You turn up the heat, wrap yourself in a blanket, and yet you're still shivering while others are comfortable—or even warm. If this sounds familiar, you’re not imagining things. Persistent feelings of coldness, especially in environments where others feel fine, can be a subtle but significant signal from your body. While environmental factors or personal preference play a role, chronic cold sensitivity may point to underlying physiological or medical conditions. Understanding the root causes empowers you to take informed action—whether it’s adjusting lifestyle habits or seeking medical evaluation.
The Physiology of Body Temperature Regulation
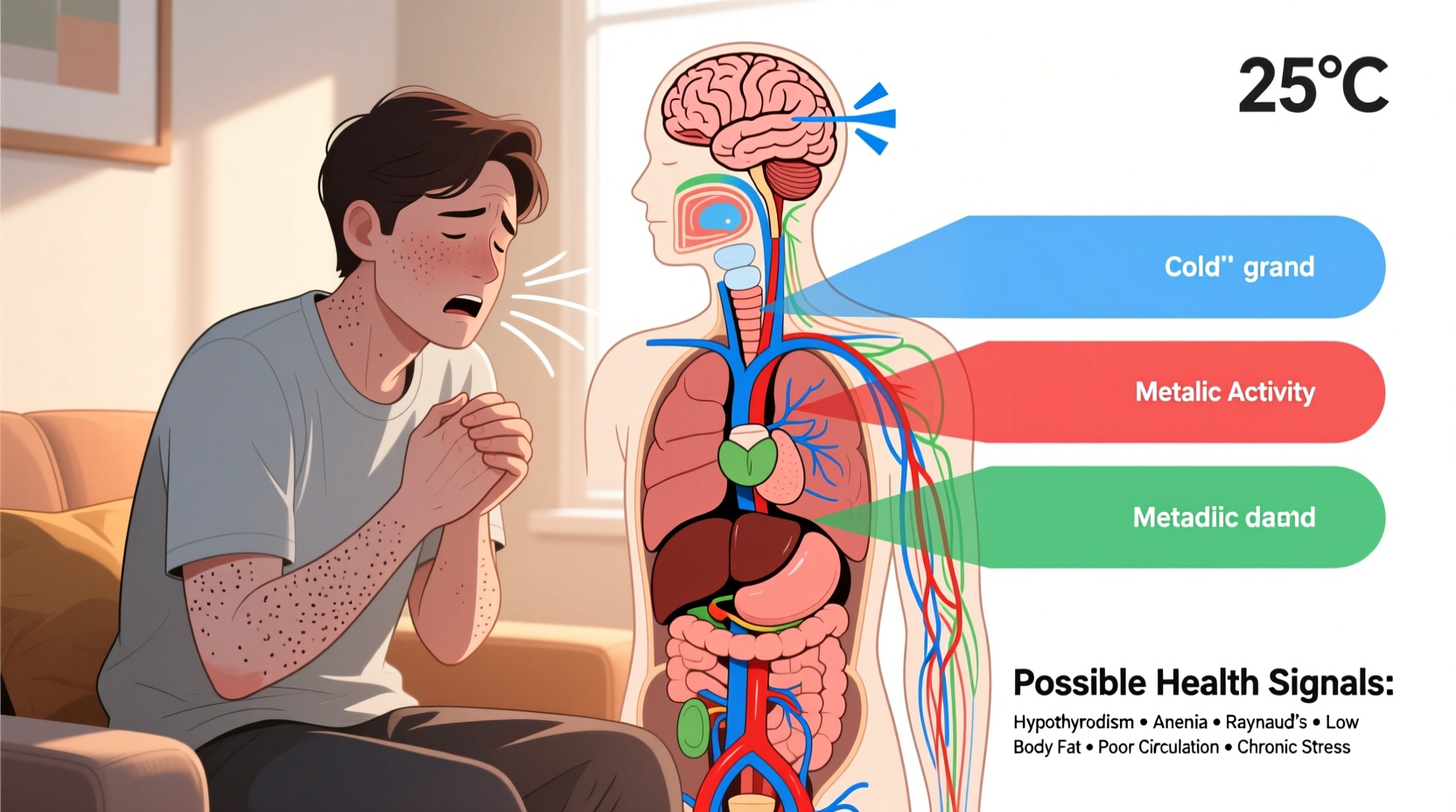
Your body maintains a core temperature of around 98.6°F (37°C) through a complex system managed by the hypothalamus in the brain. This internal thermostat constantly monitors and adjusts heat production and loss via mechanisms like shivering, sweating, blood vessel constriction, and metabolic activity. When this system is disrupted—even slightly—you may experience dysregulation, leading to sensations of cold despite ambient warmth.
