The human circulatory system is a marvel of biological engineering, designed to transport blood efficiently throughout the body. At the heart of this system are two major types of blood vessels: arteries and veins. While both carry blood, they do so under vastly different conditions and with distinct anatomical features. One of the most notable differences is that veins contain valves—small, flap-like structures—while arteries do not. Understanding why valves exist only in veins requires a deep dive into pressure dynamics, anatomy, and physiology.
Anatomical and Functional Differences Between Arteries and Veins
Arteries and veins serve opposite roles in circulation. Arteries carry oxygenated blood away from the heart (except for the pulmonary artery), while veins return deoxygenated blood back to the heart (except for the pulmonary vein). This fundamental difference sets the stage for their structural divergence.
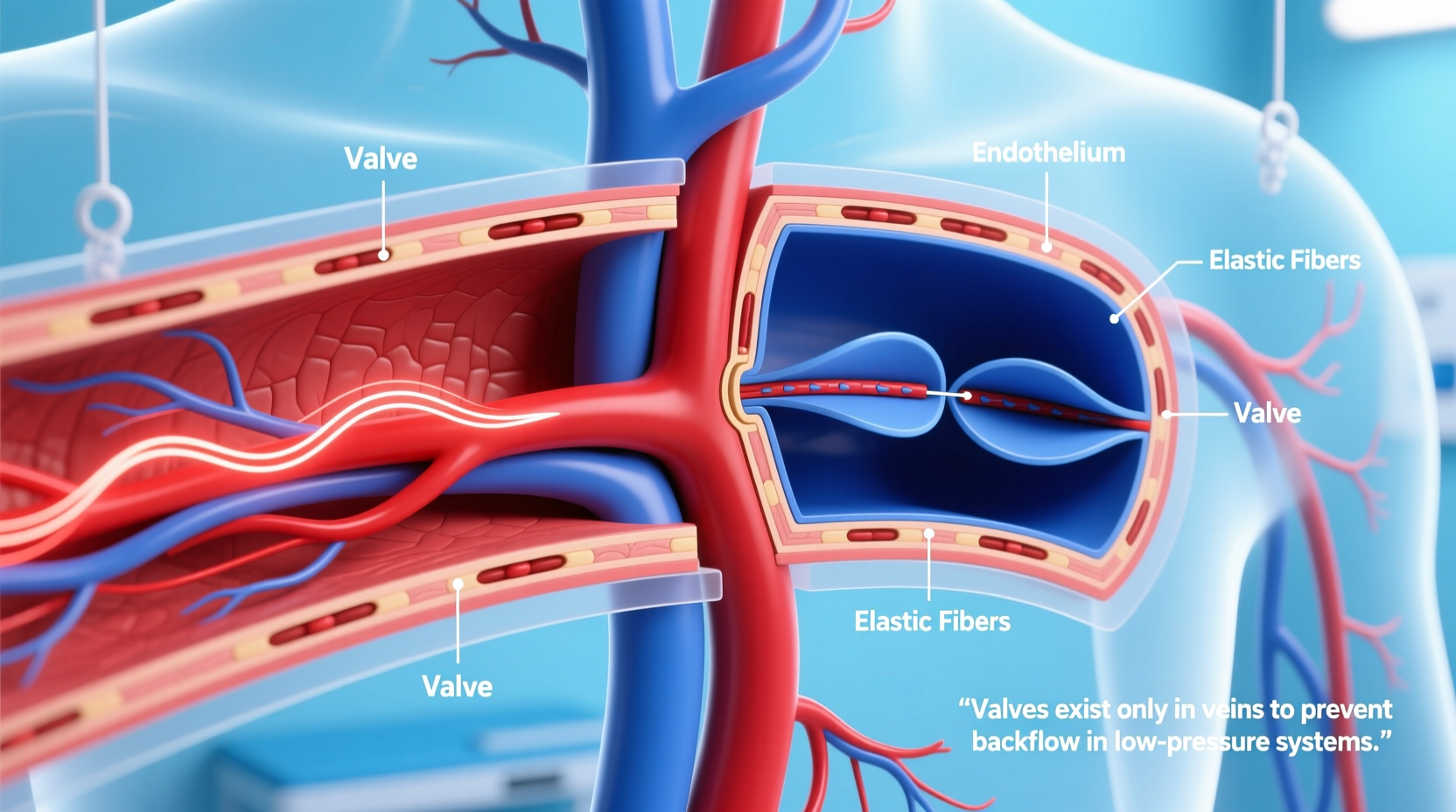
Arteries are built to withstand high pressure. The blood ejected from the left ventricle of the heart enters the aorta at pressures averaging 120 mmHg during systole. To handle this force, arteries have thick, muscular, and elastic walls. These layers allow them to expand with each heartbeat and recoil to maintain continuous forward flow—a phenomenon known as the Windkessel effect.
In contrast, veins operate under much lower pressure. By the time blood reaches the venous system, after passing through capillaries and arterioles, pressure has dropped significantly—often to less than 10 mmHg. Their walls are thinner and less muscular, making them more compliant and capable of holding a larger volume of blood. In fact, about 70% of the body’s blood volume resides in the venous system at any given time, earning veins the nickname “capacitance vessels.”
