Rectal bleeding is more common than many people realize, yet it often triggers anxiety. The sight of blood—whether bright red on toilet paper or mixed with stool—can be alarming. While some causes are benign and easily treatable, others may signal a serious underlying condition. Understanding the difference between harmless and dangerous bleeding can help you make informed decisions about when to seek care.
Bleeding from the anus typically originates in the lower gastrointestinal tract. The color, amount, and accompanying symptoms offer clues about the source. Bright red blood usually indicates a problem close to the anus, such as hemorrhoids or anal fissures. Darker, maroon, or black stool (melena) suggests bleeding higher in the digestive tract, like the colon or stomach, which may be more urgent.
Common Causes of Anal Bleeding
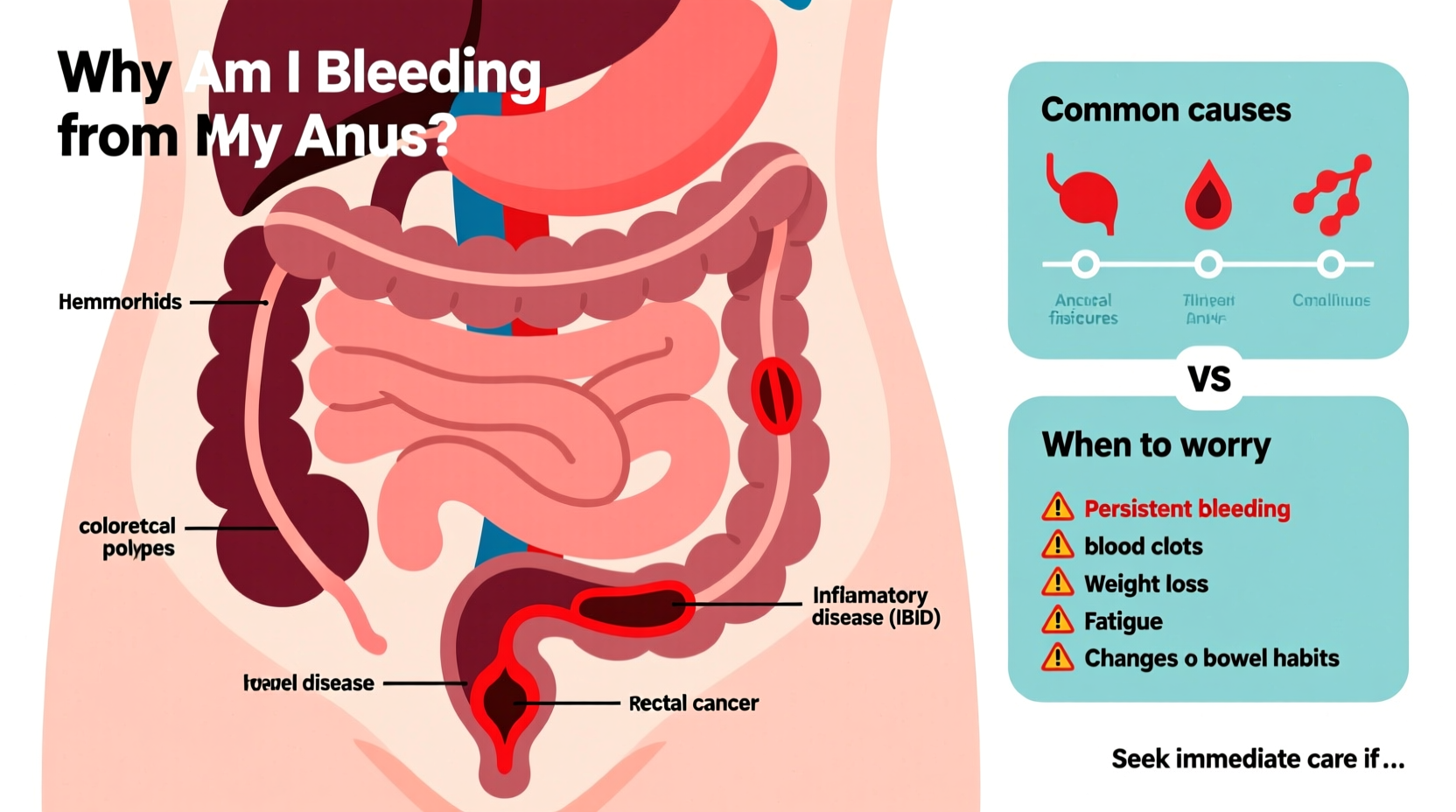
Most cases of rectal bleeding stem from non-life-threatening conditions. However, even mild symptoms should not be ignored if they persist.
- Hemorrhoids: Swollen veins in the rectum or around the anus. Internal hemorrhoids may bleed during bowel movements without pain, while external ones can cause itching, swelling, and discomfort.
- Anal fissures: Small tears in the lining of the anus, often caused by passing hard stools. These can produce sharp pain during defecation and streaks of bright red blood.
- Constipation: Straining due to infrequent or difficult bowel movements increases pressure in the rectal veins and can lead to both hemorrhoids and fissures.
- Proctitis: Inflammation of the rectal lining, sometimes due to infections (like sexually transmitted infections), inflammatory bowel disease (IBD), or radiation therapy.
