Hallucinations can be disorienting, frightening, and confusing—especially when they occur unexpectedly. You might see something that isn’t there, hear voices with no source, or feel sensations on your skin that have no physical cause. While occasional perceptual distortions can happen under extreme stress or fatigue, persistent or recurring hallucinations often point to underlying medical, neurological, or psychological conditions. Understanding why you’re experiencing these sensory events is the first step toward appropriate care.
This article explores the science behind hallucinations, categorizes their types, outlines common and rare causes, and provides clear guidance on when professional intervention is necessary. Whether you're experiencing mild visual disturbances or full-blown auditory episodes, recognizing the patterns and triggers can make a critical difference in your health journey.
What Are Hallucinations?
A hallucination is a sensory experience that appears real but has no external stimulus. Unlike illusions—misinterpretations of actual stimuli—hallucinations are entirely fabricated by the brain. They can affect any of the five senses and vary widely in intensity, duration, and frequency.
These experiences are not always linked to severe mental illness. Many people encounter hallucinations during periods of sleep deprivation, intense grief, or high fever. However, recurrent or disruptive hallucinations may indicate a more serious condition requiring evaluation.
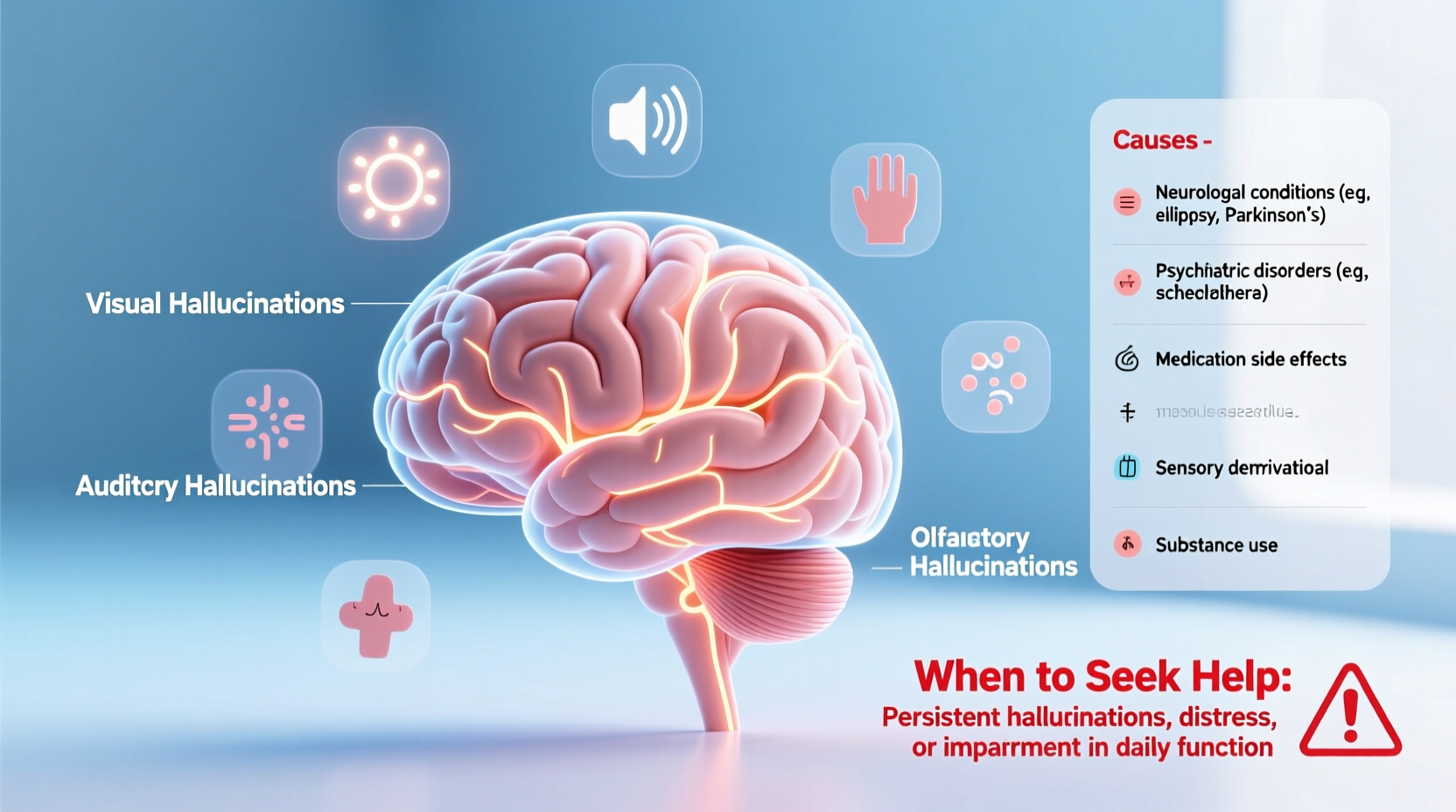
Types of Hallucinations
Hallucinations manifest in different forms depending on which sensory system is involved. The most common types include:
- Visual: Seeing shapes, lights, people, or objects that aren't present. Common in delirium, migraines, or certain psychiatric disorders.
- Auditory: Hearing voices, music, or sounds with no origin. Most frequently associated with schizophrenia but also seen in bipolar disorder and trauma.
- Tactile: Feeling sensations like crawling insects, pressure, or burning on the skin. Often reported in substance withdrawal (e.g., alcohol or stimulants).
- Olfactory: Smelling odors such as smoke, rot, or chemicals without a source. Can be linked to temporal lobe epilepsy or brain tumors.
