Lightheadedness is a sensation many people experience at some point—feeling faint, woozy, or as though the room might spin. While often temporary and harmless, it can also signal underlying health issues. Understanding why it happens and knowing how to respond can make a significant difference in your comfort and safety.
This article explores the most frequent causes of lightheadedness, provides actionable strategies for relief, and outlines when it’s time to consult a healthcare provider. Whether you’ve felt this briefly after standing up too fast or have experienced recurring episodes, the insights here will help you take informed control.
Common Causes of Lightheadedness
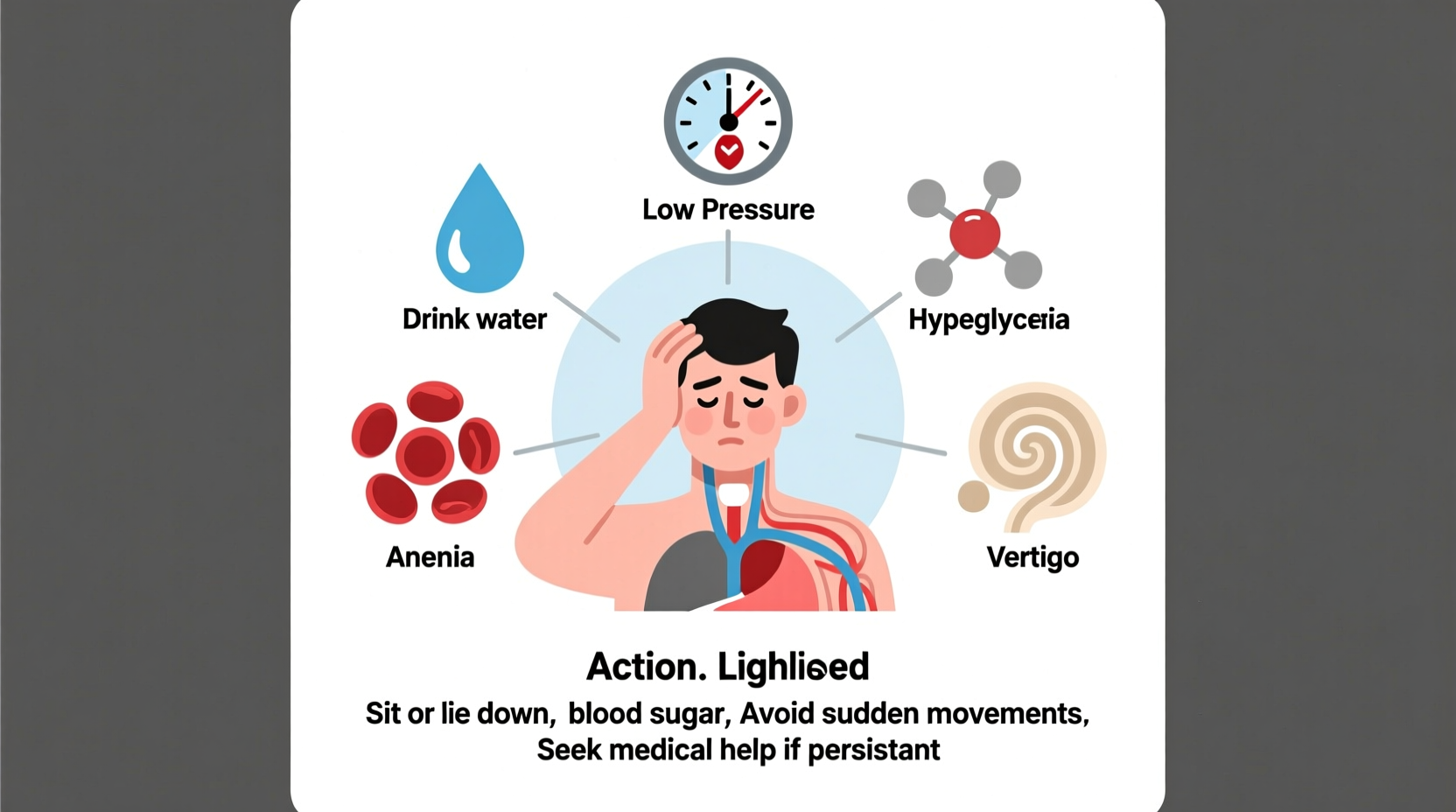
Lightheadedness arises from disruptions in blood flow, inner ear balance, or neurological signals. The triggers vary widely in severity and origin. Below are the most typical causes:
- Low blood pressure (hypotension): Especially upon standing (orthostatic hypotension), reduced blood flow to the brain causes dizziness.
- Dehydration: Inadequate fluid intake reduces blood volume, leading to drops in blood pressure and oxygen delivery.
- Low blood sugar (hypoglycemia): Common in people with diabetes, but can occur after skipping meals or intense exercise.
- Inner ear problems: Conditions like benign paroxysmal positional vertigo (BPPV), labyrinthitis, or Meniere’s disease affect balance.
- Anemia: Low red blood cell count limits oxygen transport, causing fatigue and lightheadedness.
- Medication side effects: Blood pressure drugs, antidepressants, sedatives, and diuretics may cause dizziness as a side effect.
- Anxiety or panic attacks: Rapid breathing (hyperventilation) alters carbon dioxide levels, triggering dizziness.
- Heart conditions: Arrhythmias or structural heart issues can reduce cardiac output, affecting brain perfusion.
