Waking up with a parched mouth is more than just an unpleasant morning sensation—it can signal underlying health issues and disrupt your overall well-being. Dry mouth upon waking affects millions of people, often leading to bad breath, difficulty swallowing, and increased risk of dental problems like cavities and gum disease. While occasional dryness may be harmless, persistent symptoms warrant attention. Understanding the root causes and knowing how to address them can transform your mornings and support long-term oral and systemic health.
Why Saliva Matters for Oral Health
Saliva plays a crucial role in maintaining oral balance. It lubricates tissues, neutralizes acids produced by bacteria, aids digestion, and helps wash away food particles. During sleep, saliva production naturally decreases, but it should not stop entirely. When the mouth becomes excessively dry overnight, the protective functions of saliva are compromised, creating an environment where harmful bacteria thrive.
Chronic dry mouth—medically known as xerostomia—is not a condition in itself but a symptom of other factors, ranging from lifestyle habits to medical conditions. Left untreated, it can lead to tooth decay, oral infections, and even impact speech and taste. Recognizing the signs early allows for timely intervention.
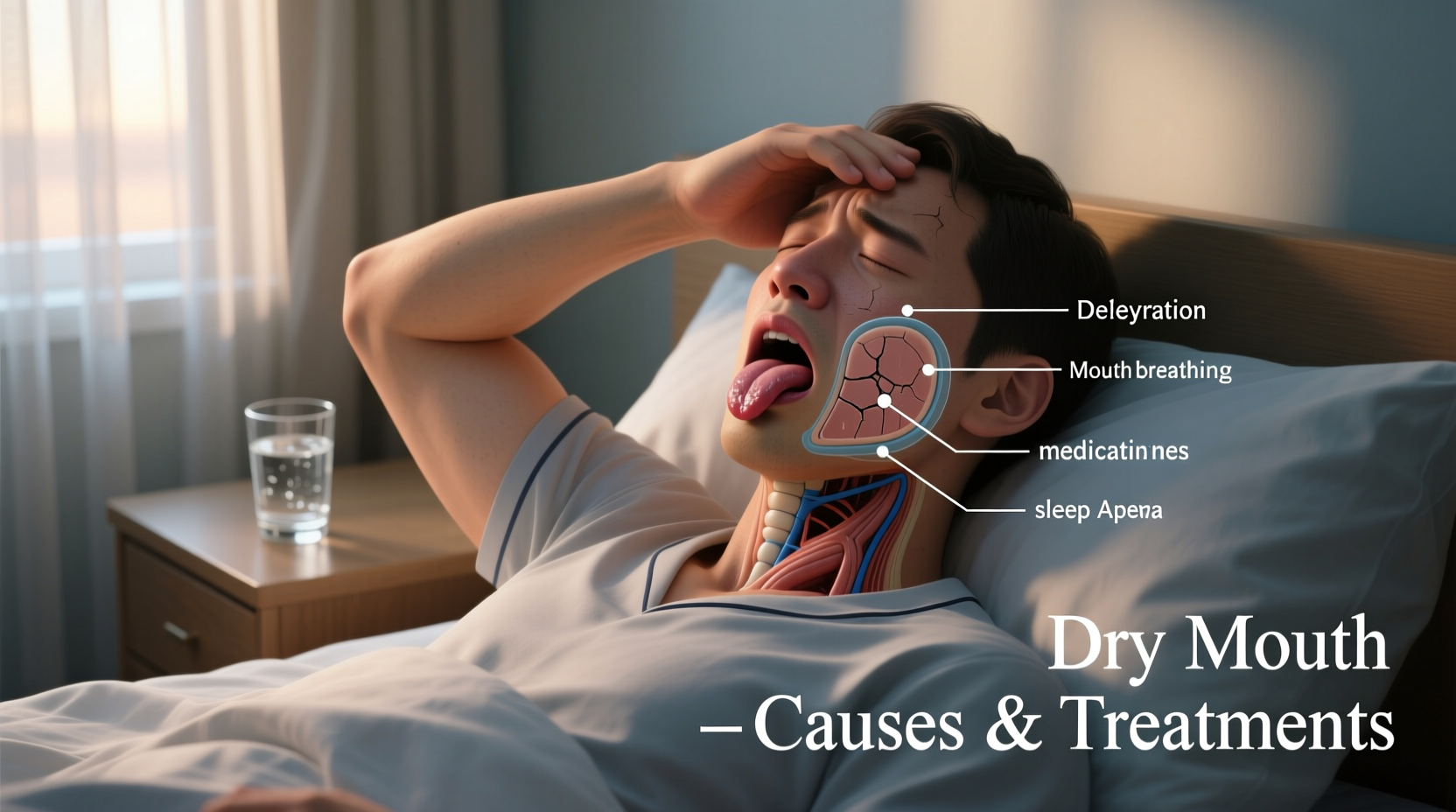
Common Causes of Waking Up with Dry Mouth
Dry mouth at night rarely has a single cause. Instead, it typically results from a combination of physiological, environmental, and behavioral factors. Below are the most frequent contributors:
- Dehydration: Not drinking enough water during the day reduces overall fluid levels, which directly affects saliva production.
- Medications: Over 400 commonly prescribed drugs list dry mouth as a side effect, including antihistamines, decongestants, antidepressants, blood pressure medications, and diuretics.
