Nasal congestion—commonly known as a stuffy nose—is one of the most frequent complaints during cold season, allergy flare-ups, or even in dry climates. While it may seem like a minor inconvenience, persistent stuffiness can disrupt sleep, impair concentration, and diminish quality of life. Understanding what’s really behind that blocked nose is the first step toward lasting relief. The causes range from temporary viral infections to chronic structural issues, and treatment varies accordingly. This guide breaks down the root causes of nasal congestion and offers practical, evidence-based solutions for immediate and long-term comfort.
Understanding Nasal Congestion: What Happens When You’re Stuffy?
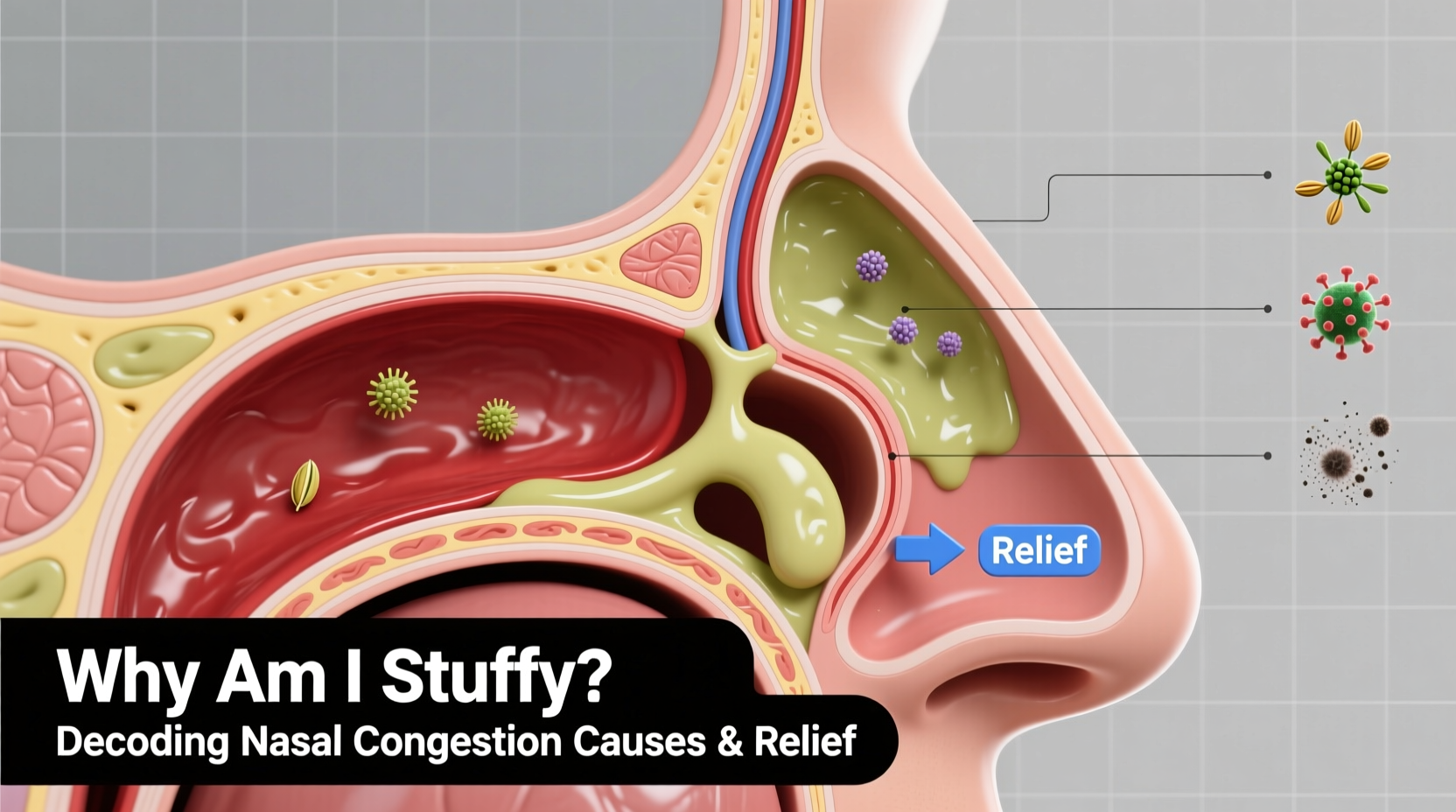
Nasal congestion occurs when the tissues lining the nasal passages become inflamed and swollen. Blood vessels in the nose expand in response to irritation, infection, or allergens, leading to increased mucus production and a sensation of blockage. It's not always due to excess mucus; sometimes, airflow is restricted simply because the nasal tissues are engorged.
The condition can be unilateral (affecting one side) or bilateral (both sides), intermittent or chronic. Acute congestion typically lasts less than four weeks and is often linked to infections or short-term allergen exposure. Chronic congestion persists beyond a month and may signal underlying conditions such as deviated septum, chronic sinusitis, or hormonal imbalances.
Common Causes of Nasal Congestion
The reasons behind a stuffy nose are diverse. Identifying the trigger is essential for choosing the right treatment.
1. Viral Infections (Colds and Flu)
The most common cause of temporary nasal congestion is a viral upper respiratory infection. Rhinoviruses, influenza, and coronaviruses trigger inflammation in the nasal mucosa, leading to swelling, mucus buildup, and postnasal drip. Symptoms usually peak within 2–3 days and resolve within 7–10 days.
2. Allergies (Allergic Rhinitis)
Seasonal or perennial allergies occur when the immune system overreacts to harmless substances like pollen, dust mites, mold, or pet dander. This reaction releases histamine, causing nasal swelling, sneezing, and watery discharge. Unlike colds, allergic congestion often comes with itchy eyes and throat and tends to last as long as exposure continues.
