Occasional sensations of vibration in the foot are more common than many realize. Often dismissed as a minor oddity, these internal tremors can range from harmless muscle twitches to signals of underlying neurological or circulatory issues. While most cases resolve on their own, persistent or worsening symptoms may indicate a condition requiring medical evaluation. Understanding the root causes—and knowing when to be concerned—can help prevent complications and support timely intervention.
Common Causes of Foot Vibrations
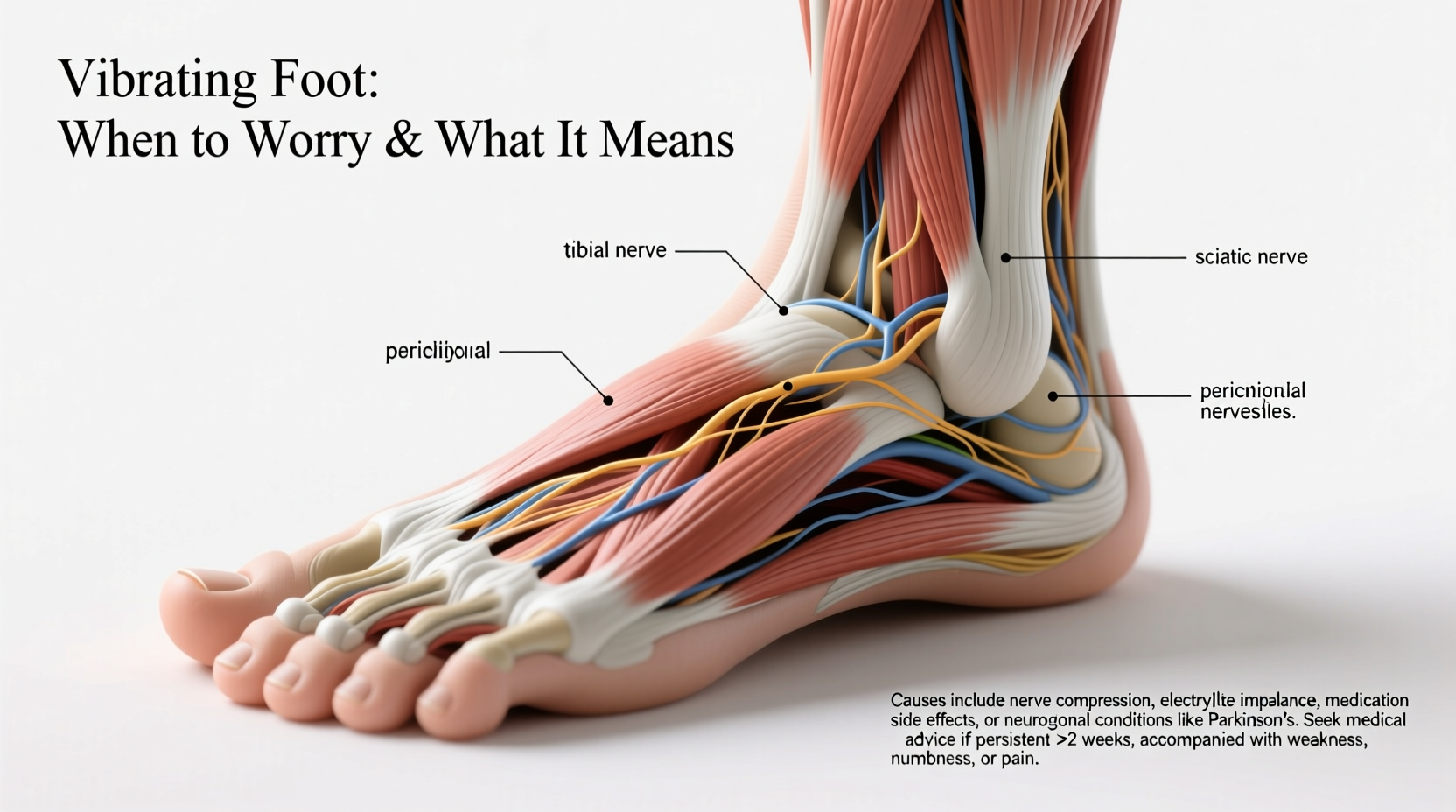
The sensation of a vibrating foot is typically not caused by actual movement but rather by abnormal nerve signaling or muscle activity. These phantom vibrations can stem from several sources, both benign and more serious.
- Muscle fatigue: Prolonged standing, intense physical activity, or overuse of foot muscles can lead to micro-tremors perceived as vibrations.
- Nerve compression: Conditions like tarsal tunnel syndrome or sciatica can irritate nerves leading to the foot, causing tingling, buzzing, or vibrating feelings.
- Peripheral neuropathy: Often linked to diabetes, vitamin deficiencies (especially B12), or alcohol use, this condition damages peripheral nerves and commonly presents with burning, numbness, or electric-like sensations.
- Restless Legs Syndrome (RLS): Though primarily affecting the legs, RLS can extend into the feet, producing an irresistible urge to move along with crawling or vibrating sensations, especially at night.
