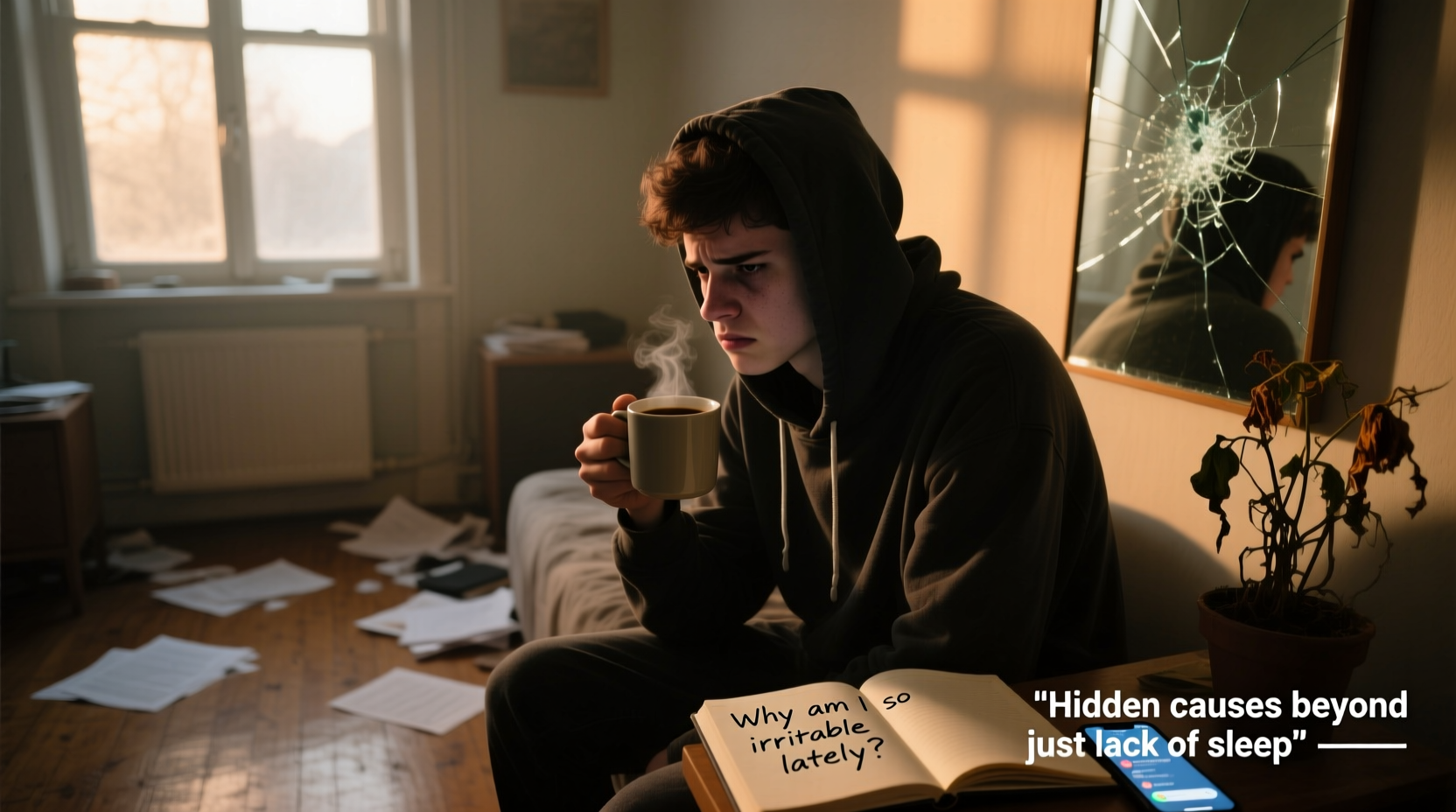
If you've found yourself snapping at coworkers, frustrated by small inconveniences, or feeling emotionally raw without clear reason, you're not alone. Irritability is one of the most common yet misunderstood emotional states. While lack of sleep is a well-known trigger, it's far from the only—or even the primary—culprit behind sudden mood shifts. Persistent irritability can signal deeper imbalances in your body, mind, and lifestyle. Understanding these underlying causes is the first step toward restoring calm, clarity, and emotional resilience.
Hormonal Fluctuations: The Silent Mood Modulators
Hormones play a pivotal role in regulating mood, energy, and emotional stability. Even subtle imbalances can lead to noticeable irritability, especially when they go unnoticed for weeks or months.
