Many people experience sudden muscle twitches just as they're drifting off to sleep—brief, involuntary jolts that can feel like falling or a startled jump. These sensations, commonly known as \"hypnic jerks,\" are widespread and usually harmless. Yet for some, they raise concerns about underlying health issues. Understanding the science behind these twitches, what triggers them, and when they might signal something more serious is essential for peace of mind and better sleep hygiene.
The Science Behind Sleep Twitches
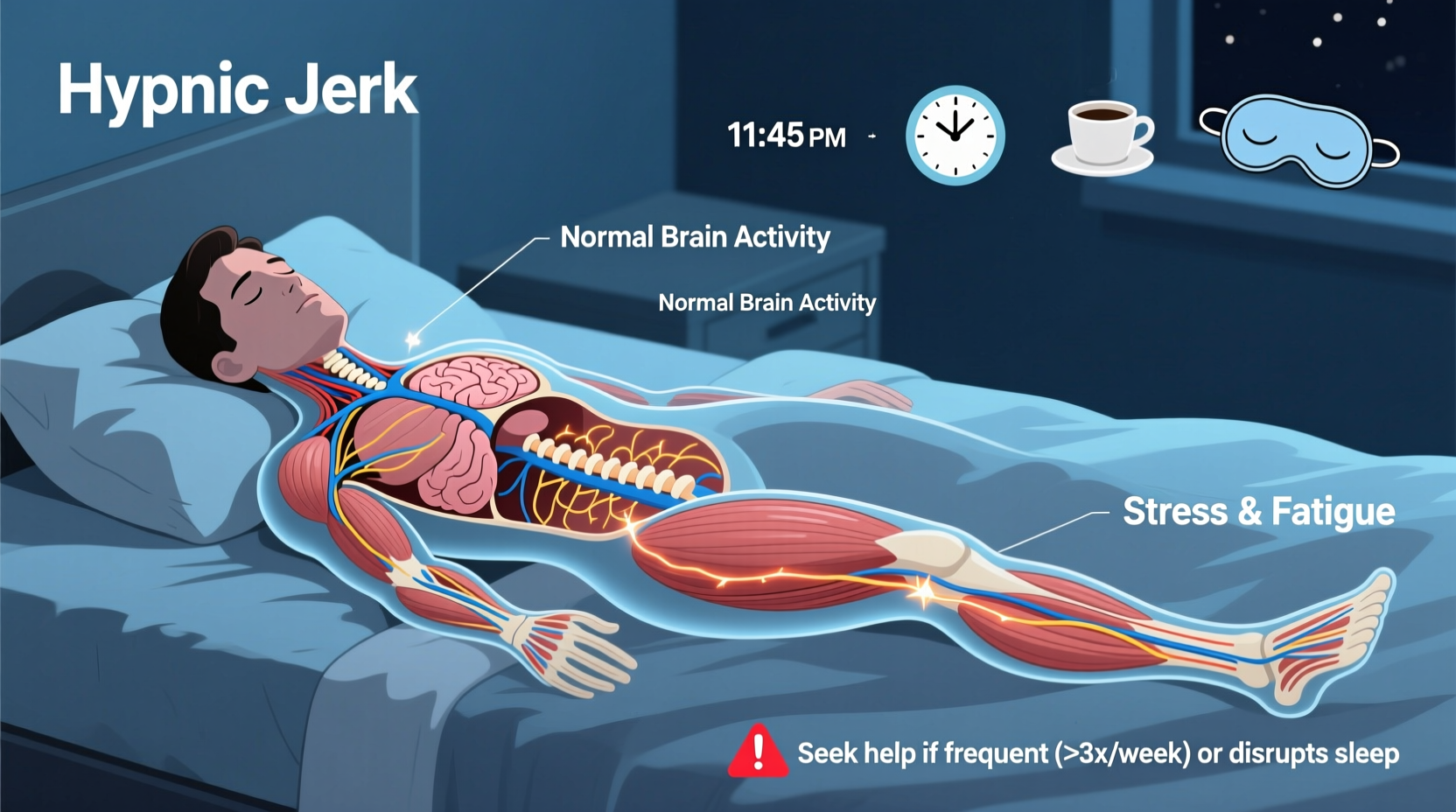
Hypnic jerks, or sleep starts, occur during the transition from wakefulness to sleep—specifically in the hypnagogic state. This phase marks the beginning of non-REM (NREM) sleep, when brain activity slows down and the body begins to relax. During this shift, the nervous system may misinterpret muscle relaxation as a sign of falling, triggering a reflexive contraction to “catch” yourself. This evolutionary response may have roots in our primate ancestors, who needed to stay alert to prevent falling from trees while resting.
Neurologically, the reticular activating system and motor cortex remain partially active during this transition. As signals from the brain to the muscles change, occasional misfiring can result in a sudden jerk—most often in the legs, arms, or whole body. These twitches are typically accompanied by a brief mental image, such as falling or tripping, which reinforces the sensation.
“Hypnic jerks are a normal part of the sleep initiation process for most people. They reflect the brain’s dynamic recalibration as it shifts from alertness to rest.” — Dr. Lena Torres, Neurologist & Sleep Specialist
Common Triggers of Pre-Sleep Twitching
While hypnic jerks are a natural phenomenon, certain lifestyle and physiological factors can increase their frequency or intensity:
- Stress and anxiety: Elevated cortisol levels keep the nervous system on high alert, making it harder for the brain to fully disengage from wakefulness.
