Experiencing vomiting shortly after a meal can be alarming, uncomfortable, and disruptive to daily life. While occasional nausea or vomiting may result from overeating or mild indigestion, recurrent or severe episodes often point to underlying health issues. Understanding the root causes and knowing how to respond appropriately can make a significant difference in managing symptoms and preventing complications.
This article explores the most frequent reasons people vomit after eating, outlines practical strategies for relief and prevention, and highlights when medical evaluation is essential. Whether the issue stems from diet, infection, or chronic illness, timely intervention and informed choices support better digestive health.
Digestive Triggers: Common Causes of Post-Meal Vomiting
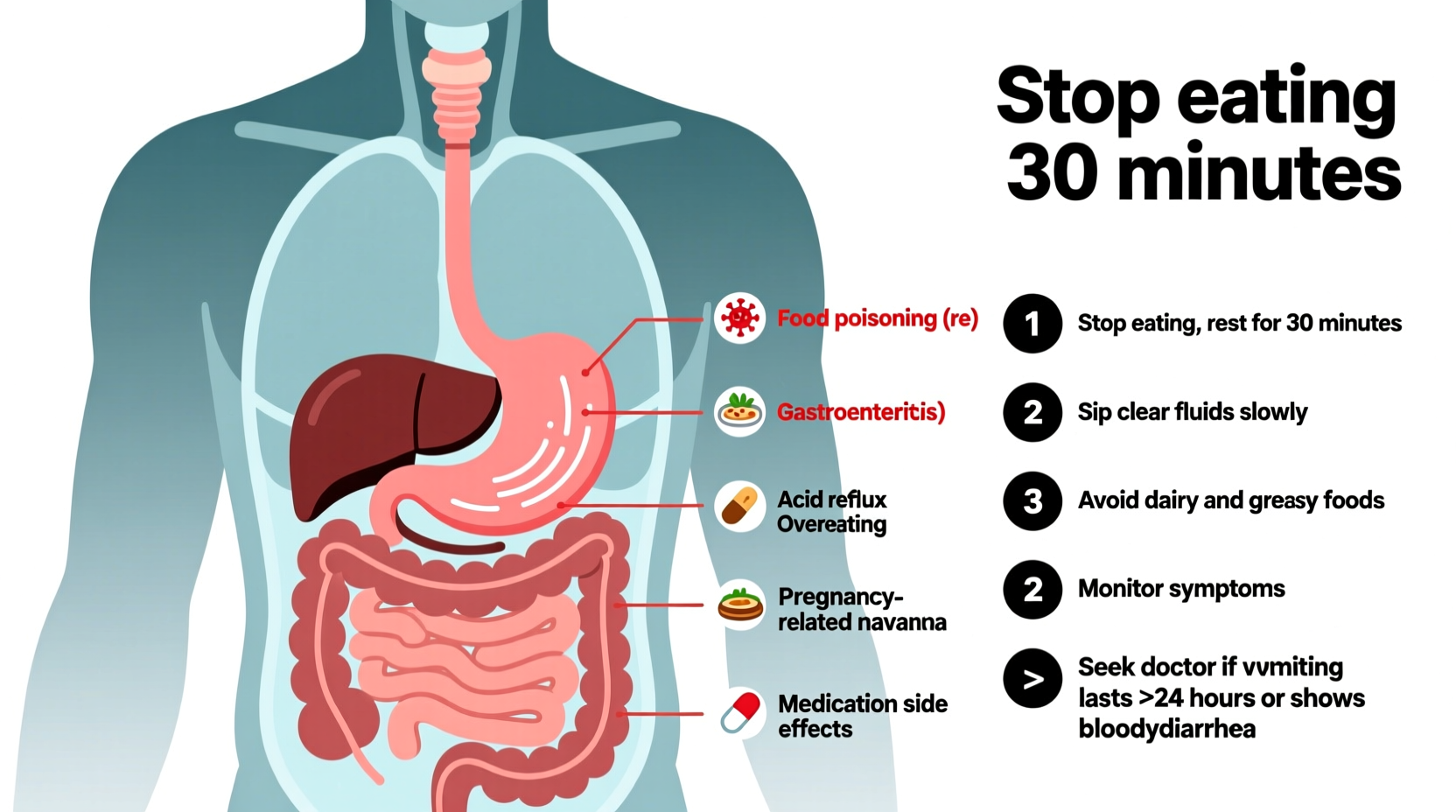
Vomiting after eating is not a diagnosis but a symptom that can arise from various conditions affecting the gastrointestinal system and beyond. Some causes are temporary and easily resolved; others require ongoing management.
- Food poisoning: Consuming contaminated food introduces bacteria like Salmonella or E. coli, leading to nausea, vomiting, and diarrhea within hours of ingestion.
- Gastroesophageal reflux disease (GERD): Stomach acid flows back into the esophagus, causing irritation. In severe cases, this can trigger regurgitation or vomiting, especially after large or fatty meals.
- Gastroparesis: A condition where the stomach empties too slowly due to nerve damage—commonly seen in people with diabetes. Symptoms include early fullness, bloating, and vomiting undigested food hours after eating.
- Pyloric stenosis: More common in infants, but rare adult cases involve narrowing of the stomach’s exit valve, blocking food passage and causing projectile vomiting.
- Food intolerances or allergies: Lactose intolerance, gluten sensitivity (non-celiac), or true food allergies can provoke nausea and vomiting after consuming trigger foods.