For women, hormonal shifts during the menstrual cycle, perimenopause, or postpartum periods often manifest as increased sensitivity and frustration. Estrogen and progesterone influence serotonin and GABA—neurotransmitters responsible for feelings of well-being and relaxation. When these hormones fluctuate, so can your emotional threshold.
Men aren't exempt either. Declining testosterone levels with age, particularly after 40, can contribute to mood swings, low motivation, and irritability. Similarly, thyroid dysfunction—whether hypothyroidism (underactive) or hyperthyroidism (overactive)—can mimic symptoms of anxiety and agitation.
“Many patients come in thinking they’re just stressed or tired, but their blood work reveals thyroid imbalances or sex hormone irregularities that explain their irritability.” — Dr. Lena Patel, Integrative Endocrinologist
Nutritional Deficiencies and Blood Sugar Swings
Your brain runs on nutrients and stable energy. When your diet lacks essential vitamins or causes erratic blood sugar levels, your mood pays the price.
Magnesium, vitamin D, B12, and omega-3 fatty acids are critical for nervous system function. Deficiency in any of these can impair neurotransmitter production and increase inflammatory markers linked to mood disorders. For example, low magnesium is associated with heightened stress reactivity and reduced GABA activity—making it harder to \"turn off\" the fight-or-flight response.
Equally disruptive are blood sugar fluctuations. Skipping meals, relying on refined carbohydrates, or consuming excessive caffeine can cause rapid spikes and crashes in glucose levels. These swings directly impact brain chemistry, leading to symptoms like brain fog, anxiety, and—yes—irritability.
| Nutrient | Role in Mood Regulation | Common Deficiency Signs |
|---|---|---|
| Magnesium | Supports nerve function and GABA production | Muscle tension, insomnia, anxiety |
| Vitamin D | Modulates dopamine and serotonin | Fatigue, low mood, seasonal depression |
| Omega-3s | Reduce brain inflammation, support neuron health | Poor focus, mood swings |
| B12 | Essential for myelin and neurotransmitter synthesis | Low energy, memory issues, tingling |
Chronic Stress and Nervous System Overload
Modern life keeps many people in a prolonged state of sympathetic activation—the “fight-or-flight” mode. When stress becomes chronic, the nervous system doesn’t get the signal to return to rest-and-digest (parasympathetic) mode. This dysregulation manifests as irritability, hypervigilance, and emotional exhaustion.
Cortisol, the primary stress hormone, should follow a natural rhythm: high in the morning, tapering off at night. But constant stress flattens this curve, leaving cortisol elevated late into the day. This disrupts sleep, suppresses immune function, and lowers the threshold for frustration.
Moreover, chronic stress depletes neurotransmitters like serotonin and dopamine over time. Without adequate recovery, even minor inconveniences can feel overwhelming.
Mini Case Study: The Breaking Point of a High-Achiever
Sarah, a 34-year-old project manager, began snapping at her team during meetings. She attributed it to being “overtired,” but even after improving her sleep, the irritability persisted. After consulting a functional medicine practitioner, she discovered elevated cortisol levels and low DHEA—a marker of adrenal fatigue. Her routine included early mornings, back-to-back Zoom calls, skipped lunches, and evening wine to unwind. Though she wasn’t clinically depressed, her nervous system was in survival mode. With dietary changes, daily mindfulness practice, and adaptogenic herbs, Sarah reported a dramatic improvement in emotional regulation within six weeks.
Hidden Inflammation and Gut Health Connections
The gut-brain axis is now recognized as a major pathway influencing mood. An unhealthy gut microbiome can promote systemic inflammation, which has been directly linked to increased irritability and depressive symptoms.
Dysbiosis—an imbalance of gut bacteria—can result from poor diet, antibiotic use, or chronic stress. When harmful bacteria dominate, they produce endotoxins like lipopolysaccharides (LPS), which cross into the bloodstream and trigger neuroinflammation. This inflammation interferes with serotonin production (95% of which occurs in the gut) and impairs the blood-brain barrier.
Food sensitivities also play a role. Common triggers like gluten, dairy, or processed foods may not cause obvious digestive symptoms but can still provoke low-grade immune responses that affect the brain. Many people report improved mood simply by eliminating inflammatory foods—even without diagnosed allergies.
