Feeling unsteady on your feet, lightheaded when standing, or struggling to maintain coordination during routine activities? You're not alone. Balance issues affect millions of people across all age groups—not just the elderly. While occasional dizziness may seem harmless, persistent imbalance can signal underlying health concerns that deserve attention. Understanding the root causes and knowing how to respond can make a significant difference in your daily well-being and long-term mobility.
Understanding the Body’s Balance System
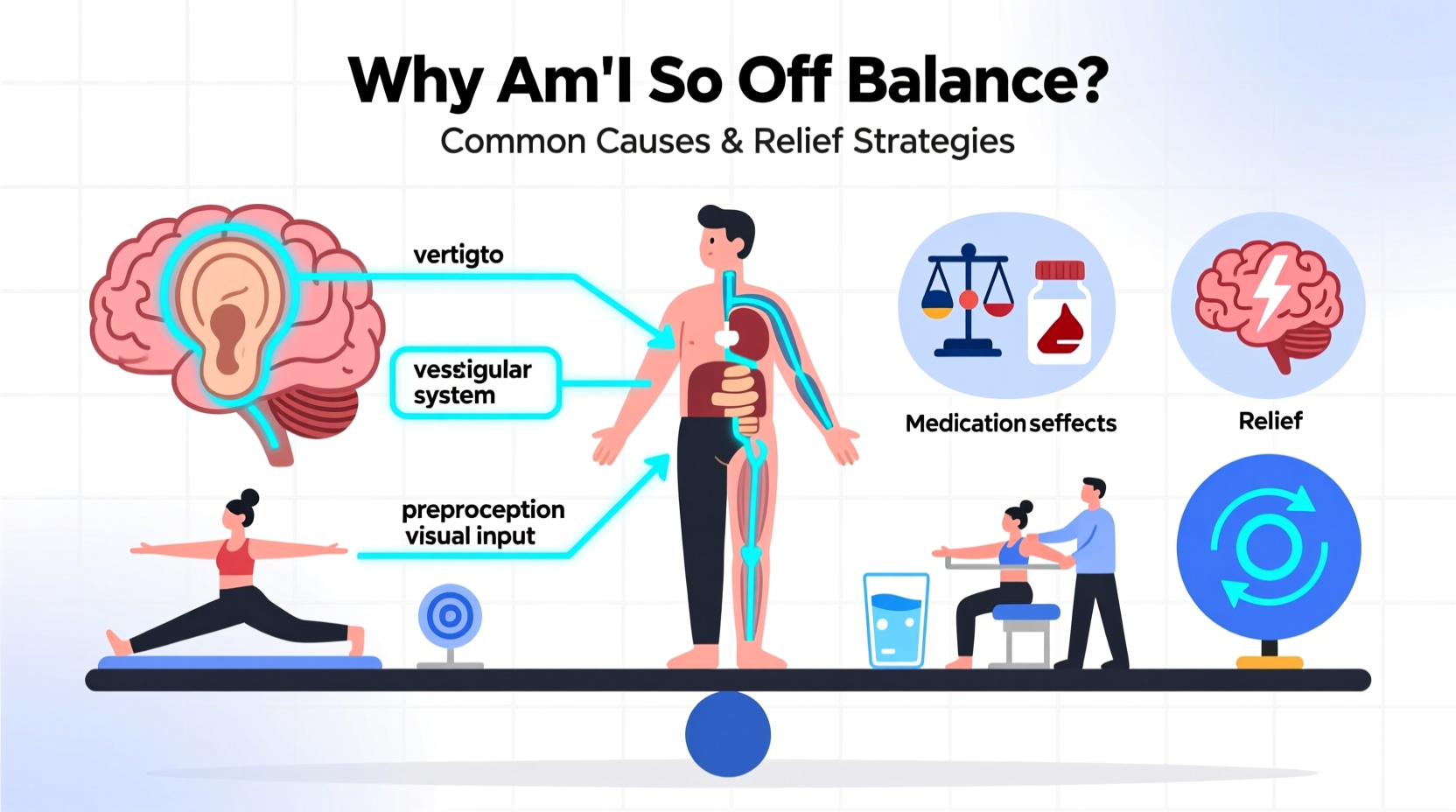
Balancing on two feet is a complex process involving multiple systems working in harmony: the inner ear (vestibular system), vision, and sensory feedback from muscles and joints (proprioception). The brain integrates signals from these sources to maintain posture, coordinate movement, and prevent falls. When one component falters, the entire system can be disrupted—leading to feelings of dizziness, swaying, or vertigo.
For example, if your inner ear detects motion but your eyes see stillness (as in motion sickness), conflicting signals confuse the brain. Similarly, poor joint sensation due to nerve damage can leave the brain \"blind\" to limb position, increasing fall risk. Recognizing how these systems interact helps explain why balance disorders are often multifactorial.