- Mouth Breathing: Whether due to nasal congestion, sleep apnea, or habit, breathing through the mouth dries out oral tissues rapidly.
- Alcohol and Caffeine: Both act as diuretics and reduce saliva flow. Consuming them in the evening intensifies nighttime dryness.
- Smoking or Tobacco Use: These substances irritate oral tissues and inhibit salivary gland function.
- Aging: Natural changes in salivary glands and increased medication use make older adults more susceptible.
- Medical Conditions: Autoimmune disorders like Sjögren’s syndrome, diabetes, Parkinson’s disease, and HIV/AIDS can impair saliva production.
- Radiation Therapy: Patients receiving head or neck radiation often experience permanent damage to salivary glands.
How Sleep Habits Influence Dry Mouth
Your sleep environment and behaviors significantly affect oral moisture. Sleeping in a room with low humidity—especially in winter when heating systems run—can dry out the air and your mouth. Using a central heating system without humidification exacerbates this issue.
Mouth breathing during sleep is one of the most overlooked causes. It often stems from obstructed nasal passages due to allergies, deviated septum, or sinusitis. In some cases, it's linked to obstructive sleep apnea (OSA), a serious sleep disorder where breathing repeatedly stops and starts. People with OSA frequently wake with a dry mouth because they breathe through their mouths to compensate for restricted airflow.
“Persistent dry mouth upon waking should never be ignored—especially if accompanied by snoring or daytime fatigue. It could be a red flag for undiagnosed sleep apnea.” — Dr. Lena Patel, Board-Certified Sleep Specialist
Effective Treatments and Lifestyle Adjustments
Treating dry mouth begins with identifying and addressing the underlying cause. For many, simple lifestyle modifications yield noticeable improvements within days.
Step-by-Step Guide to Reduce Nighttime Dry Mouth
- Stay Hydrated Throughout the Day: Aim for at least 8 glasses of water daily. Avoid waiting until you're thirsty, as thirst is a late sign of dehydration.
- Limit Evening Alcohol and Caffeine: Cut off coffee after 2 p.m. and avoid alcoholic beverages within 3 hours of bedtime.
- Use a Humidifier at Night: A cool-mist humidifier adds moisture to the air, reducing tissue dryness. Clean it regularly to prevent mold buildup.
- Treat Nasal Congestion: Use saline sprays, nasal strips, or allergy medications to promote nasal breathing.
- Switch Medications If Possible: Talk to your doctor about alternatives to drugs causing dry mouth. Never discontinue medication without medical advice.
- Practice Good Oral Hygiene: Brush twice daily with fluoride toothpaste, floss, and use an alcohol-free mouthwash designed for dry mouth.
- Avoid Tobacco and Reduce Sugar Intake: Both worsen dryness and increase cavity risk.
Over-the-Counter and Prescription Solutions
For those who need additional support, several products can help stimulate or replace saliva:
| Solution Type | Examples | How It Helps |
|---|---|---|
| Artificial Saliva | XyliMelts, Biotène OralBalance | Coats the mouth to provide moisture and comfort |
| Saliva Stimulants | Sugar-free gum with xylitol, pilocarpine (prescription) | Promotes natural saliva flow |
| Moisturizing Mouthwashes | Biotène Dry Mouth Rinse, ACT Total Care Sensitive | Hydrates without alcohol irritation |
| Nasal Dilators | Breathe Right strips, internal nasal cones | Improve airflow through the nose, reducing mouth breathing |
When to See a Doctor
If dry mouth persists despite lifestyle changes, consult a healthcare provider. Chronic xerostomia may indicate a systemic condition requiring diagnosis and treatment. Your doctor may perform blood tests, imaging of salivary glands, or refer you to a dentist, ENT specialist, or sleep clinic.
A mini case study illustrates this point:
Maria, a 54-year-old teacher, struggled with severe morning dry mouth for months. She tried drinking more water and using mouthwash, but her symptoms worsened. After a dental checkup revealed multiple new cavities, her dentist referred her to an ENT. Testing confirmed she had undiagnosed Sjögren’s syndrome—an autoimmune disorder attacking moisture-producing glands. With proper treatment, including prescription saliva stimulants and immune-modulating therapy, Maria’s symptoms improved dramatically within weeks.
Frequently Asked Questions
Can dry mouth cause bad breath?
Yes. Saliva helps cleanse the mouth and control odor-causing bacteria. When saliva is lacking, bacteria multiply, leading to persistent halitosis, especially in the morning.
Is dry mouth a sign of diabetes?
It can be. High blood sugar levels lead to increased urination and dehydration, contributing to dry mouth. Other symptoms include excessive thirst, frequent urination, and fatigue. If you have these signs, ask your doctor about glucose testing.
Are there foods that make dry mouth worse?
Dry, salty, spicy, or sugary foods can irritate oral tissues and worsen discomfort. Opt for moist foods like soups, stews, and fruits with high water content such as melons and oranges.
Final Thoughts and Action Plan
Waking up with dry mouth is a common but manageable issue. The key is to approach it holistically—assess your hydration, review medications, optimize your sleep environment, and prioritize nasal breathing. Small, consistent changes often lead to significant improvements in comfort and oral health.
If home remedies don’t bring relief within two weeks, seek professional evaluation. Early detection of conditions like sleep apnea or autoimmune disease can prevent complications down the line.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?