Peripheral circulation plays a key role. Blood carries heat throughout the body. If circulation to your extremities (hands, feet, nose) is reduced, those areas will feel colder. This can happen due to vascular issues, nervous system dysfunction, or hormonal imbalances. Additionally, metabolic rate influences how much heat your body generates at rest. A slower metabolism means less internal heat production, increasing susceptibility to cold.
Common Medical Conditions Linked to Chronic Cold Sensitivity
Feeling cold isn’t always a standalone symptom. Often, it's one piece of a larger clinical picture. Several health conditions are known to disrupt thermoregulation or reduce baseline body heat production.
Anemia
Iron-deficiency anemia is a leading cause of persistent coldness. Iron is essential for hemoglobin, which carries oxygen in red blood cells. Without sufficient oxygen delivery, cellular metabolism slows, reducing energy and heat output. Women with heavy menstrual cycles, individuals with poor diets, or those with gastrointestinal blood loss are particularly vulnerable.
Hypothyroidism
The thyroid gland regulates metabolism. When it underperforms (hypothyroidism), your metabolic rate drops, leading to fatigue, weight gain, dry skin—and a constant feeling of being cold. The condition is more common in women over 50 but can affect anyone. A simple blood test measuring TSH (thyroid-stimulating hormone) can confirm diagnosis.
“Patients with undiagnosed hypothyroidism often report feeling cold months before other symptoms become apparent. It’s one of the earliest and most consistent complaints.” — Dr. Lena Torres, Endocrinologist, Cleveland Clinic
Raynaud’s Phenomenon
This condition causes exaggerated vasoconstriction in response to cold or stress, primarily affecting fingers and toes. Small arteries spasm, drastically reducing blood flow and causing affected areas to turn white, then blue, then red as circulation returns. While often triggered by cold environments, Raynaud’s can make someone feel cold even indoors if their extremities aren’t receiving adequate blood flow.
Diabetes and Peripheral Neuropathy
Long-term high blood sugar damages nerves and blood vessels, particularly in the hands and feet. This neuropathy can distort temperature perception, making limbs feel cold, numb, or tingly—even when they’re not objectively cold. Poor circulation compounds the issue.
Heart Failure and Circulatory Issues
A weakened heart pumps less efficiently, reducing blood flow to peripheral tissues. As a result, extremities receive less warm blood, leading to persistent cold hands and feet. Other signs include shortness of breath, swelling in the legs, and fatigue.
Lifestyle and Non-Medical Factors That Contribute
Not every case of chronic coldness stems from disease. Daily habits and environmental exposures significantly influence how your body manages temperature.
- Low body fat percentage: Subcutaneous fat acts as natural insulation. Athletes or individuals with very lean builds may feel cold more easily.
- Sedentary lifestyle: Physical activity increases circulation and metabolic heat. Sitting for long periods reduces blood flow to limbs.
- Caffeine and nicotine: Both are vasoconstrictors—they narrow blood vessels, limiting peripheral circulation.
- Dehydration: Reduced blood volume impairs circulation and heat distribution.
- Poor nutrition: Deficiencies in iron, vitamin B12, and folate impair red blood cell production and oxygen transport.
When to See a Doctor: Warning Signs Beyond Coldness
Occasional chills aren’t alarming. But if you're consistently cold and notice accompanying symptoms, it’s time to consult a healthcare provider. Consider scheduling an appointment if you experience:
- Fatigue or unexplained weakness
- Dry skin, hair loss, or brittle nails
- Irregular heartbeat or palpitations
- Unintended weight changes (gain or loss)
- Pale or yellowish skin tone
- Numbness, tingling, or color changes in fingers/toes
- Heavy menstrual bleeding (in women)
Early detection of conditions like hypothyroidism or anemia can prevent complications such as heart strain, cognitive decline, or worsening neuropathy.