When to Seek Medical Attention
Most cases of lightheadedness resolve quickly and don’t require emergency care. However, certain symptoms suggest a more serious condition that needs prompt evaluation.
“Dizziness alone is rarely dangerous, but when paired with chest pain, slurred speech, or loss of coordination, it could indicate a stroke or heart issue.” — Dr. Lena Patel, Neurologist at Boston General Hospital
Seek immediate medical help if lightheadedness is accompanied by:
- Chest pain or palpitations
- Difficulty speaking or confusion
- Sudden vision changes
- Weakness or numbness on one side of the body
- Fainting or near-fainting episodes
- Persistent vomiting
If symptoms recur without clear triggers or interfere with daily activities, schedule an appointment with your doctor. Diagnostic tests such as blood work, ECG, or vestibular assessments may be needed.
Immediate Actions to Take When Feeling Lightheaded
Reacting quickly during an episode can prevent falls and reduce discomfort. Follow these steps the moment you feel unsteady:
- Sit or lie down immediately. This lowers your center of gravity and improves blood flow to the brain.
- Elevate your legs if lying down. This helps return blood from the extremities to the heart and brain.
- Stay still and avoid sudden movements, especially turning your head quickly.
- Breathe slowly and deeply if anxiety is a factor. Inhale through the nose for four counts, hold for four, exhale for four.
- Hydrate with water or an electrolyte drink if dehydration is suspected.
- Eat something sugary (e.g., fruit juice, candy) if you haven’t eaten recently and suspect low blood sugar.
| Cause | Quick Relief Strategy | Prevention Tip |
|---|---|---|
| Standing up too fast | Sit back down, wait 30 seconds | Rise slowly; pause after sitting |
| Dehydration | Drink water or sports drink | Consume 6–8 glasses of fluids daily |
| Low blood sugar | Eat 15g of fast-acting carbs | Don’t skip meals; balance protein & carbs |
| Anxiety-induced | Practice box breathing | Regular mindfulness or therapy |
| Inner ear disturbance | Stay still, focus on a fixed point | Avoid sudden head movements |
Long-Term Prevention Strategies
Recurrent lightheadedness often improves with lifestyle adjustments. These evidence-based approaches can reduce frequency and severity:
- Increase fluid and salt intake (if medically appropriate): Helps maintain blood volume and pressure, especially for those with chronic low BP.
- Eat balanced meals regularly: Include complex carbohydrates, protein, and healthy fats to stabilize blood sugar.
- Exercise consistently: Cardiovascular fitness improves circulation and autonomic regulation.
- Manage stress: Chronic stress impacts blood pressure and breathing patterns. Techniques like yoga, meditation, or cognitive behavioral therapy (CBT) help.
- Review medications: Discuss side effects with your doctor. Dose adjustments or alternatives may reduce dizziness.
- Treat underlying conditions: Anemia, diabetes, thyroid disorders, and heart issues must be managed under medical supervision.
Real-Life Example: Maria’s Experience with Recurrent Dizziness
Maria, a 42-year-old teacher, began experiencing frequent lightheadedness after morning staff meetings. She often skipped breakfast and drank only coffee. Episodes worsened when she stood up to write on the board.
After tracking her symptoms for a week, she noticed a pattern: dizziness occurred before lunch and improved after eating. Her doctor diagnosed mild hypoglycemia and dehydration. With simple changes—eating a protein-rich breakfast, drinking water hourly, and pausing before standing—her symptoms resolved within two weeks.
Maria’s case illustrates how everyday habits can contribute to lightheadedness—and how small, consistent changes can restore well-being.
Step-by-Step Guide to Managing Lightheadedness
Follow this timeline to address both acute episodes and long-term prevention:
- Day 1–3: Begin symptom tracking. Record timing, triggers, duration, and what helps.
- Day 4–7: Improve hydration and nutrition. Add snacks between meals and eliminate excessive caffeine.
- Week 2: Incorporate gentle exercise like walking for 20 minutes daily to support circulation.
- Week 3: Review all medications with your doctor. Ask about dizziness as a side effect.
- Week 4: If symptoms persist, schedule a medical check-up including blood pressure, blood count, and glucose testing.
- Ongoing: Maintain healthy routines and reassess every few months, especially if new symptoms arise.
Frequently Asked Questions
Can lack of sleep cause lightheadedness?
Yes. Poor sleep disrupts autonomic nervous system function, which regulates blood pressure and heart rate. Chronic sleep deprivation can lead to dizziness, brain fog, and imbalance.
Is lightheadedness a sign of anxiety?
It can be. Anxiety triggers the fight-or-flight response, increasing heart rate and altering breathing. Hyperventilation reduces carbon dioxide in the blood, leading to dizziness, tingling, and lightheadedness.
Why do I get dizzy when I stand up?
This is often orthostatic hypotension—your blood pressure drops temporarily upon standing. It’s common in older adults, those on blood pressure medication, or individuals who are dehydrated. Rising slowly can help prevent it.
Conclusion: Take Control of Your Balance and Health
Lightheadedness is more than just a fleeting annoyance—it’s a signal from your body that something may be off. While many causes are manageable with simple lifestyle changes, ignoring persistent or severe symptoms risks missing serious conditions.
You don’t have to live with constant dizziness. Start by paying attention to your body’s cues, making sustainable adjustments, and seeking professional guidance when needed. Small steps today can lead to greater stability, energy, and confidence tomorrow.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?