Chronic nasal congestion affects millions of people worldwide, often disrupting sleep, reducing concentration, and diminishing quality of life. While occasional stuffiness after a cold is normal, persistent congestion may point to underlying health issues or environmental triggers. Understanding the root causes—and knowing how to respond effectively—can make a significant difference in your daily comfort and respiratory health.
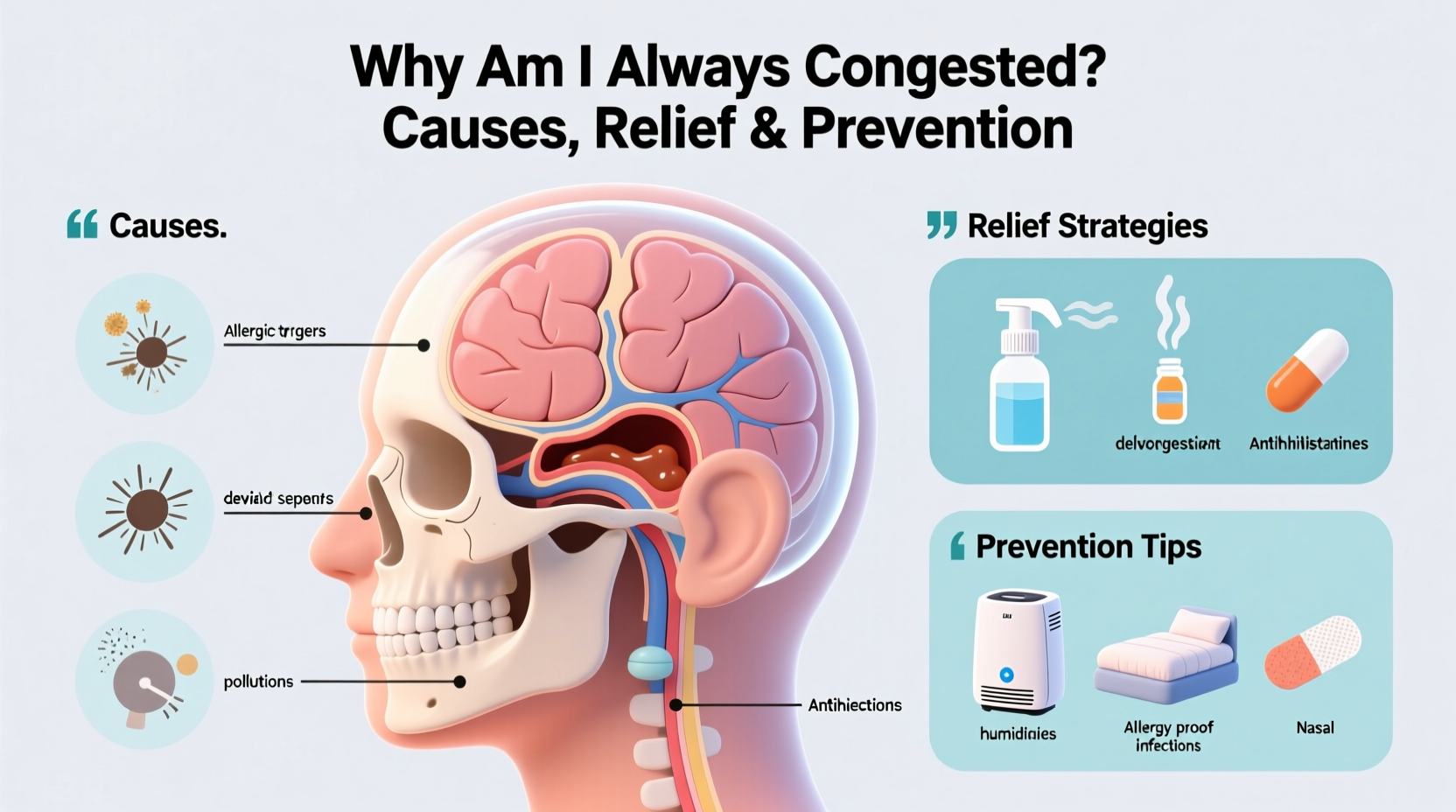
Common Causes of Persistent Nasal Congestion
Nasal congestion occurs when the tissues lining the nasal passages become swollen due to inflamed blood vessels. This inflammation can stem from various sources, both temporary and chronic.
- Allergic Rhinitis: Also known as hay fever, this immune response to allergens like pollen, dust mites, pet dander, or mold leads to ongoing nasal swelling and mucus production.
- Non-Allergic Rhinitis: Triggered by irritants such as smoke, strong odors, weather changes, or certain medications, without an allergic component.
- Sinus Infections (Sinusitis): Bacterial or viral infections in the sinuses cause prolonged congestion, facial pressure, and discolored mucus lasting more than 10 days.
- Nasal Polyps: Soft, noncancerous growths in the nasal passages or sinuses that obstruct airflow and contribute to chronic blockage.
- Deviated Septum: A crooked nasal septum can restrict one or both nasal passages, leading to one-sided or constant congestion.
- Medication Side Effects: Drugs such as beta-blockers, some antidepressants, and overuse of nasal decongestant sprays (rhinitis medicamentosa) can worsen congestion.
- Hormonal Changes: Pregnancy, menstruation, or thyroid disorders can alter blood flow in nasal tissues, increasing swelling.
