You can bend your thumbs back to touch your forearms, twist your limbs into positions most people find impossible, or have been called \"double jointed\" since childhood. While it may seem like a quirky party trick, this ability is actually due to joint hypermobility—a condition more complex than casual labels suggest. Far from having extra joints, individuals with this trait possess unusually flexible connective tissues, particularly ligaments and tendons, which allow for greater-than-normal range of motion in one or more joints.
Joint hypermobility affects up to 20% of the population, with higher prevalence in children, women, and certain ethnic groups. For some, it's a harmless flexibility quirk; for others, it’s part of a broader health concern. Understanding the science behind hypermobility, its implications, and how to manage it is essential for maintaining long-term joint health and overall well-being.
What Does “Double Jointed” Actually Mean?
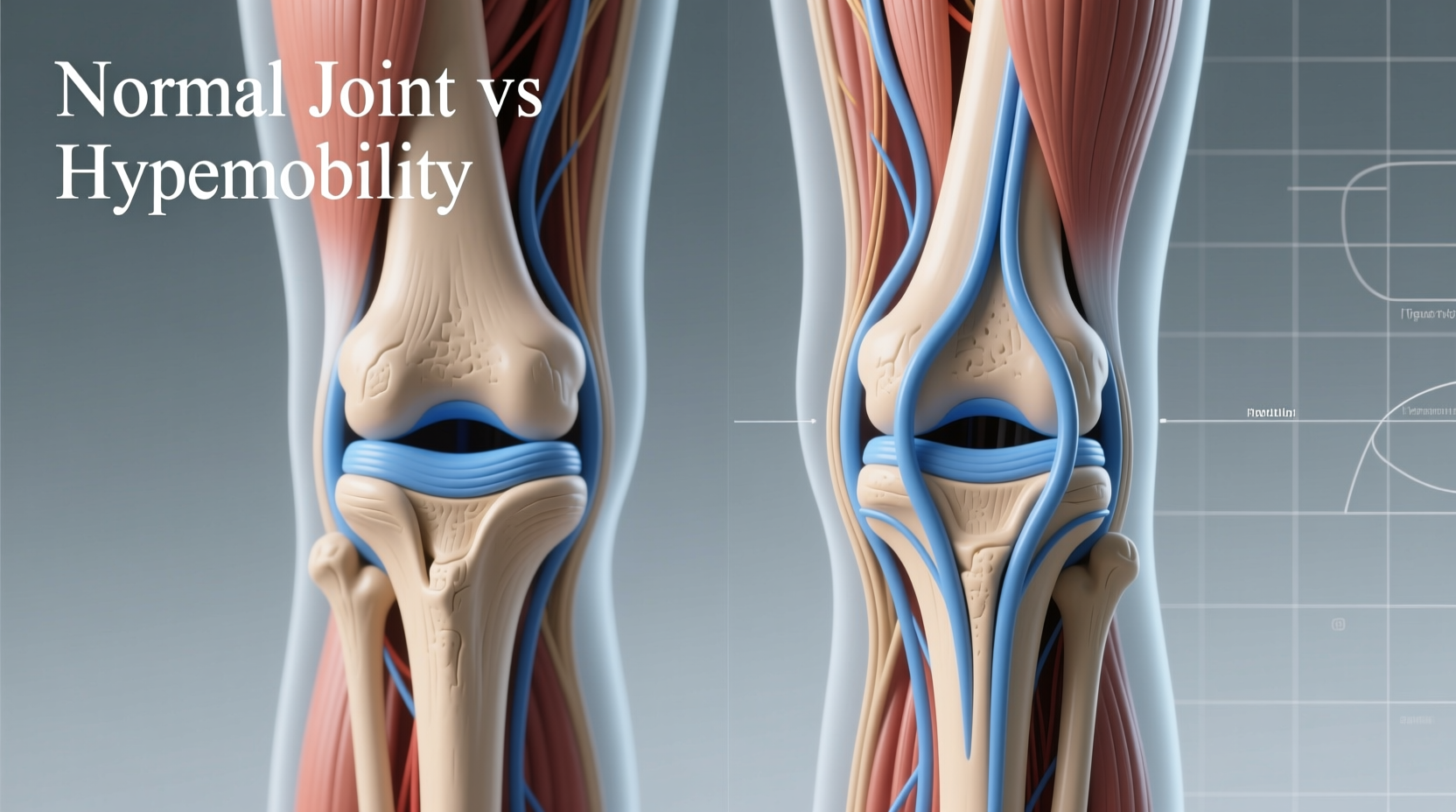
The term \"double jointed\" is a misnomer. No one has extra joints. Instead, the phrase refers to people whose joints move beyond the typical range seen in most individuals. This increased mobility stems from differences in collagen—the primary protein in connective tissues like ligaments and tendons. In hypermobile individuals, collagen is more elastic, allowing joints to stretch further without immediate resistance.
Hypermobility can be localized (affecting only a few joints) or generalized (involving multiple joints throughout the body). It’s often identified using the Beighton Score, a clinical assessment that tests flexibility in five specific movements:
- Can you place your palms flat on the floor without bending your knees?
- Can you bend your elbows or knees backward more than 10 degrees?
- Can you bend your thumbs to touch your forearms?
- Can you spread your fingers unusually wide?
- Have you ever been able to perform splits without training?
A score of 5 or more out of 9 typically indicates generalized joint hypermobility. However, a high score alone doesn’t mean there’s an underlying disorder—it simply identifies increased flexibility.
