Glucagon-like peptide-1 (GLP-1) receptor agonists have emerged as powerful tools in managing type 2 diabetes and supporting weight loss. Medications like semaglutide (Ozempic, Wegovy), liraglutide (Victoza, Saxenda), and tirzepatide (Mounjaro, Zepbound) are increasingly prescribed due to their dual benefits on glycemic control and body weight. However, many patients wonder: when will I start seeing results? Understanding the timeline and what to expect can help set realistic goals and improve adherence.
How GLP-1 Medications Work
GLP-1 medications mimic the action of a naturally occurring hormone that regulates insulin secretion, slows gastric emptying, and reduces appetite. By activating GLP-1 receptors, these drugs help lower blood glucose levels after meals and promote a feeling of fullness, which often leads to reduced calorie intake.
Unlike fast-acting insulin or oral hypoglycemics, GLP-1 agonists work gradually. Their effects build over time, both in terms of glucose control and weight reduction. This slow onset is by design—most regimens start at a low dose to minimize gastrointestinal side effects and are titrated upward over several weeks.
The Typical Timeline for Results
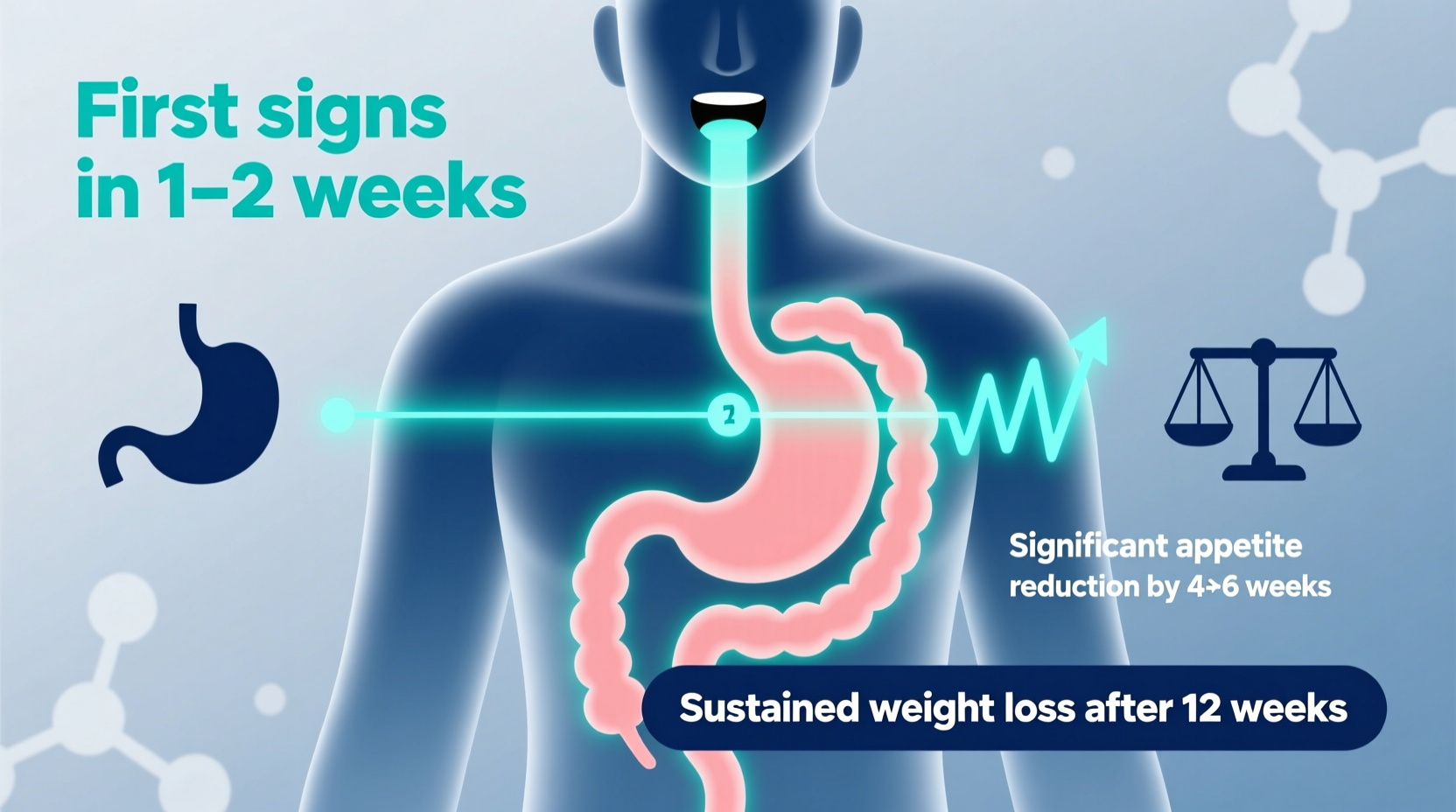
Response times vary depending on the specific medication, dosage, individual metabolism, and treatment goals. However, most patients follow a predictable pattern:
- Weeks 1–4: Initial adjustment phase. Patients may notice reduced appetite and mild nausea. Blood sugar improvements can begin within the first few weeks, especially in those with elevated baseline glucose.
- Weeks 5–12: Early weight loss becomes apparent—typically 3–5% of body weight. Fasting glucose and HbA1c levels continue to decline.