Medication Side Effects and Environmental Toxins
Some medications list irritability as a side effect, including certain antidepressants, stimulants, corticosteroids, and even hormonal contraceptives. Birth control pills, for instance, can lower zinc and B6 levels while altering estrogen metabolism, both of which impact mood stability.
Environmental factors are equally overlooked. Exposure to mold (especially in water-damaged buildings), heavy metals (like lead or mercury), or endocrine-disrupting chemicals (such as BPA or phthalates in plastics) can interfere with neurological and hormonal function. These toxins accumulate over time and may not present with classic illness symptoms, yet quietly erode emotional well-being.
“We’re seeing more patients with ‘idiopathic’ irritability who test positive for mycotoxins or elevated urinary bisphenols. Once we address the exposure, their mood improves significantly.” — Dr. Rafael Torres, Environmental Medicine Specialist
Step-by-Step Guide to Identifying Your Irritability Triggers
Irritability rarely has a single cause. A systematic approach helps isolate contributing factors and build a personalized recovery plan.
- Track Your Mood Daily: Use a journal or app to record irritability episodes, noting time, context, food intake, sleep quality, and stressors.
- Review Medications and Supplements: Check labels or consult your doctor about potential mood-altering side effects.
- Assess Diet Patterns: Identify reliance on caffeine, sugar, or processed foods. Note if mood dips occur after meals.
- Order Key Lab Tests: Request tests for vitamin D, B12, magnesium, thyroid panel (TSH, free T3/T4), cortisol rhythm, and possibly food sensitivities.
- Evaluate Your Environment: Consider indoor air quality, mold history, plastic use, and chemical exposures at home or work.
- Implement One Change at a Time: Adjust diet, add magnesium, reduce screen time before bed, or start breathwork. Monitor effects over 2–3 weeks.
Checklist: Actions to Reduce Unexplained Irritability
- ✅ Get tested for vitamin D, B12, magnesium, and thyroid function
- ✅ Eat balanced meals every 3–4 hours to stabilize blood sugar
- ✅ Limit caffeine to before 12 PM and avoid alcohol as a coping tool
- ✅ Practice diaphragmatic breathing for 5 minutes daily
- ✅ Remove known inflammatory foods for a 3-week trial
- ✅ Assess your living space for mold, poor ventilation, or chemical cleaners
- ✅ Schedule 10 minutes of digital detox each evening
- ✅ Talk to your doctor about medication side effects
When Emotional Health Crosses Into Clinical Territory
While irritability is a normal human experience, persistent or severe mood disturbances may indicate an underlying mental health condition. Generalized anxiety disorder, ADHD, bipolar disorder, and even early-stage depression often present with irritability—especially in men or older adults who may not exhibit classic sadness.
Depression, for example, frequently manifests as anger, frustration, or emotional numbness rather than overt sadness. If irritability is accompanied by loss of interest, changes in appetite, hopelessness, or difficulty concentrating, professional evaluation is crucial.
Similarly, undiagnosed ADHD in adults can appear as chronic impatience, emotional dysregulation, and frustration with routine tasks. These symptoms are often mistaken for personality flaws rather than neurodevelopmental differences.
FAQ
Can dehydration really make me more irritable?
Yes. Even mild dehydration (as little as 1–2% fluid loss) impairs cognitive performance and increases perceived task difficulty. The brain responds to dehydration with heightened stress signals, lowering your tolerance for frustration. Aim for at least 2 liters of water daily, more if active or in hot climates.
Is there a link between screen time and irritability?
Absolutely. Excessive screen exposure—especially blue light at night—disrupts melatonin production and circadian rhythms. It also overstimulates the visual cortex and reduces opportunities for reflective downtime. Studies show that reducing screen time, particularly before bed, leads to improved emotional regulation and reduced reactivity.
How long does it take to see improvements in mood after making lifestyle changes?
Most people notice subtle shifts within 2–3 weeks of consistent changes—like better sleep, reduced sugar intake, or daily mindfulness. However, full neurochemical and hormonal rebalancing can take 3–6 months. Patience and consistency are key.
Conclusion
Irritability is rarely just about being “short-tempered” or “needing more sleep.” It’s a signal—one that deserves attention, not dismissal. By looking beyond surface-level explanations, you open the door to meaningful solutions: balancing hormones, nourishing your brain, calming your nervous system, and cleaning up environmental inputs. These changes don’t require drastic overhauls. Small, sustained actions compound into profound shifts in emotional well-being.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?