Melanoma is the most aggressive form of skin cancer, known for its potential to spread rapidly if not detected early. Unlike other skin cancers, melanoma arises from melanocytes—the pigment-producing cells in the skin—and can develop in areas not typically exposed to sunlight. The speed at which melanoma grows varies significantly between individuals, influenced by a complex interplay of biological, environmental, and behavioral factors. Understanding what accelerates melanoma development is crucial for prevention, early diagnosis, and effective treatment.
Genetic Predisposition and Family History
One of the strongest predictors of rapid melanoma development is genetic susceptibility. Individuals with a family history of melanoma are at increased risk due to inherited gene mutations such as CDKN2A or BAP1. These mutations impair the body’s ability to regulate cell division and repair DNA damage, allowing abnormal cells to proliferate unchecked.
People with certain genetic traits—such as fair skin, red or blonde hair, blue eyes, and a tendency to burn rather than tan—are more vulnerable to UV-induced DNA damage, which can initiate melanoma. Additionally, those with a high number of moles (especially atypical or dysplastic nevi) face a higher baseline risk, as these lesions can undergo malignant transformation over time.
“Approximately 10% of melanoma patients have a family history of the disease, indicating a significant hereditary component.” — Dr. Rebecca Tan, Dermatology Oncologist, Mayo Clinic
UV Radiation Exposure: The Primary Environmental Trigger
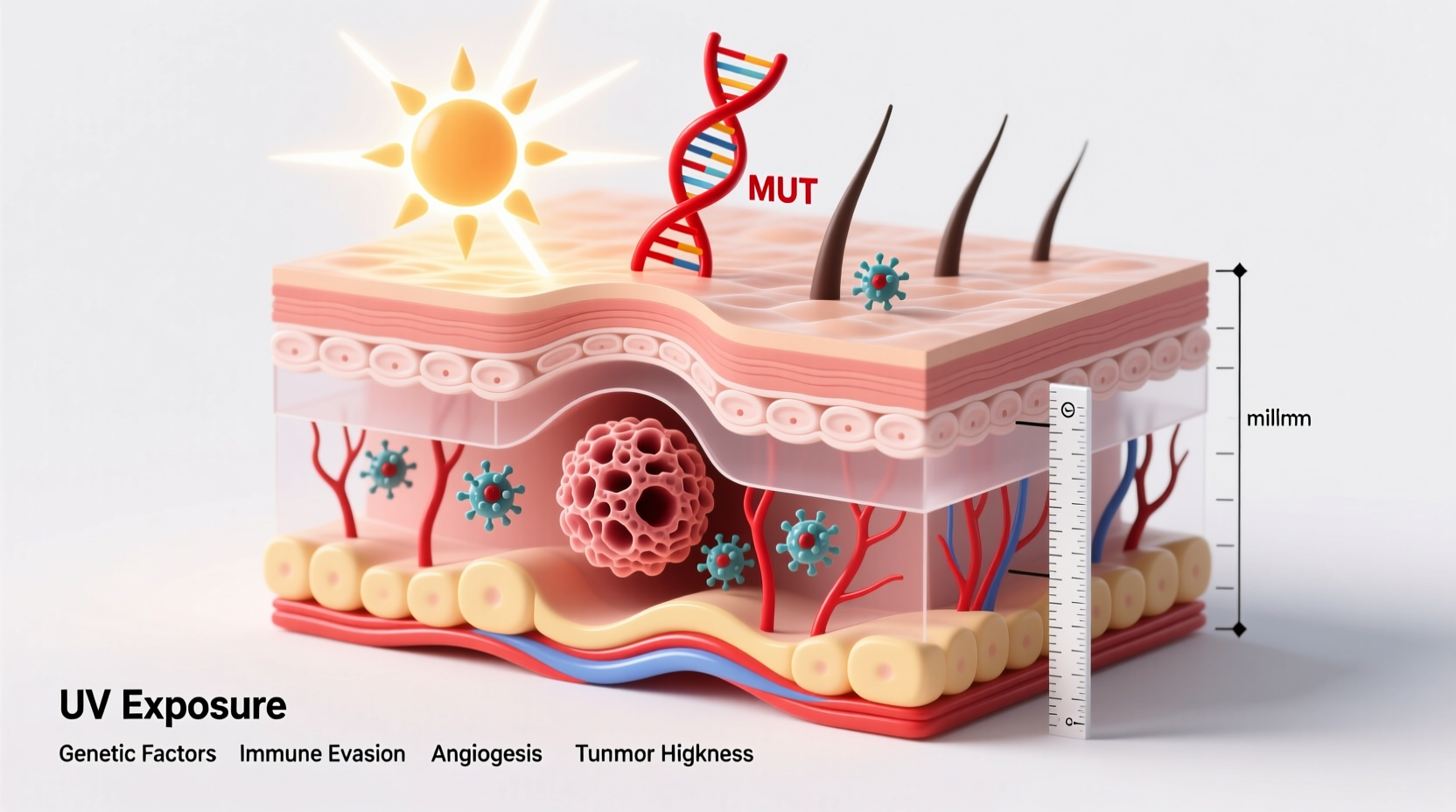
Ultraviolet (UV) radiation—both from natural sunlight and artificial sources like tanning beds—is the leading environmental factor driving melanoma initiation and progression. UVB rays directly damage DNA in skin cells, causing mutations in critical genes like BRAF and NRAS, which are found in up to 70% of melanoma cases.