- Gustatory: Tasting something unusual or unpleasant without eating anything. Less common and often tied to seizure activity.
Common Causes of Hallucinations
The brain generates hallucinations when normal sensory processing is disrupted. This disruption can stem from biological, chemical, or psychological imbalances. Below are key categories of causes:
1. Mental Health Conditions
Psychiatric disorders are among the most recognized causes of hallucinations. Schizophrenia involves frequent auditory hallucinations, often perceived as threatening or commanding voices. Bipolar disorder during manic or depressive psychosis can also trigger visual or auditory episodes. Severe depression with psychotic features may lead to guilt-laden voices or visions.
2. Neurological Disorders
Conditions affecting brain structure or function can induce hallucinations. Parkinson’s disease commonly causes vivid visual hallucinations due to dopamine therapy or neurodegeneration in visual pathways. Epilepsy, particularly temporal lobe seizures, may produce brief but intense sensory distortions. Brain tumors or strokes in sensory-processing regions can also lead to hallucinatory experiences.
3. Substance Use and Withdrawal
Psychoactive substances directly alter brain chemistry. Hallucinogens like LSD or psilocybin intentionally induce hallucinations. However, other drugs—including high-dose cannabis, amphetamines, and even prescription medications—can provoke unintended perceptual disturbances. Alcohol withdrawal, especially in delirium tremens (DTs), often includes tactile hallucinations (e.g., formication—the feeling of bugs crawling under the skin).
4. Sleep Deprivation and Disorders
Extreme fatigue impairs the brain’s ability to distinguish reality from imagination. Hypnagogic hallucinations occur as one falls asleep; hypnopompic ones happen upon waking. These are usually brief and visual or auditory but can be unsettling. Narcolepsy significantly increases the risk of such episodes.
5. Medical Illnesses
Fever, especially in children or elderly individuals, can trigger delirium and hallucinations. Infections like encephalitis or urinary tract infections in older adults may impair cognition. Metabolic imbalances—such as low sodium, liver failure, or kidney disease—also disrupt neural function and perception.