- Electrolyte imbalances: Low levels of potassium, calcium, or magnesium disrupt normal nerve and muscle function, potentially triggering unusual sensations.
When to Worry: Red Flags That Require Medical Attention
While intermittent foot vibrations are usually temporary and harmless, certain patterns and accompanying symptoms should prompt concern. Recognizing these warning signs early can make a significant difference in diagnosis and treatment outcomes.
“Persistent internal tremors without visible movement should never be ignored—especially if they spread or worsen over time.” — Dr. Lena Patel, Neurologist at Boston General Hospital
Seek medical evaluation if you experience any of the following:
- Vibrations lasting longer than two weeks without improvement
- Progressive numbness, weakness, or loss of coordination in the foot or leg
- Pain that radiates from the lower back down to the foot
- Symptoms that interfere with sleep or daily activities
- Bilateral involvement (both feet affected simultaneously)
- History of diabetes, autoimmune disorders, or recent injury
Case Example: Early Detection Prevents Complications
Mark, a 54-year-old office worker with type 2 diabetes, began noticing a faint buzzing sensation in his left foot after long days at his desk. Initially dismissing it as fatigue, he eventually sought care when the feeling became constant and was accompanied by reduced sensitivity to temperature. Testing revealed moderate peripheral neuropathy due to poorly controlled blood sugar. With medication adjustments, physical therapy, and improved glucose monitoring, Mark’s symptoms stabilized within three months. His case underscores the importance of not ignoring subtle neurological changes, especially in high-risk individuals.
Diagnostic Process: What to Expect
If foot vibrations persist, a healthcare provider will likely conduct a comprehensive assessment to determine the underlying cause. This process typically includes:
- Medical history review: Focus on chronic conditions, medications, lifestyle habits, and symptom onset.
- Neurological examination: Tests for reflexes, muscle strength, sensation, and coordination.
- Blood work: To check for diabetes, thyroid dysfunction, vitamin deficiencies, and inflammatory markers.
- Nerve conduction studies (NCS) and electromyography (EMG): These assess how well nerves transmit signals and whether muscles respond appropriately.
- Imaging: MRI or CT scans may be ordered if spinal nerve compression is suspected.
| Test | Purpose | Indicates |
|---|---|---|
| Blood Glucose & HbA1c | Evaluate diabetes control | Chronic hyperglycemia damaging nerves |
| Vitamin B12 Level | Assess nutritional status | Deficiency-related neuropathy |
| EMG/NCS | Measure nerve and muscle function | Peripheral neuropathy or radiculopathy |
| Lumbar MRI | Visualize spine and nerve roots | Herniated disc or spinal stenosis |
Managing and Treating Underlying Causes
Treatment depends entirely on the diagnosed cause. There is no one-size-fits-all solution, but addressing the root issue often resolves or significantly reduces the vibrating sensation.
- For diabetic neuropathy: Tight glycemic control through diet, medication, and regular monitoring is essential.
- For vitamin deficiency: Supplementation with B12, folate, or other nutrients under medical supervision can reverse symptoms.
- For nerve compression: Physical therapy, ergonomic adjustments, or in severe cases, surgical decompression may be necessary.
- For RLS: Lifestyle changes such as reducing caffeine, maintaining a regular sleep schedule, and sometimes dopamine-regulating medications can provide relief.
Self-Care Checklist for Managing Foot Vibrations
Use this checklist to monitor symptoms and support nerve health:
- ✅ Track when vibrations occur (time of day, activity level)
- ✅ Check blood sugar regularly if diabetic
- ✅ Take prescribed vitamins or supplements consistently
- ✅ Avoid tight footwear and prolonged pressure on feet
- ✅ Practice daily foot inspections for cuts, sores, or swelling
- ✅ Limit alcohol and quit smoking to improve circulation
- ✅ Schedule follow-up appointments as recommended
Frequently Asked Questions
Can anxiety cause a vibrating sensation in the foot?
Yes. Anxiety and stress can trigger hyperventilation and increased muscle tension, which may lead to paresthesia—abnormal sensations including tingling, buzzing, or vibrations. These are usually temporary and subside once the anxiety episode passes.
Is a vibrating foot a sign of multiple sclerosis (MS)?
While MS can cause various sensory disturbances, isolated foot vibrations are rarely the first or only symptom. MS typically presents with additional neurological signs such as vision problems, balance issues, or muscle spasms. However, unexplained neurological symptoms warrant evaluation by a neurologist.
Why does my foot vibrate only at night?
Nocturnal vibrations may be linked to restless legs syndrome, poor circulation, or positional nerve compression during sleep. It could also reflect heightened awareness of bodily sensations in a quiet environment. Keeping a symptom diary helps identify patterns.
Conclusion: Listen to Your Body
The human body communicates through sensations, and a vibrating foot—however subtle—is one form of that dialogue. While often benign, recurring or escalating symptoms deserve attention. Ignoring them may delay diagnosis of conditions that, if caught early, are manageable or even reversible. Whether it's adjusting your lifestyle, correcting a deficiency, or seeking specialist care, taking proactive steps today can preserve mobility and comfort tomorrow.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?