The Spectrum of Hypermobility: From Advantage to Disorder
Not all hypermobility is problematic. Dancers, gymnasts, musicians, and yogis often benefit from enhanced flexibility, giving them a physical edge. But when joint laxity leads to symptoms like chronic pain, dislocations, or fatigue, it may signal a connective tissue disorder.
The most common conditions linked to symptomatic hypermobility include:
- Benign Joint Hypermobility Syndrome (BJHS): A diagnosis given when hypermobility causes pain but no identifiable genetic disorder.
- Hypermobile Ehlers-Danlos Syndrome (hEDS): A hereditary condition involving widespread joint instability, soft tissue fragility, and systemic symptoms such as gastrointestinal issues or autonomic dysfunction.
- Marfan Syndrome: A genetic disorder affecting connective tissue, often involving tall stature, long limbs, and cardiovascular complications.
“Hypermobility isn't just about flexibility—it’s about stability. When ligaments are too loose, muscles must compensate, leading to strain and fatigue over time.” — Dr. Lena Torres, Rheumatologist and Connective Tissue Specialist
Recognizing Symptoms Beyond Flexibility
Many people live years without realizing their hypermobility is connected to recurring issues. Common signs that go beyond mere flexibility include:
- Recurrent sprains or joint subluxations (partial dislocations)
- Chronic joint or muscle pain, especially after activity
- Fatigue that worsens with prolonged standing or walking
- Clicking, popping, or instability in joints during movement
- Soft tissue injuries like tendonitis or bursitis
- Poor proprioception (awareness of joint position), increasing fall risk
In more systemic forms like hEDS, additional symptoms may appear, such as easy bruising, digestive problems, dizziness, or skin that stretches easily. These clues suggest the issue extends beyond musculoskeletal flexibility and involves broader connective tissue involvement.
Real-Life Example: Maya’s Journey to Diagnosis
Maya, a 28-year-old graphic designer, had always been praised for her flexibility. She could effortlessly do the splits and often entertained friends by bending her fingers backward. But in her mid-twenties, she began experiencing persistent knee pain, frequent ankle rolls, and unexplained fatigue. Doctors initially dismissed her concerns, attributing them to poor posture or stress.
After a shoulder dislocation during yoga, she sought a second opinion. A rheumatologist administered the Beighton test, reviewed her medical history, and diagnosed her with hypermobile Ehlers-Danlos Syndrome. With proper guidance, Maya began a targeted strength program, learned joint protection techniques, and started managing her symptoms proactively. Her story highlights the importance of looking beyond surface-level flexibility to assess functional impact.
Managing Hypermobility: A Proactive Approach
While hypermobility itself can’t be “cured,” its effects can be significantly reduced through intelligent management. The key lies in building muscular support around loose joints to improve stability and prevent injury.
Step-by-Step Guide to Building Joint Stability
- Consult a Specialist: See a physiotherapist experienced in hypermobility or connective tissue disorders for a personalized assessment.
- Start Low-Impact Strengthening: Focus on controlled exercises targeting core, hips, shoulders, and ankles—such as Pilates, resistance bands, or bodyweight routines.
- Avoid Overstretching: Skip deep stretching or advanced yoga poses that push joints beyond safe limits.
- Improve Proprioception: Practice balance exercises like single-leg stands or use a wobble board to enhance joint awareness.
- Monitor Activity Levels: Pace yourself throughout the day. Fatigue is a warning sign—don’t push through pain.
- Use Supportive Gear if Needed: Braces, kinesiology tape, or orthotics can provide external stability during high-demand activities.
Do’s and Don’ts of Daily Living with Hypermobility
| Do | Don’t |
|---|---|
| Engage in regular, moderate strength training | Perform high-impact sports like basketball or parkour without conditioning |
| Use ergonomic tools to reduce hand strain | Hold heavy bags on one shoulder or overextend wrists while typing |
| Sit with back support and feet flat on the floor | “Wiggle” joints for relief—it increases laxity over time |
| Wear supportive footwear with good arch support | Go barefoot on hard surfaces for extended periods |
| Take breaks during prolonged standing or sitting | Ignore swelling or recurring joint pain |
Frequently Asked Questions
Can joint hypermobility get worse over time?
Yes, without proper management, repeated joint stress can lead to early wear-and-tear, increasing the risk of osteoarthritis. Poor muscle support and repeated micro-injuries contribute to worsening symptoms. However, consistent strength training and joint protection can slow or prevent deterioration.
Is hypermobility inherited?
Frequently, yes. Most cases of generalized hypermobility run in families, especially those linked to hEDS or Marfan syndrome. These are autosomal dominant conditions, meaning a child has a 50% chance of inheriting the gene variant if one parent is affected.
Should I stop exercising if I’m hypermobile?
No—exercise is essential, but the type matters. Avoid high-impact, contact, or extreme flexibility-based activities. Instead, focus on low-impact strength training, swimming, cycling, and neuromuscular control exercises that build stability without overstressing joints.
Conclusion: Embrace Awareness, Not Limitation
Being “double jointed” is more than a curiosity—it’s a physiological reality with real implications. Whether your flexibility is a silent asset or a source of discomfort, understanding your body’s mechanics empowers better choices. By shifting focus from flexibility to stability, you can protect your joints, reduce pain, and maintain an active, fulfilling life.
Knowledge is the first step toward control. If you’ve spent years wondering why your joints behave differently, take action today: assess your symptoms, consult a specialist, and begin building strength where it matters most.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?