Testicular atrophy—the shrinking of the testicles—is a condition that affects many men, particularly those who have used anabolic steroids or experienced prolonged hormonal imbalances. While it can be distressing both physically and psychologically, there is a scientifically supported method for recovery: human chorionic gonadotropin (HCG). This hormone mimics luteinizing hormone (LH), stimulating testosterone production and helping restore testicular size and function. This guide provides a comprehensive, evidence-based look at how HCG works, when to use it, and how to implement it safely and effectively.
What Causes Testicular Atrophy?
Testicular atrophy occurs when the testes decrease in size due to suppressed natural testosterone production. The most common cause is exogenous testosterone use—such as in anabolic steroid cycles—which signals the brain to stop producing luteinizing hormone (LH) and follicle-stimulating hormone (FSH). Without these signals, the testes become dormant.
Other contributing factors include:
- Long-term use of testosterone replacement therapy (TRT)
- Hypogonadism (low hormone production)
- Pituitary disorders
- Chronic illness or malnutrition
- Alcohol abuse
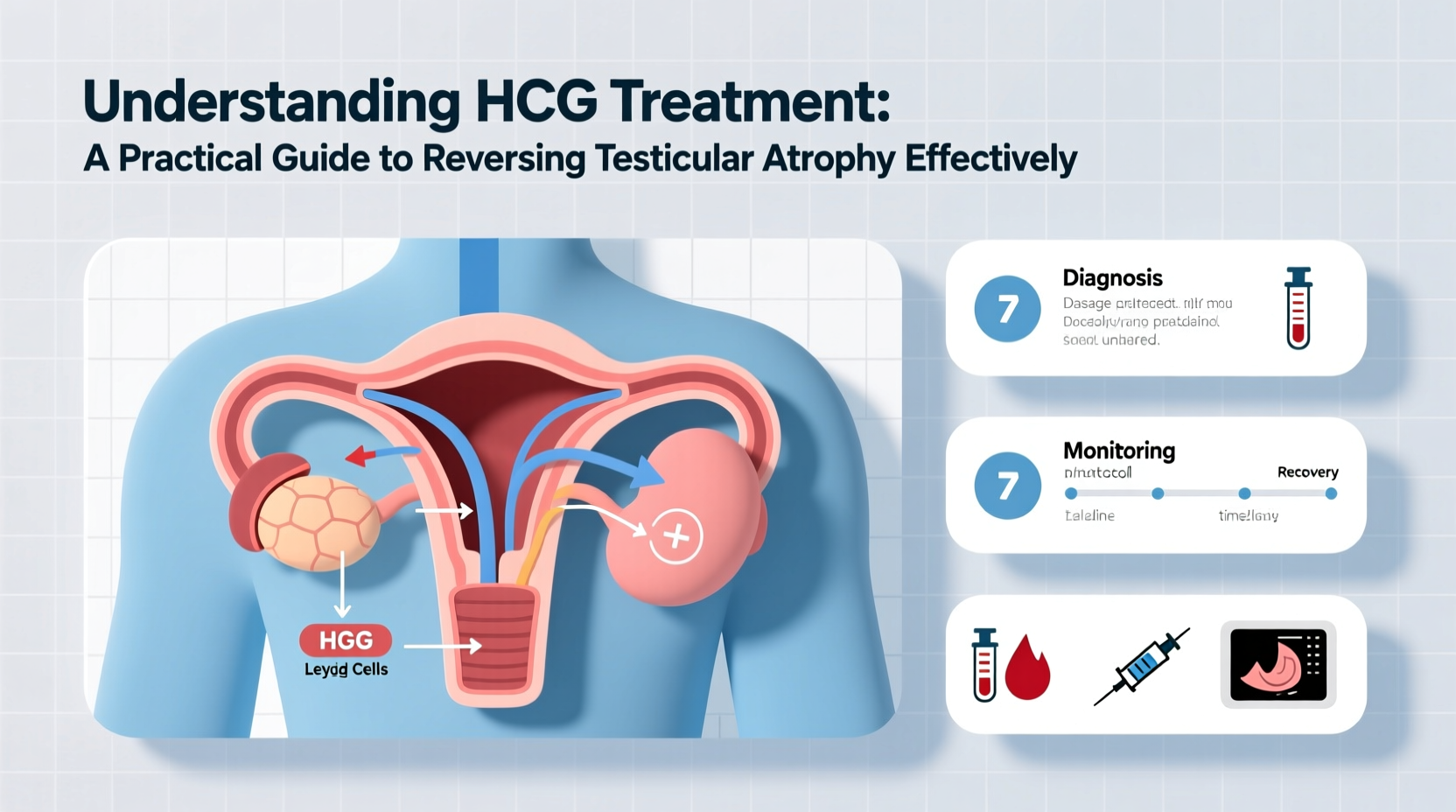
When LH levels drop, Leydig cells in the testes receive no stimulation, leading to reduced activity and shrinkage over time. The good news is that this process is often reversible with proper intervention.
