues that require prompt diagnosis and treatment.
Conclusion: Take Control of Your Digestive Comfort
Struggling to fart is more than just awkward—it can be physically distressing and emotionally draining. But with the right knowledge, most people can find quick relief and long-term prevention. From adjusting posture and diet to understanding the role of stress and gut health, small changes make a big difference.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?