“Persistent nasal congestion shouldn’t be ignored. It’s not just about discomfort—it can affect sleep quality, lead to mouth breathing, and even contribute to fatigue.” — Dr. Lena Patel, Otolaryngologist
Effective Relief Strategies for Immediate Comfort
While treating the underlying cause is essential, immediate relief helps restore function and improve well-being. The following methods are clinically supported and widely recommended.
Saline Irrigation
Using a neti pot or saline spray helps flush out mucus, allergens, and irritants from the nasal cavity. Regular use reduces inflammation and improves drainage.
Steam Inhalation
Inhaling warm, moist air loosens mucus and soothes irritated membranes. Add a few drops of eucalyptus oil for enhanced effect, but avoid direct contact with skin or eyes.
Warm Compresses
Applying a warm towel over the nose and sinuses helps open nasal passages and relieve sinus pressure.
Over-the-Counter (OTC) Medications
Choose based on symptoms:
- Antihistamines (e.g., loratadine, cetirizine): Best for allergy-related congestion.
- Decongestants (e.g., pseudoephedrine, phenylephrine): Reduce swelling quickly but should not be used longer than 3–5 days.
- Nasal corticosteroid sprays (e.g., fluticasone, mometasone): Most effective for long-term control of inflammation, especially in allergies.
Prevention: Building Long-Term Respiratory Health
Preventing recurrence requires identifying and managing triggers. Here’s how to create a sustainable plan.
Control Your Environment
Indoor air quality plays a major role in nasal health.
- Use HEPA air purifiers to reduce airborne allergens.
- Wash bedding weekly in hot water to eliminate dust mites.
- Keep windows closed during high pollen seasons.
- Avoid smoking and secondhand smoke exposure.
Maintain Optimal Humidity
Dry air irritates nasal passages. Aim for indoor humidity between 40% and 60%. Too much moisture, however, encourages mold growth—use a hygrometer to monitor levels.
Stay Hydrated
Drinking plenty of fluids thins mucus, making it easier to drain. Herbal teas, broths, and water are excellent choices.
Manage Allergies Proactively
If allergies are confirmed, consider immunotherapy (allergy shots or sublingual tablets) for long-term desensitization.
Step-by-Step Guide to Assessing and Addressing Chronic Congestion
- Track Symptoms: Keep a daily log noting congestion severity, timing, triggers (e.g., pets, weather), and associated symptoms like headaches or post-nasal drip.
- Eliminate Obvious Triggers: Remove scented candles, clean HVAC filters, wash stuffed animals, and vacuum regularly.
- Start Saline Rinses: Begin daily nasal irrigation using a neti pot or squeeze bottle.
- Begin Daily Nasal Spray: Use an OTC steroid spray consistently for at least two weeks before evaluating effectiveness.
- Consult a Specialist: If no improvement after 3–4 weeks, see an ENT or allergist for evaluation (possible allergy testing, CT scan, or endoscopy).
- Discuss Treatment Options: Depending on diagnosis, treatments may include prescription medications, polyp removal, or surgical correction of structural issues.
Do’s and Don’ts: Quick Reference Table
| Do’s | Don’ts |
|---|---|
| Use saline sprays daily | Use nasal decongestant sprays for more than 3 days |
| Run a humidifier in dry environments | Ignore persistent congestion lasting over 2 weeks |
| Shower before bed to rinse off allergens | Smoke or expose yourself to strong chemical fumes |
| Take prescribed medications consistently | Self-diagnose structural issues like deviated septum |
| See an allergist if seasonal patterns emerge | Overuse antihistamines causing drowsiness or dryness |
Real-Life Example: Sarah’s Journey to Clearer Breathing
Sarah, a 34-year-old teacher, had struggled with year-round congestion for over five years. She assumed it was “just allergies” and relied on OTC decongestants. However, her symptoms worsened—she began snoring, waking up tired, and experiencing frequent sinus headaches.
After seeing an allergist, she discovered she had both dust mite allergies and nasal polyps. Her treatment plan included a daily steroid spray, biweekly saline rinses, replacing her bedroom carpet with hardwood, and undergoing minor outpatient surgery to remove the polyps.
Within three months, Sarah reported dramatic improvement. She no longer needed rescue medications and finally slept through the night. Her case highlights the importance of accurate diagnosis and comprehensive care.
Frequently Asked Questions
Can dehydration cause nasal congestion?
Yes. When dehydrated, mucus becomes thicker and harder to clear, leading to a sensation of blockage. Staying hydrated helps maintain thin, flowing mucus that drains easily.
Why do I only get congested at night?
Lying down increases blood flow to the nasal passages, which can worsen swelling. Additionally, allergens in pillows, bedding, or bedroom air (like dust or pet dander) may trigger nighttime symptoms.
Is it safe to use nasal sprays every day?
It depends on the type. Corticosteroid sprays (e.g., Flonase) are safe for daily, long-term use. However, decongestant sprays (e.g., Afrin) should be limited to 3 consecutive days to avoid rebound congestion.
Conclusion: Take Control of Your Breathing and Well-Being
Chronic congestion is more than a nuisance—it's a signal from your body that something needs attention. Whether it’s an allergic reaction, structural issue, or environmental irritant, identifying the cause is the first step toward lasting relief. Simple lifestyle adjustments, consistent hygiene practices, and timely medical consultation can transform your breathing and overall vitality.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?