- Diverticulosis: Small pouches that form in the colon wall. If one becomes inflamed or ruptures, it can cause sudden, painless rectal bleeding—usually moderate to heavy and bright red.
When to Worry: Warning Signs That Demand Medical Attention
While occasional minor bleeding may resolve on its own, certain symptoms indicate the need for prompt evaluation. Delaying care in these cases can have serious consequences.
“Not all rectal bleeding is created equal. Persistent or heavy bleeding—even without pain—should always be assessed.” — Dr. Lena Patel, Gastroenterologist at Cleveland Clinic Digestive Institute
Seek immediate medical attention if you experience any of the following:
- Heavy or continuous bleeding
- Dark red or maroon-colored stool
- Black, tarry stools (a sign of upper GI bleeding)
- Dizziness, lightheadedness, or fainting (signs of significant blood loss)
- Unexplained weight loss
- Persistent abdominal pain or cramping
- Change in bowel habits lasting more than a few days
- A family history of colorectal cancer
These red flags could point to conditions such as colorectal cancer, inflammatory bowel disease (Crohn’s disease or ulcerative colitis), ischemic colitis, or severe infections.
Understanding the Risk: Age, Lifestyle, and Screening
Age plays a major role in assessing risk. Colorectal cancer is rare under age 40 but rises sharply after 50. That’s why screening colonoscopies are recommended starting at age 45 for average-risk individuals, per guidelines from the American Cancer Society.
Lifestyle factors also influence your likelihood of developing conditions that cause rectal bleeding:
| Risk Factor | Associated Condition | Prevention Strategy |
|---|---|---|
| Low-fiber diet | Hemorrhoids, constipation | Eat fruits, vegetables, whole grains |
| Sedentary lifestyle | Slowed digestion, diverticulosis | Exercise regularly, stay active |
| Chronic straining | Anal fissures, hemorrhoids | Improve toilet posture (use a footstool) |
| Smoking and alcohol | Colorectal polyps, cancer | Quit smoking, limit alcohol |
| Family history of cancer | Hereditary colon cancer syndromes | Early and frequent screening |
What Happens During a Medical Evaluation?
If you visit a doctor for rectal bleeding, expect a thorough assessment. This begins with a detailed history: when the bleeding started, its frequency, appearance, associated symptoms, diet, medications, and family history.
Next, a physical exam may include a digital rectal examination (DRE), where the physician checks for abnormalities using a gloved finger. Depending on findings, further testing may be ordered:
- Anoscopy or sigmoidoscopy: A short scope examines the lower rectum and anus.
- Colonoscopy: A full view of the colon to detect polyps, inflammation, or tumors. Often done under sedation.
- Fecal occult blood test (FOBT): Checks for hidden blood in stool.
- Imaging: CT scan or MRI if structural issues are suspected.
Biopsies may be taken during endoscopic procedures to rule out cancer or confirm inflammatory conditions.
Mini Case Study: Recognizing a Silent Threat
Mark, a 58-year-old accountant, noticed occasional bright red blood on the toilet paper for several months. He assumed it was hemorrhoids—common in his family—and used over-the-counter creams. But after six months, he began feeling fatigued and lost 12 pounds unintentionally. His primary care doctor ordered a colonoscopy, which revealed a large tumor in the descending colon. Early intervention led to surgery and chemotherapy. Mark later said, “I wish I hadn’t waited. The bleeding was a warning I ignored.”
This case underscores a critical point: persistent bleeding—even if mild—deserves investigation, especially in older adults.
Step-by-Step Guide: What to Do If You Notice Rectal Bleeding
Follow this timeline to manage concerns safely and effectively:
- Day 1–2: Observe symptoms. Note the color, amount, frequency, and whether it's associated with pain, changes in bowel habits, or other symptoms.
- Day 3: Adjust lifestyle. Increase fiber, hydrate well, avoid straining. Use a sitz bath if discomfort is present.
- Day 5–7: Reassess. If bleeding stops and no other symptoms exist, monitor closely. If it persists beyond a week, schedule a doctor’s visit.
- Immediately: Seek emergency care if bleeding is heavy, accompanied by dizziness, or if stool is black/tarry.
- Within 2 weeks: Follow up with screening if you’re over 45 or have a family history of colon cancer, regardless of symptom resolution.
FAQ
Is it normal to see blood after a hard bowel movement?
Occasional spotting due to straining or a small anal tear can happen and often resolves within a few days. However, recurring episodes should be evaluated to rule out chronic hemorrhoids or fissures.
Can hemorrhoids turn into cancer?
No, hemorrhoids themselves do not become cancerous. But their symptoms can mimic those of colorectal cancer. Persistent bleeding should always be confirmed through proper diagnosis.
Do I need a colonoscopy if I’m young and bleeding?
While less common, young people can develop IBD, infections, or even early-onset colorectal cancer. If symptoms persist or worsen, diagnostic testing is appropriate at any age.
Conclusion: Take Control of Your Digestive Health
Seeing blood from the anus doesn't automatically mean something is seriously wrong—but it does mean something is happening in your body that warrants attention. Whether it's a simple fix like adding more fiber or a call for deeper investigation, your response today shapes your long-term health.
Don’t normalize symptoms because they seem common. Early detection saves lives, especially when it comes to conditions like colorectal cancer, which is highly treatable when caught early. Listen to your body, act with care, and never hesitate to ask for professional insight.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?