Why Valves Are Necessary in Veins
Because veins operate under low pressure, they face a critical challenge: gravity. When blood travels upward from the legs and feet toward the heart, it must overcome gravitational pull. Without assistance, blood would pool in the lower extremities, leading to swelling, reduced cardiac output, and tissue damage.
This is where valves come in. Venous valves are small, bicuspid (two-cusped) flaps made of endothelial tissue that open to allow blood to flow toward the heart and close to prevent backflow. They are especially abundant in the deep veins of the legs, where the risk of retrograde flow is highest.
The mechanism relies on muscle contractions. When leg muscles contract during walking or movement, they compress the veins, pushing blood upward. The valves ensure this motion translates into unidirectional flow. Once the muscle relaxes, the pressure drops, and the valve snaps shut, preventing blood from slipping backward.
“Venous valves act like one-way gates in a river system—they keep the flow moving toward the heart even when external forces try to reverse it.” — Dr. Alan Reyes, Vascular Physiologist
Why Don’t Arteries Need Valves?
The answer lies in pressure. Arterial blood flow is driven directly by the forceful contractions of the heart. Each heartbeat generates enough pressure to propel blood through the arterial tree without relying on secondary mechanisms like muscle pumps or valves.
Additionally, the elasticity of arterial walls helps maintain forward momentum during diastole (the relaxation phase of the heartbeat), smoothing out pulsatile flow and ensuring continuity. Because arterial pressure is consistently high—especially in systemic arteries—there is minimal risk of backflow under normal conditions.
Even in upright positions, arterial pressure remains sufficient to overcome gravity. For example, blood reaching the brain via the carotid arteries does so against gravity, yet no valves are needed because systolic pressure easily exceeds gravitational resistance.
Comparative Overview: Arteries vs. Veins
| Feature | Arteries | Veins |
|---|---|---|
| Blood Pressure | High (80–120 mmHg) | Low (5–10 mmHg) |
| Wall Thickness | Thick, muscular | Thin, less elastic |
| Lumen Size | Smaller, round | Larger, often collapsed |
| Valves Present? | No | Yes (especially in limbs) |
| Primary Function | Carry blood away from heart | Return blood to heart |
| Volume Capacity | Low (20% of blood volume) | High (70% of blood volume) |
Clinical Insight: What Happens When Valves Fail?
A real-world example illustrates the importance of venous valves. Consider Maria, a 48-year-old nurse who spends most of her 12-hour shifts standing. Over time, she begins to notice swelling and aching in her calves, along with visible blue, twisted cords beneath her skin—classic signs of varicose veins.
Upon examination, her physician explains that prolonged standing has increased venous pressure in her legs. This constant strain weakened the valves in her superficial veins, causing them to become incompetent. Instead of closing tightly, they now allow blood to reflux downward, pooling in the lower limbs. The resulting distension damages vein walls and leads to chronic discomfort.
Maria’s case highlights a key point: valves are essential for maintaining venous return under low-pressure conditions. When they fail, the entire circulatory efficiency declines. Treatment includes compression stockings, lifestyle changes, and sometimes surgical intervention to remove damaged veins.
Step-by-Step: How Blood Returns to the Heart from the Legs
- Deoxygenated blood enters the capillaries in the foot and gradually moves into small venules.
- Venules merge into larger superficial and deep veins in the leg.
- As leg muscles contract during walking, they compress the veins, squeezing blood upward.
- Blood passes through an open venous valve, moving closer to the heart.
- When the muscle relaxes, pressure drops, and the valve closes behind the blood, preventing backflow.
- This process repeats with each step, creating the “muscle pump” effect.
- Blood eventually reaches the inferior vena cava and returns to the right atrium of the heart.
Frequently Asked Questions
Can arteries ever develop valves?
No, arteries do not naturally have valves. However, in rare congenital conditions or pathological states, abnormal tissue formations may resemble valves, but these are not functional in the same way as venous valves and can impede flow.
Are there any veins without valves?
Yes. Not all veins contain valves. For example, the large central veins like the superior and inferior vena cava, as well as cerebral veins, typically lack valves. Their proximity to the heart and relatively straight path reduce the risk of backflow.
What happens if you stand still for too long?
Standing motionless reduces muscle pump activity, allowing blood to pool in the legs due to gravity. This can lead to dizziness or fainting (vasovagal syncope) in some people, as less blood returns to the heart, reducing cardiac output temporarily.
Conclusion: Respecting the Design of Circulation
The absence of valves in arteries and their presence in veins is not arbitrary—it’s a precise adaptation to the physics of blood flow. Arteries rely on high pressure and elastic recoil; veins depend on valves and external muscle action to complete their journey. Recognizing this balance enhances our appreciation of cardiovascular health and underscores the importance of movement, posture, and circulation support.
Whether you're on your feet all day or sitting at a desk, understanding how your veins work empowers you to make better choices. Stay active, avoid prolonged immobility, and listen to your body’s signals. Your circulatory system is working tirelessly—give it the support it deserves.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?