- Months 3–6: Most people reach their maintenance dose and experience steady weight loss, averaging 5–10% of body weight. Many report improved energy, better hunger control, and noticeable changes in clothing fit.
- Month 6 and beyond: Continued gradual weight loss up to 15–20% over a year in clinical trials. Metabolic markers stabilize, and cardiovascular risk factors often improve.
What to Expect During Treatment
While the primary outcomes are weight reduction and improved glycemic control, patients also experience secondary effects—some welcome, others less so. Being prepared helps manage expectations and maintain motivation.
Positive Changes
- Reduced hunger and fewer cravings, particularly for sugary or high-carb foods
- Better post-meal blood sugar stability
- Gradual but consistent weight loss, especially around the abdomen
- Improved mood and energy levels as metabolic health improves
- Potential reduction in blood pressure and triglycerides
Common Side Effects
The most frequent side effects are gastrointestinal and typically occur during dose escalation:
- Nausea (most common, usually mild and temporary)
- Constipation or diarrhea
- Occasional vomiting or bloating
- Decreased appetite (often beneficial, but can lead to inadequate nutrition if not managed)
These symptoms usually subside within a few weeks as the body adjusts. Taking the medication at bedtime, eating smaller meals, and avoiding high-fat foods initially can reduce discomfort.
Factors That Influence Response Time
Not everyone responds at the same pace. Several variables affect how quickly and effectively GLP-1 medications work:
| Factor | Impact on Response Time |
|---|---|
| Dosage and Titration Schedule | Slower titration delays full effect but reduces side effects; faster escalation may speed results but increases GI risk. |
| Baseline Weight and Insulin Resistance | Higher starting weight may lead to more rapid initial loss; severe insulin resistance may blunt early response. |
| Diet and Physical Activity | Calorie deficit and regular movement enhance weight loss and glucose improvements. |
| Medication Type | Tirzepatide (dual GIP/GLP-1 agonist) tends to produce faster, greater weight loss than semaglutide in head-to-head trials. |
| Adherence | Missed doses delay progress and reduce efficacy. |
“Patients who combine GLP-1 therapy with lifestyle changes see twice the weight loss and three times the improvement in insulin sensitivity compared to medication alone.” — Dr. Rachel Nguyen, Endocrinologist and Obesity Specialist
Step-by-Step Guide: Maximizing Your Results Over 6 Months
To get the most from your treatment, follow this structured approach:
- Month 1: Focus on Adaptation
Start at the prescribed low dose. Track side effects and eating patterns. Stay hydrated and eat small, balanced meals. - Month 2: Monitor Early Changes
Check fasting glucose if diabetic. Weigh yourself weekly. Begin light physical activity like walking 30 minutes daily. - Month 3: Assess Progress
Review results with your provider. Adjust dose if needed. Evaluate hunger cues and identify sustainable eating habits. - Months 4–6: Optimize Lifestyle
Incorporate strength training, increase protein intake, and refine portion control. Address any plateaus with dietary review. - Month 6+: Maintain and Reassess
Discuss long-term plans. Consider body composition testing. Evaluate whether goals have been met and next steps.
Realistic Expectations: A Mini Case Study
Sarah, a 47-year-old woman with prediabetes and a BMI of 32, started on semaglutide 0.25 mg weekly. In the first two weeks, she experienced mild nausea and skipped one dose. After adjusting her meal timing and switching injection nights, symptoms improved.
By week 6, her fasting glucose dropped from 115 mg/dL to 98 mg/dL. She lost 4 pounds in the first month and another 6 by week 12. At six months, she reached her maintenance dose and had lost 18 pounds—about 9% of her body weight. She reported wearing smaller clothes and no longer needing afternoon snacks.
Her success was supported by walking 4 days a week and reducing processed carbohydrates. Her provider emphasized that while progress wasn’t linear, consistency made the difference.
FAQ
Can I see results in the first week?
Some people notice reduced appetite within days, but measurable weight loss or blood sugar changes typically take 3–4 weeks. Rapid results are uncommon and not necessary for long-term success.
What if I don’t lose weight after two months?
Several factors could be at play: incorrect dosing, insufficient calorie deficit, underlying hormonal issues, or poor adherence. Discuss concerns with your provider before making changes.
Do GLP-1 medications stop working over time?
No evidence suggests tolerance develops. However, some patients plateau around 6–8 months. This is normal and often addressed through lifestyle refinement rather than medication change.
Action Plan Checklist
Use this checklist to stay on track during your first six months:
- ✅ Take medication consistently on the same day each week
- ✅ Attend all follow-up appointments for dose adjustments
- ✅ Drink plenty of water to manage constipation
- ✅ Eat protein-rich, fiber-filled meals to support satiety
- ✅ Walk or move for at least 20–30 minutes most days
- ✅ Track weight and symptoms weekly
- ✅ Communicate side effects or concerns to your healthcare team
- ✅ Avoid alcohol and greasy foods during dose escalation
Conclusion
GLP-1 medications are not quick fixes—they are tools that require patience, consistency, and lifestyle integration. Most people begin to feel and see changes within 4 to 12 weeks, with optimal results unfolding over 6 to 12 months. The journey involves adaptation, monitoring, and ongoing support.
Success isn’t measured solely by the scale but by improved energy, better lab results, and enhanced quality of life. If you’re starting or already on a GLP-1 regimen, trust the process, stay engaged with your care team, and make sustainable choices every day.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?