Diagnostic Steps Your Doctor May Take
A thorough evaluation typically includes:
- Blood tests: CBC (complete blood count), ferritin, TSH, free T4, vitamin B12, glucose levels
- Physical exam: Checking skin texture, reflexes, pulse strength in extremities
- Medical history review: Medications, diet, family history of autoimmune or endocrine disorders
| Condition | Key Diagnostic Test | Associated Symptoms |
|---|---|---|
| Anemia | CBC, Ferritin | Fatigue, pale skin, dizziness |
| Hypothyroidism | TSH, Free T4 | Weight gain, constipation, depression |
| Raynaud’s | Clinical evaluation, capillaroscopy | Color changes in fingers, pain during attacks |
| Diabetes | Fasting glucose, HbA1c | Thirst, frequent urination, slow healing |
| Heart Disease | Echocardiogram, ECG | Shortness of breath, swelling, chest discomfort |
Practical Strategies to Reduce Cold Sensitivity
Whether you're managing a diagnosed condition or simply want to improve comfort, targeted actions can make a real difference.
Step-by-Step Guide to Staying Warmer Naturally
- Layer clothing strategically: Use moisture-wicking base layers, insulating mid-layers (like wool), and wind-resistant outerwear—even indoors if needed.
- Warm your core first: Focus on heating your torso with vests or heated garments. A warm core improves overall circulation.
- Stay active: Take short walks, stretch hourly, or do light resistance exercises to boost circulation.
- Optimize your diet: Include iron-rich foods (red meat, spinach, lentils), B12 sources (eggs, dairy, fortified cereals), and healthy fats (avocados, nuts).
- Hydrate wisely: Sip warm herbal teas or water throughout the day. Avoid excessive caffeine and alcohol.
- Use localized heat: Heated blankets, foot warmers, or hand warmers can provide relief without overheating a room.
Checklist: What You Can Do Today
- ✔️ Take a morning walk to stimulate circulation
- ✔️ Add iron-rich foods to your next meal
- ✔️ Check your thermostat setting—aim for at least 68–70°F (20–21°C)
- ✔️ Schedule a blood test if you’ve never been screened for anemia or thyroid issues
- ✔️ Replace synthetic pajamas with thermal or wool blends
Real-Life Example: Sarah’s Journey to Diagnosis
Sarah, a 38-year-old graphic designer, spent years thinking she was just “always cold.” Coworkers opened windows while she wore a sweater and scarf year-round. She dismissed it until she began experiencing hair thinning, constipation, and overwhelming fatigue. After researching her symptoms online, she requested a thyroid panel from her doctor. Her TSH level was 8.2 mIU/L (normal is 0.4–4.0), confirming hypothyroidism.
Within weeks of starting levothyroxine, Sarah noticed dramatic improvements—not just in energy and digestion, but in her ability to regulate body temperature. “I didn’t realize how much I’d adapted to feeling cold,” she said. “Now I actually feel warm in the same office where I used to shiver.” Her story highlights how easily subtle symptoms can be normalized—until they begin to interfere with daily life.
Frequently Asked Questions
Can anxiety make me feel cold?
Yes. Anxiety triggers the sympathetic nervous system, which can cause vasoconstriction—reducing blood flow to the skin and extremities. This may lead to cold hands, feet, or even full-body chills despite normal room temperature. Panic attacks often include sensations of coldness or shivering unrelated to actual temperature.
Is it normal for older adults to feel colder?
Partially. Aging reduces subcutaneous fat, slows metabolism, and diminishes circulation and skin sensitivity. However, extreme cold intolerance shouldn’t be dismissed as “just aging.” It may indicate anemia, thyroid dysfunction, or cardiovascular issues that require treatment.
Can medications cause cold sensitivity?
Yes. Beta-blockers (used for high blood pressure and anxiety), certain migraine medications (like triptans), and some psychiatric drugs can constrict blood vessels or alter metabolic function, leading to increased cold perception.
Conclusion: Listen to Your Body’s Signals
Feeling cold when others don’t may seem minor, but it’s your body’s way of communicating imbalance. Whether rooted in nutrition, circulation, hormones, or chronic illness, persistent coldness deserves attention—not dismissal. By combining self-awareness with proactive health checks, you can uncover hidden issues early and restore comfort naturally or with medical support.
If you've been asking, “Why am I always cold even in warm rooms?” consider it a prompt to investigate deeper. Track your symptoms, adjust lifestyle factors, and don’t hesitate to request blood work. Your internal thermostat matters—and tuning into its signals today can prevent bigger problems tomorrow.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?