“Balance isn’t just about strength—it’s a neurological symphony. Even subtle disruptions in one area can throw off the whole performance.” — Dr. Lena Torres, Neurotologist at Boston Balance Institute
Common Causes of Balance Problems
Imbalance rarely has a single cause. Instead, it's typically the result of overlapping physical, neurological, or environmental factors. Below are some of the most frequent contributors:
- Vestibular disorders: Conditions like benign paroxysmal positional vertigo (BPPV), Meniere’s disease, or vestibular neuritis disrupt inner ear function, leading to sudden spinning sensations.
- Neurological conditions: Multiple sclerosis, Parkinson’s disease, stroke, or peripheral neuropathy interfere with nerve signaling essential for coordination.
- Muscle weakness or joint instability: Aging, inactivity, or injury can weaken core and lower-limb muscles critical for stability.
- Medication side effects: Blood pressure drugs, sedatives, antidepressants, and anticonvulsants may impair alertness or blood flow to the brain.
- Low blood pressure: Especially upon standing (orthostatic hypotension), this can cause dizziness due to reduced cerebral perfusion.
- Dehydration or low blood sugar: Simple metabolic imbalances can trigger lightheadedness and unsteadiness.
- Poor vision: Cataracts, glaucoma, or uncorrected prescriptions reduce spatial awareness.
When to Seek Medical Help
Not every bout of dizziness requires emergency care, but certain red flags should prompt immediate evaluation:
- Sudden onset of severe vertigo lasting more than a few minutes
- Double vision, slurred speech, or facial drooping (possible stroke signs)
- Chest pain or irregular heartbeat accompanying dizziness
- Frequent unexplained falls
- Hearing loss or ringing in ears alongside imbalance
A primary care physician may refer you to an ENT specialist, neurologist, or physical therapist depending on suspected origin. Diagnostic tools such as vestibular testing, MRI scans, or gait analysis help pinpoint the issue.
Effective Relief Strategies and Daily Adjustments
Treatment depends on the diagnosis, but many balance problems improve with targeted interventions. Here’s a practical roadmap for managing and reducing symptoms:
Step-by-Step Guide to Improving Balance
- Consult a healthcare provider to rule out serious conditions and identify contributing factors.
- Begin vestibular rehabilitation therapy (VRT) if inner ear dysfunction is diagnosed. These customized exercises retrain the brain to compensate for faulty signals. <3> Strengthen key muscle groups through regular exercise focusing on legs, core, and hips. Simple routines like heel-to-toe walking or single-leg stands build stability.
- Review medications with your doctor to assess whether any are contributing to dizziness.
- Stay hydrated and eat balanced meals to avoid drops in blood sugar or volume that impair equilibrium.
- Improve home safety by removing tripping hazards, installing grab bars, and ensuring adequate lighting.
| Do’s | Don’ts |
|---|---|
| Move slowly when changing positions (sit to stand) | Rush from lying down to standing up |
| Use a cane or walker if recommended | Ignore repeated near-falls |
| Wear supportive, non-slip footwear | Walk barefoot on slick surfaces |
| Practice balance exercises daily | Isolate yourself out of fear of falling |
Real Example: Maria’s Recovery Journey
Maria, a 62-year-old teacher, began experiencing episodes of room-spinning dizziness whenever she turned her head quickly or got up from bed. After an initial panic attack-like episode, she visited her doctor, who referred her to an audiologist. Testing confirmed BPPV in her right ear. She underwent the Epley maneuver—a series of guided head movements—and completed three sessions of vestibular rehab over six weeks. Within two months, her vertigo resolved, and she regained confidence walking and driving. “I didn’t realize something so fixable was making me feel so broken,” she said.
Prevention Checklist: Maintain Stability Long-Term
Even if you’ve never fallen, proactive habits protect future balance. Use this checklist to stay steady:
- ✅ Schedule annual eye and hearing exams
- ✅ Monitor blood pressure regularly, especially if on medication
- ✅ Engage in balance-focused activities like tai chi or yoga twice weekly
- ✅ Limit alcohol and avoid smoking—both harm circulation and neural function
- ✅ Keep floors clear of clutter and rugs secured
- ✅ Rise slowly after sitting or lying down
- ✅ Stay socially active—mental engagement supports motor control
Frequently Asked Questions
Can anxiety cause balance problems?
Yes. Anxiety and panic disorders can lead to hyperventilation, muscle tension, and heightened sensitivity to motion, all of which mimic or worsen dizziness. However, it’s crucial to first rule out physical causes before attributing imbalance solely to stress.
Are balance issues normal with aging?
While more common with age, they are not inevitable. Some decline in reflex speed or joint sensitivity occurs naturally, but significant imbalance should never be dismissed as “just getting older.” Early intervention can prevent disability.
What exercises help with balance?
Proven options include standing on one foot (progressively longer durations), heel-to-toe walks along a line, seated marches, and tai chi—all shown to enhance neuromuscular coordination. Always start with support nearby until confident.
Take Control of Your Stability Today
Feeling off balance doesn’t have to become your new normal. Whether your symptoms stem from a temporary inner ear glitch or a chronic condition, actionable solutions exist. From medical treatments to lifestyle tweaks, regaining stability starts with awareness and commitment. Don’t wait for a fall to take action—your body’s ability to adapt is remarkable when given the right support.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?