- Eating too quickly or overeating: Large portions overwhelm the stomach, increasing pressure and triggering reflexive vomiting.
- Pregnancy: Morning sickness, especially in the first trimester, frequently causes post-meal nausea and vomiting.
When Illness Mimics Indigestion: Serious Conditions to Consider
While many cases of vomiting after eating are benign, some stem from serious medical conditions requiring prompt attention. These should not be ignored, especially if symptoms persist or worsen.
Pancreatitis—inflammation of the pancreas—often presents with upper abdominal pain radiating to the back, nausea, and vomiting after meals, particularly those high in fat. Alcohol use and gallstones are common causes.
Peptic ulcers, typically caused by H. pylori infection or prolonged NSAID use, can lead to stomach pain and vomiting, sometimes with blood. The discomfort may temporarily improve with eating but return as digestion progresses.
Intestinal obstruction blocks the passage of food through the digestive tract. Symptoms include cramping, bloating, inability to pass gas, and vomiting—sometimes of fecal-like material in advanced cases.
“Recurrent vomiting after meals, especially if associated with weight loss or pain, warrants investigation. It’s not something to dismiss as mere indigestion.” — Dr. Lena Torres, Gastroenterologist
Immediate Steps to Take After Vomiting
Knowing how to respond in the hours following an episode can reduce discomfort and prevent dehydration or further irritation.
- Stop eating and drinking temporarily: Allow your stomach 30–60 minutes to settle. Sudden intake can trigger another bout.
- Sip clear fluids: Start with small amounts of water, diluted apple juice, or oral rehydration solutions. Avoid sugary, carbonated, or acidic drinks.
- Rest in an upright position: Lying flat increases the risk of aspiration and acid reflux. Sit or recline slightly elevated.
- Gradually reintroduce bland foods: Once nausea subsides, try small portions of toast, rice, bananas, or boiled potatoes (the BRAT diet).
- Avoid strong smells and spicy foods: Sensory triggers can reignite nausea even after initial recovery.
| Do | Don’t |
|---|---|
| Sip water slowly every 10–15 minutes | Drink large amounts quickly |
| Eat small, low-fat, bland meals | Consume fried, spicy, or dairy-rich foods |
| Rest with head elevated | Lie flat immediately after vomiting |
| Monitor for signs of dehydration | Ignore persistent symptoms beyond 24 hours |
Preventing Recurrence: Lifestyle and Dietary Adjustments
For many individuals, long-term relief comes from modifying eating habits and addressing contributing lifestyle factors.
- Eat smaller, more frequent meals: Five to six mini-meals reduce stomach strain compared to three large ones.
- Chew thoroughly and eat slowly: This aids digestion and prevents air swallowing, which contributes to bloating and nausea.
- Avoid lying down within 2–3 hours of eating: Gravity helps keep stomach contents down, reducing reflux risk.
- Limit alcohol and caffeine: Both relax the lower esophageal sphincter and irritate the stomach lining.
- Manage stress: Anxiety impacts gut motility. Techniques like deep breathing, meditation, or yoga may improve digestive function.
Real-Life Example: Identifying Gastroparesis Early
Sarah, a 42-year-old office worker with type 2 diabetes, began experiencing nausea and vomiting 1–2 hours after lunch. At first, she assumed it was food-related. Over several weeks, symptoms worsened, and she noticed undigested food in her vomit days after eating. She also felt full after just a few bites.
After consulting her doctor, Sarah underwent a gastric emptying study, which confirmed gastroparesis. With medication, dietary changes (smaller, low-fiber meals), and better blood sugar control, her symptoms improved significantly within two months. Her case illustrates the importance of tracking symptoms and seeking evaluation when vomiting becomes a pattern rather than an isolated event.
When to Seek Medical Help
While self-care works for mild, infrequent episodes, certain red flags demand professional assessment:
- Vomiting lasting more than 24 hours without improvement
- Blood in vomit (appears bright red or like coffee grounds)
- Severe abdominal pain or swelling
- Inability to keep any liquids down
- Signs of dehydration: dark urine, dizziness, dry mouth, rapid heartbeat
- Unintentional weight loss
- Fever above 101°F (38.3°C) accompanying vomiting
Diagnostic tools such as endoscopy, ultrasound, gastric emptying studies, or blood tests may be used to pinpoint the cause. Treatment varies widely—from antibiotics for H. pylori to surgery for obstructions.
FAQ
Can anxiety cause vomiting after eating?
Yes. Severe anxiety or panic attacks can activate the autonomic nervous system, disrupting digestion and triggering nausea or vomiting, even without a physical gastrointestinal disorder.
Is it normal to vomit after every meal during pregnancy?
While morning sickness is common, vomiting after every meal—especially if it leads to dehydration or weight loss—may indicate hyperemesis gravidarum, a serious condition requiring medical treatment.
Why do I feel nauseous only after eating certain foods?
This could signal a food intolerance (like lactose or gluten), allergy, or sensitivity. Keeping a detailed food log and working with a healthcare provider can help identify and eliminate triggers.
Conclusion
Vomiting after eating is more than an inconvenience—it’s a signal from your body that something needs attention. Whether due to poor eating habits, an acute infection, or a chronic condition, understanding the cause is the first step toward relief. Simple adjustments in diet and routine can prevent many episodes, while recognizing warning signs ensures timely care when needed.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?