Shortness of breath—medically known as dyspnea—is a sensation many people experience at some point. It can range from mild breathlessness after exertion to a terrifying feeling of not being able to catch your breath. While occasional breathlessness during physical activity is normal, persistent or sudden difficulty breathing may signal an underlying health issue. Understanding the causes, recognizing red flags, and knowing when to act can make a critical difference in outcomes.
Common Causes of Difficulty Breathing
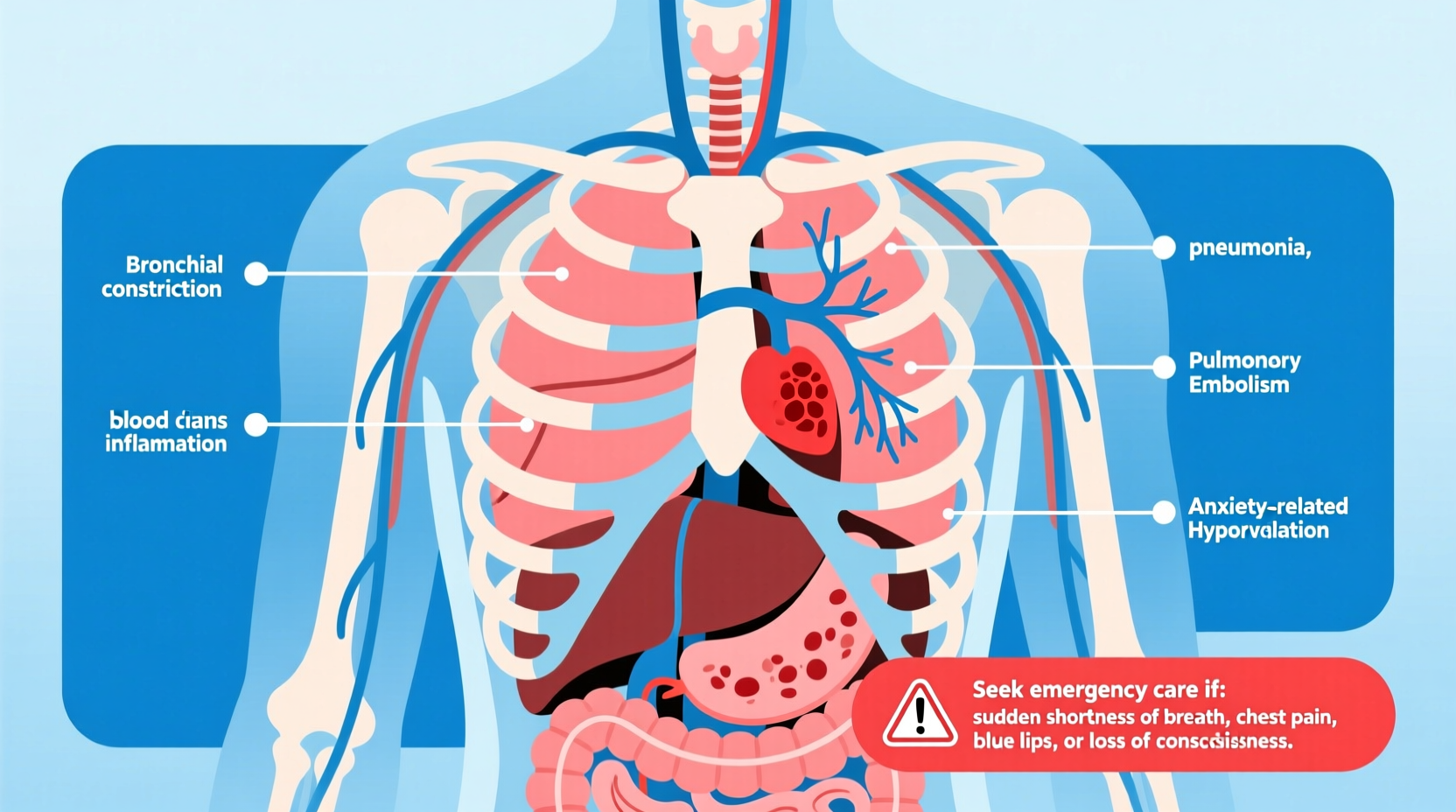
Breathing difficulties arise from a wide spectrum of conditions, some temporary and others chronic. The respiratory and cardiovascular systems are most frequently involved, but metabolic, neurological, and psychological factors also play roles.
- Asthma: A chronic condition where airways become inflamed and narrow, often triggered by allergens, cold air, or exercise.
- Chronic Obstructive Pulmonary Disease (COPD): Includes emphysema and chronic bronchitis, commonly linked to smoking.
- Pneumonia: A lung infection causing fluid buildup, leading to cough, fever, and labored breathing.
- Heart failure: When the heart can’t pump effectively, fluid may accumulate in the lungs, making breathing difficult, especially when lying down.
- Pulmonary embolism: A blood clot in the lungs that can cause sudden, severe shortness of breath and requires emergency care.
- Anxiety or panic attacks: Hyperventilation and chest tightness mimic serious conditions but stem from psychological stress.
- Obesity: Excess weight increases the workload on the heart and lungs, reducing respiratory efficiency.
- Anemia: Low red blood cell count reduces oxygen delivery, prompting faster breathing to compensate.