Intermittent, intense sun exposure—such as weekend sunbathing or vacation-related burns—is particularly dangerous. This pattern leads to sudden DNA stress that overwhelms repair mechanisms. In contrast, chronic daily exposure may lead to slower-developing skin cancers but still contributes to cumulative skin damage that increases melanoma risk over time.
Tanning bed use before age 35 increases melanoma risk by 75%, according to the World Health Organization. The concentrated UVA radiation in tanning devices penetrates deeply into the dermis, generating free radicals and suppressing local immune surveillance, creating an environment conducive to tumor growth.
Types of UV Exposure and Their Impact on Melanoma Risk
| Type of Exposure | Description | Associated Risk Level |
|---|---|---|
| Intermittent Intense | Sudden, high-dose exposure (e.g., sunburns) | High – strongly linked to early-onset melanoma |
| Chronic Cumulative | Daily, long-term exposure (e.g., outdoor work) | Moderate – associated with slower-growing subtypes |
| Artificial UV | Tanning bed use | Very High – doubles risk with regular use |
Biological Factors Influencing Growth Rate
The speed of melanoma progression depends heavily on the tumor’s biological characteristics. Some melanomas grow slowly over years (e.g., lentigo maligna melanoma), while others—like nodular melanoma—can advance deeply within weeks.
- BRAF Mutations: Present in about half of all melanomas, BRAF V600E mutations drive rapid cell division and are often found in younger patients with trunk or limb tumors.
- Tumor Thickness (Breslow Depth): Measured in millimeters, this is one of the strongest prognostic indicators. Tumors thicker than 1 mm grow faster and metastasize earlier.
- Immune System Function: A robust immune response can slow melanoma progression. Immunosuppressed individuals (e.g., organ transplant recipients) face a 2–3 times higher risk of aggressive disease.
The microenvironment surrounding the tumor also plays a role. Inflammation, angiogenesis (formation of new blood vessels), and immune evasion mechanisms allow melanoma cells to thrive and spread. For example, tumors that express PD-L1 protein can deactivate T-cells, effectively hiding from the immune system.
Step-by-Step Guide to Early Detection and Monitoring
Catching melanoma early dramatically improves outcomes. When localized, the five-year survival rate exceeds 99%. However, once it spreads to lymph nodes or distant organs, survival drops sharply. Follow this timeline to stay proactive:
- Monthly Self-Exams: Use mirrors or a partner to inspect hard-to-see areas. Focus on changes in size, shape, color, or texture of moles.
- Follow the ABCDE Rule:
- A – Asymmetry: One half doesn’t match the other.
- B – Border irregularity: Edges are ragged or blurred.
- C – Color variation: Multiple shades of brown, black, red, or white.
- D – Diameter: Larger than 6 mm (pencil eraser).
- E – Evolution: Any change over time.
- Annual Dermatologist Visit: Professional skin exams using dermoscopy can detect subtle changes invisible to the naked eye.
- Dermoscopic Imaging: For high-risk patients, clinics may use total-body photography and digital monitoring to track mole changes over months.
- Biopsy Suspicious Lesions: Prompt removal and histopathological analysis confirm diagnosis and determine depth and mitotic rate.
Real-World Example: Rapid Onset in a Young Adult
James, a 28-year-old software developer, noticed a small dark spot on his upper back that appeared suddenly after a beach vacation. Initially dismissing it as a new freckle, he returned six weeks later to find it had grown, bled slightly, and developed uneven borders. A dermatologist performed a biopsy, revealing nodular melanoma with a Breslow depth of 2.3 mm—already in stage IIB.
Despite no family history, James had experienced multiple blistering sunburns during childhood and used tanning beds occasionally in college. His case highlights how intermittent UV exposure combined with delayed self-detection can result in fast-progressing melanoma—even in young, otherwise healthy individuals.
Actionable Prevention Checklist
Reducing melanoma risk isn’t just about sunscreen—it requires a comprehensive approach. Use this checklist to protect yourself and your family:
- ✅ Apply broad-spectrum SPF 30+ sunscreen every day, even when cloudy
- ✅ Reapply sunscreen every two hours during outdoor activity
- ✅ Wear UV-protective clothing, wide-brimmed hats, and sunglasses
- ✅ Avoid peak sun hours (10 a.m. to 4 p.m.) whenever possible
- ✅ Never use indoor tanning beds
- ✅ Perform monthly skin self-exams using full-length and hand mirrors
- ✅ Schedule annual skin checks with a board-certified dermatologist
- ✅ Document moles with photos to monitor changes over time
Frequently Asked Questions
How fast can melanoma spread?
Some types of melanoma, especially nodular melanoma, can become invasive within weeks. Other forms may take months or years to progress. The average doubling time for melanoma cells ranges from 30 to 100 days, depending on subtype and individual biology.
Can melanoma appear overnight?
While it doesn’t literally appear overnight, some melanomas—particularly nodular types—can seem to emerge suddenly because they grow vertically from the start, making them noticeable quickly. What appears to be a new mole could actually be a rapidly evolving tumor.
Is melanoma always caused by sun exposure?
No. While UV radiation is a major contributor, melanoma can occur in areas with little to no sun exposure, such as the soles of feet, palms, or under nails (acral lentiginous melanoma). Genetic factors, immune status, and random mutations also play significant roles.
Conclusion: Take Control Before It Spreads
Understanding the factors that influence melanoma growth empowers individuals to act before cancer advances. Genetics and UV exposure set the stage, but personal vigilance determines the outcome. Regular skin checks, sun-safe behaviors, and prompt medical evaluation of changing lesions are non-negotiable steps in preventing life-threatening progression.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?