- Caffeine intake: Consuming coffee, tea, or energy drinks late in the day stimulates the central nervous system and delays the calming process needed for sleep onset.
- Physical exertion close to bedtime: Intense exercise raises core body temperature and adrenaline, disrupting the smooth transition into sleep.
- Sleep deprivation: When severely tired, the brain enters deep sleep more abruptly, increasing the likelihood of neural misfires.
- Uncomfortable sleeping environment: Noise, light, or an unsupportive mattress can create micro-arousals that trigger muscle responses.
When Twitching Is Normal vs. When to Be Concerned
Occasional twitches at sleep onset are considered normal and affect up to 70% of the population. However, there are specific red flags that suggest the twitching may be linked to a neurological or sleep disorder rather than benign hypnic jerks.
| Normal Twitching | Potentially Concerning Signs |
|---|---|
| Occurs only at sleep onset | Happens multiple times throughout the night |
| Single, isolated jerk | Repetitive or rhythmic muscle contractions |
| No pain or lasting discomfort | Pain, cramping, or soreness afterward |
| Does not disrupt overall sleep quality | Frequent awakenings or fear of falling asleep |
| No associated dreams or hallucinations | Vivid imagery, sensory disturbances, or panic |
If twitching becomes frequent, painful, or interferes with your ability to fall asleep, it may indicate conditions such as restless legs syndrome (RLS), periodic limb movement disorder (PLMD), or even early signs of epilepsy. In rare cases, persistent myoclonus—a broader category of sudden muscle jerks—can be associated with neurological diseases.
Real-Life Example: Sarah’s Experience with Frequent Sleep Jerks
Sarah, a 34-year-old graphic designer, began noticing intense body jerks every night as she tried to sleep. Initially, she dismissed them as stress-related, but over time, the twitches became so frequent that she started dreading bedtime. She often woke up with sore shoulders and described feeling “electric shocks” in her legs. After weeks of disrupted sleep, she consulted a sleep specialist.
Her sleep study revealed no seizures or PLMD, but high cortisol levels and poor sleep hygiene were contributing factors. She was consuming energy drinks during late work hours and sleeping in a brightly lit room. With adjustments—eliminating stimulants, practicing mindfulness, and optimizing her bedroom environment—her symptoms reduced significantly within three weeks. Her case highlights how lifestyle choices can amplify a normally benign condition into a disruptive one.
Step-by-Step Guide to Reducing Sleep Twitches
For most people, improving sleep habits can dramatically reduce the frequency and intensity of pre-sleep twitches. Follow this five-step approach:
- Establish a consistent sleep schedule: Go to bed and wake up at the same time every day, even on weekends, to regulate your circadian rhythm.
- Limit stimulants: Avoid caffeine, nicotine, and heavy meals at least 4–6 hours before bedtime.
- Create a wind-down routine: Spend 20–30 minutes doing calming activities like reading, stretching, or meditation to signal your body it’s time to rest.
- Optimize your sleep environment: Keep the room cool (60–67°F), dark, and quiet. Use blackout curtains and white noise if needed.
- Practice gentle evening exercise: Light yoga or walking can help release muscle tension without overstimulating the nervous system.
Checklist: Assess Your Risk for Problematic Twitching
Use this checklist to evaluate whether your sleep twitches warrant medical attention:
- ☑ Twitches occur more than once per night regularly
- ☑ You experience pain or muscle soreness afterward
- ☑ Twitching causes you to wake up frequently
- ☑ You feel anxious about falling asleep due to jerks
- ☑ Family history of epilepsy or movement disorders
- ☑ Twitches also happen during wakefulness or daytime naps
If three or more of these apply, consider scheduling a consultation with a neurologist or sleep specialist.
Frequently Asked Questions
Can dehydration cause twitching before sleep?
Yes. Low levels of electrolytes like magnesium, potassium, and calcium—often due to dehydration—can increase nerve excitability and lead to muscle spasms or twitches. Staying well-hydrated throughout the day, especially after exercise, helps maintain proper neuromuscular function.
Are hypnic jerks a sign of sleep paralysis?
No. While both occur during sleep transitions, they are different phenomena. Hypnic jerks happen as you’re falling asleep and involve physical movement. Sleep paralysis occurs upon waking (or rarely, while falling asleep) and involves temporary inability to move or speak, often accompanied by hallucinations. They share some risk factors but are distinct conditions.
Can children experience hypnic jerks?
Yes. Children and adolescents commonly experience sleep starts, sometimes more vividly than adults. Growth spurts, active imaginations, and irregular sleep schedules may contribute. As long as the twitches are infrequent and don’t disrupt sleep, they are generally not a cause for concern.
Conclusion: Listen to Your Body, Prioritize Rest
Twitching before sleep is a common, usually harmless event rooted in the complex biology of transitioning into rest. For the vast majority, simple lifestyle adjustments are enough to minimize discomfort and improve sleep quality. But when twitches become frequent, painful, or anxiety-inducing, they should not be ignored. Pay attention to patterns, track changes, and don’t hesitate to seek professional guidance if needed.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?