When to Worry: Red Flags That Demand Immediate Attention
Not all breathing problems require urgent care, but certain symptoms should never be ignored. Sudden or worsening dyspnea can indicate life-threatening conditions.
“Sudden shortness of breath with chest pain or fainting is a medical emergency. Don’t wait—call emergency services immediately.” — Dr. Lena Patel, Pulmonologist, Massachusetts General Hospital
Seek immediate medical attention if you experience any of the following:
- Chest pain, pressure, or tightness
- Pain radiating to the arm, neck, or jaw
- Sudden onset of severe breathlessness
- Bluish lips or fingertips (cyanosis)
- Confusion, dizziness, or near-fainting
- High fever with rapid breathing and chills
- Wheezing or gasping for air
- Swelling in legs or abdomen (possible heart or liver involvement)
Distinguishing Between Acute and Chronic Breathlessness
Acute breathing difficulty comes on suddenly and often indicates an emergency—such as a pulmonary embolism, heart attack, or asthma attack. Chronic dyspnea develops over weeks or months and is typically associated with long-term conditions like COPD, heart disease, or deconditioning due to inactivity.
Chronic doesn’t mean harmless. If your baseline breathing worsens gradually, it may reflect disease progression that needs evaluation.
Step-by-Step: What to Do If You’re Struggling to Breathe
If you or someone nearby experiences troubling breathlessness, follow this sequence to stay safe and get appropriate care:
- Stop activity and sit upright: This position helps expand the lungs more easily.
- Stay calm: Panic increases breathing rate. Focus on slow, deep breaths.
- Use prescribed inhalers (if asthmatic): Follow your asthma action plan if available.
- Check for other symptoms: Note chest pain, fever, swelling, or confusion.
- Call emergency services if symptoms are severe or worsening: Especially if breathing becomes extremely labored or consciousness is affected.
- Wait for help in a comfortable position: Leaning forward slightly may ease breathing in some cases.
- Follow up with a doctor: Even if symptoms resolve, unexplained dyspnea warrants medical review.
Do’s and Don’ts: Managing Breathing Difficulties
| Do’s | Don’ts |
|---|---|
| Monitor symptoms and keep a symptom diary | Ignore persistent or worsening breathlessness |
| Quit smoking and avoid secondhand smoke | Use scented candles or strong cleaners if you have asthma |
| Exercise within your limits to build endurance | Push through breathlessness during workouts |
| Keep rescue medications accessible | Self-diagnose or skip prescribed treatments |
| Get vaccinated (flu, pneumonia, COVID-19) | Delay seeking help during acute episodes |
Real Example: Recognizing a Silent Heart Condition
Sarah, a 58-year-old teacher, noticed she was getting winded climbing stairs—a task she used to handle easily. At first, she attributed it to aging and lack of exercise. Over three months, the breathlessness worsened. She began waking up at night gasping and had swollen ankles. Her primary care physician ordered an echocardiogram, which revealed moderate heart failure. With medication and lifestyle changes, Sarah regained her stamina. Her case underscores how gradual symptoms can mask serious conditions—and why early evaluation matters.
FAQ: Common Questions About Breathing Difficulties
Can anxiety really cause trouble breathing?
Yes. Anxiety triggers the body’s fight-or-flight response, leading to rapid, shallow breathing (hyperventilation). This can cause dizziness, tingling, and a sense of suffocation. While not directly life-threatening, it can mimic heart or lung emergencies. Breathing exercises and grounding techniques often help.
Is shortness of breath normal during pregnancy?
Mild breathlessness is common in pregnancy due to hormonal changes and the growing uterus pressing on the diaphragm. However, sudden or severe dyspnea, especially with chest pain or leg swelling, could indicate complications like pulmonary embolism and must be evaluated promptly.
How do doctors diagnose the cause of breathing problems?
Doctors use a combination of patient history, physical exams, and tests such as chest X-rays, spirometry (lung function test), ECG, echocardiograms, blood work (including oxygen levels and D-dimer for clots), and sometimes CT scans. The goal is to differentiate between cardiac, pulmonary, and other systemic causes.
Prevention and Long-Term Management Tips
While not all causes of dyspnea are preventable, proactive habits reduce risk and improve quality of life:
- Maintain a healthy weight: Obesity increases strain on the respiratory system.
- Exercise regularly: Aerobic activity improves lung capacity and cardiovascular health.
- Avoid lung irritants: Smoke, pollution, dust, and chemical fumes can trigger or worsen breathing issues.
- Manage chronic conditions: Control diabetes, hypertension, and asthma with proper treatment.
- Practice breathing techniques: Pursed-lip and diaphragmatic breathing help those with COPD or anxiety-related dyspnea.
Conclusion: Listen to Your Body and Act Early
Difficulty breathing is your body’s way of signaling that something isn’t right. Whether it’s due to a reversible trigger like anxiety or a serious condition like heart failure, timely recognition and response are crucial. Don’t dismiss persistent symptoms as “just getting older” or “out of shape.” Pay attention to patterns, document changes, and consult a healthcare provider for a thorough evaluation.
Early diagnosis often leads to better management and improved outcomes. If you're struggling to breathe, take it seriously—your lungs and heart depend on it.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?