How HCG Works to Reverse Atrophy
HCG is a glycoprotein hormone naturally produced during pregnancy, but it has powerful applications in male endocrinology. Structurally similar to LH, HCG binds to the same receptors on Leydig cells in the testes, prompting them to produce testosterone just as they would under normal physiological conditions.
By reintroducing this signal externally, HCG “tricks” the body into thinking LH is present, reactivating dormant testicular tissue. Over time, this can lead to:
- Increased intratesticular testosterone levels
- Restoration of testicular volume
- Improved spermatogenesis (sperm production)
- Enhanced fertility potential
“HCG is one of the most effective tools we have for preserving or restoring testicular function in men with secondary hypogonadism.” — Dr. Alan Morse, Endocrinologist & Men’s Health Specialist
Effective HCG Treatment Protocol
Using HCG effectively requires careful dosing, timing, and monitoring. Below is a step-by-step protocol commonly used by clinicians and informed users.
Step-by-Step HCG Treatment Timeline
- Week 1–2: Begin with 250–500 IU every other day via subcutaneous injection to assess tolerance.
- Week 3–8: Maintain 500 IU every other day. This phase typically shows measurable increases in testicular size.
- Week 9–12: Reassess progress via physical exam and blood work (total testosterone, estradiol, LH/FSH). Consider reducing frequency if goals are met.
- After 12 weeks: Taper usage gradually or discontinue if natural function resumes, especially post-cycle.
Dosing Guidelines by Use Case
| Purpose | Dose | Frequency | Duration |
|---|---|---|---|
| Post-cycle therapy (PCT) | 500 IU | Every other day | 3–6 weeks |
| TRT support | 250–500 IU | 2–3 times/week | Ongoing |
| Fertility enhancement | 1,000–2,000 IU | 2–3 times/week | 3–6 months |
| Atrophy reversal | 500 IU | Daily or EOD | 8–12 weeks |
Common Pitfalls and How to Avoid Them
While HCG is highly effective, improper use can lead to side effects or diminished results. Here are key mistakes to avoid:
- Overuse leading to desensitization: Continuous high-dose HCG may downregulate LH receptors, making the testes less responsive over time.
- Neglecting estrogen control: HCG increases testosterone, which can aromatize into estrogen. Unchecked, this may cause gynecomastia or water retention.
- Skipping bloodwork: Monitoring hormone levels ensures safety and effectiveness. Check total testosterone, estradiol, and gonadotropins before and during treatment.
- Stopping too soon: Some men see results in 4 weeks, but full recovery often takes 8–12 weeks. Patience is essential.
“Patients who combine HCG with proper nutrition, sleep, and stress management tend to recover faster and more completely.” — Dr. Lena Patel, Reproductive Endocrinologist
Real-World Example: Recovery After Long-Term TRT
James, a 42-year-old man, had been on testosterone replacement therapy for five years without any testicular support. He noticed significant shrinkage, low energy, and declining libido. His doctor recommended adding HCG at 250 IU three times per week while maintaining his TRT dose.
After six weeks, James reported improved testicular firmness and increased spontaneous erections. By week 10, ultrasound measurements showed a 35% increase in testicular volume. Blood tests confirmed elevated intratesticular testosterone and normalized estradiol with the addition of an aromatase inhibitor as needed.
This case illustrates that even long-standing atrophy can be reversed with consistent, well-managed HCG therapy.
Checklist: Starting HCG Safely and Effectively
- ✔ Consult a healthcare provider or endocrinologist before starting
- ✔ Get baseline blood work (testosterone, estradiol, LH, FSH, prolactin)
- ✔ Source pharmaceutical-grade HCG from a reputable pharmacy
- ✔ Learn proper injection technique (subcutaneous abdominal or thigh)
- ✔ Monitor for side effects (acne, mood changes, gynecomastia)
- ✔ Schedule follow-up blood tests at 6 and 12 weeks
- ✔ Combine with healthy lifestyle habits: strength training, quality sleep, and balanced diet
Frequently Asked Questions
Can HCG permanently reverse testicular atrophy?
In most cases of secondary hypogonadism, yes—especially when caught early and combined with lifestyle optimization. However, permanent damage is possible with very long-term suppression without intervention.
Will I need to stay on HCG forever?
Not necessarily. For post-cycle recovery, HCG is typically used short-term. In TRT patients, some choose ongoing low-dose HCG to preserve fertility and testicular health, but it’s not mandatory for all.
Does HCG affect fertility?
Yes—positively. HCG stimulates both testosterone and sperm production. It’s often used in fertility clinics to treat men with low sperm counts due to low gonadotropins.
Final Thoughts and Next Steps
Understanding HCG treatment is crucial for any man facing testicular atrophy due to steroid use, TRT, or hormonal dysfunction. With proper dosing, monitoring, and patience, HCG offers a proven path to restoring testicular size, boosting natural hormone production, and reclaiming reproductive health.
The journey back to optimal function begins with informed decisions. Whether you're recovering from a steroid cycle or managing long-term TRT, integrating HCG wisely can make a meaningful difference. Don’t navigate this alone—consult a qualified medical professional, get tested, and take control of your hormonal health today.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?