“Hallucinations are not always a sign of madness. They are signals—messages from the brain indicating something is off-balance, whether chemically, structurally, or emotionally.” — Dr. Lena Patel, Neuropsychiatrist at Boston Behavioral Health Center
When to Seek Help: Warning Signs
Not all hallucinations require emergency care, but certain red flags demand immediate attention. Knowing when to consult a healthcare provider can prevent complications.
| Situation | Action Recommended |
|---|---|
| First-time hallucination with no known cause | Schedule doctor visit within 48 hours |
| Hallucinations after head injury | Seek ER evaluation immediately |
| Voice commands to harm self or others | Contact crisis line or go to emergency room |
| Accompanied by confusion, fever, or seizures | Go to hospital—possible delirium or infection |
| Recurrent episodes disrupting daily life | See psychiatrist or neurologist for assessment |
Checklist: What to Do If You’re Hallucinating
- Stay calm and remind yourself it’s a hallucination.
- Ensure your environment is safe (e.g., sit down, avoid driving).
- Note the time, duration, and nature of the experience.
- Check recent changes: new medications, drug use, sleep patterns.
- Contact a trusted person to help assess the situation.
- Reach out to a healthcare provider for evaluation.
Real Example: A Case of Charles Bonnet Syndrome
At age 78, Robert began seeing detailed figures in his living room—children playing, fully formed but vanishing when approached. He was otherwise alert, cognitively intact, and not on psychiatric medication. After ruling out dementia and stroke, his ophthalmologist diagnosed Charles Bonnet Syndrome (CBS), a condition where vision loss leads to complex visual hallucinations. The brain, deprived of visual input, generates its own imagery.
Robert found relief simply in understanding the cause. His doctor reassured him it wasn’t a mental illness and suggested strategies like blinking rapidly or changing lighting to interrupt episodes. Over time, the hallucinations became less frequent and less distressing.
This case illustrates how non-psychiatric conditions can produce vivid hallucinations—and why thorough medical evaluation matters.
Step-by-Step Guide to Getting Proper Evaluation
If you or someone you know is experiencing hallucinations, follow this timeline to ensure comprehensive care:
- Day 1–2: Document each episode—what you saw, heard, felt, duration, and context (e.g., just woke up, stressed, ill).
- Day 3: Review all medications and supplements with a pharmacist or doctor to identify possible side effects.
- Day 5: Schedule an appointment with your primary care physician. Bring your symptom log.
- Week 2: Undergo basic tests—blood work, ECG, neurological screening—to rule out metabolic or cardiac causes.
- Week 3–4: Be referred to specialists if needed: neurologist (for seizures, dementia), psychiatrist (for psychosis), or ophthalmologist (if vision-related).
- Ongoing: Begin treatment plan—medication adjustment, therapy, or lifestyle changes—as directed.
Frequently Asked Questions
Can anxiety cause hallucinations?
Yes, in extreme cases. Severe anxiety or panic attacks may lead to brief dissociative states where a person misinterprets surroundings or hears faint voices. However, true hallucinations are more commonly linked to psychosis, neurological issues, or substance effects rather than anxiety alone.
Are hallucinations always dangerous?
No. Isolated hypnagogic hallucinations or those linked to grief or temporary illness are not inherently dangerous. But if they persist, worsen, or interfere with functioning, they should be evaluated. Safety becomes a concern if hallucinations involve command voices or paranoia.
Can lack of sleep really make me see things?
Absolutely. After 24–48 hours without sleep, the brain begins to malfunction. Visual distortions, auditory misperceptions, and even tactile sensations are well-documented in sleep-deprived individuals. Soldiers, medical residents, and new parents often report such experiences.
Conclusion: Take Action Before It Escalates
Hallucinations are not a life sentence—they are clues. Whether rooted in mental health, neurological function, or physical illness, they signal that your body or mind needs attention. Ignoring them can lead to worsening symptoms, isolation, or missed diagnoses. On the other hand, early recognition and intervention can restore stability and improve quality of life dramatically.
You don’t need to face this alone. Talk to a doctor, share your experience with someone you trust, and take the first step toward clarity. Your perception may be distorted now, but your path forward can be clear and supported.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?