3. Sinus Infections (Sinusitis)
When nasal congestion persists beyond 10 days or worsens after initial improvement, a bacterial sinus infection may be developing. Sinusitis involves inflammation of the sinuses, often accompanied by facial pain, thick yellow or green mucus, and reduced sense of smell.
4. Environmental Irritants
Smoke, strong perfumes, chemical fumes, and dry air can irritate nasal membranes and provoke congestion—even without an allergic response. Indoor heating systems in winter reduce humidity, drying out nasal passages and prompting reactive swelling.
5. Structural Abnormalities
Some people experience chronic stuffiness due to anatomical factors. A deviated septum, nasal polyps, or enlarged turbinates physically obstruct airflow. These issues may require medical evaluation or surgical correction.
6. Hormonal Changes
Pregnancy, menstruation, and thyroid disorders can influence nasal blood flow and mucosal swelling. “Pregnancy rhinitis” affects up to 30% of expectant mothers, typically in the second trimester, due to elevated estrogen levels increasing vascular congestion in nasal tissues.
7. Medication Side Effects
Overuse of nasal decongestant sprays (like oxymetazoline) can lead to rebound congestion, known as rhinitis medicamentosa. Certain blood pressure medications, antidepressants, and oral contraceptives may also contribute to nasal stuffiness.
“Persistent nasal congestion should never be ignored. It can be a sign of something more than just a cold—especially if it affects only one side or is accompanied by loss of smell.” — Dr. Lena Patel, Otolaryngologist
Effective Relief Strategies: From Home Remedies to Medical Treatments
Treatment depends on the underlying cause. Here’s how to find relief based on your situation.
Immediate Home-Based Relief
- Saline nasal irrigation: Using a neti pot or saline spray helps flush out allergens, thin mucus, and reduce inflammation.
- Steam inhalation: Breathing warm, moist air from a bowl of hot water or shower can loosen mucus and soothe irritated tissues.
- Hydration: Drinking plenty of fluids keeps mucus thin and easier to drain.
- Elevate your head: Sleeping with an extra pillow reduces nighttime congestion by improving sinus drainage.
Over-the-Counter (OTC) Options
| Medication Type | Best For | Caution |
|---|---|---|
| Oral decongestants (e.g., pseudoephedrine) | Short-term relief of cold or allergy congestion | Avoid if you have high blood pressure or heart conditions |
| Antihistamines (e.g., loratadine, cetirizine) | Allergic rhinitis with sneezing and runny nose | May cause drowsiness (especially older types like diphenhydramine) |
| Nasal corticosteroid sprays (e.g., fluticasone) | Chronic allergies or inflammation | Takes several days to reach full effect; safe for long-term use |
| Decongestant nasal sprays (e.g., Afrin) | Fast relief for severe congestion | Limited to 3 days to avoid rebound congestion |
Step-by-Step Guide to Managing Nasal Congestion
- Identify the cause: Track symptoms—duration, triggers, associated signs (fever, itching, facial pain)—to determine whether it’s a cold, allergy, or structural issue.
- Start with conservative care: Use saline rinses, steam, and hydration for at least 48 hours before turning to medication.
- Choose appropriate OTC treatment: Opt for antihistamines for allergies, decongestants for short-term viral congestion, or steroid sprays for ongoing inflammation.
- Monitor progress: If symptoms persist beyond 10 days, worsen, or include high fever or facial swelling, consult a healthcare provider.
- Consider professional evaluation: For chronic or one-sided congestion, see an ENT specialist to rule out polyps, deviated septum, or other structural concerns.
Real-Life Example: Sarah’s Seasonal Struggle
Sarah, a 34-year-old teacher, began experiencing daily nasal congestion every spring. She assumed it was just “bad weather,” but her symptoms included itchy eyes, fatigue, and constant throat clearing. Over-the-counter cold medicines didn’t help. After tracking her symptoms and noticing they coincided with tree pollen counts, she consulted an allergist. Skin testing confirmed sensitivity to birch and oak pollen. With a prescription nasal steroid and advice to keep windows closed during high pollen days, her congestion resolved within two weeks. The key was identifying the true cause—seasonal allergic rhinitis—instead of treating it like a recurring cold.
Checklist: When to Seek Medical Help
- ☑ Congestion lasting more than 10 days without improvement
- ☑ Facial pain or pressure with thick, discolored nasal discharge
- ☑ Loss of smell or taste
- ☑ One-sided nasal blockage, especially if persistent
- ☑ Frequent nosebleeds or visible nasal deformity
- ☑ Symptoms interfering with sleep or daily function despite home care
Frequently Asked Questions
Can dehydration make nasal congestion worse?
Yes. Dehydration thickens mucus, making it harder to drain and increasing the sensation of blockage. Staying well-hydrated helps keep secretions thin and promotes natural clearance.
Is it possible to be “stuffy” without having a runny nose?
Absolutely. Swollen nasal tissues can block airflow even if mucus production is minimal. This is common in non-allergic rhinitis, dry air exposure, or early stages of a cold.
Are nasal strips effective for congestion?
Nasal strips can help some people by gently pulling open the external nasal passages during sleep, improving airflow. They don’t treat inflammation but may offer mechanical relief, especially for snoring or positional congestion.
Take Control of Your Breathing
Being stuffy isn’t something you have to endure. Whether your congestion stems from a passing cold, seasonal allergies, or a deeper anatomical issue, there are effective ways to regain clear breathing and comfort. Start with simple, natural remedies and track your symptoms carefully. When needed, use targeted medications wisely and know when to seek expert care. Small changes—like using a humidifier, avoiding irritants, or starting a nasal spray routine before allergy season—can make a big difference. Don’t ignore chronic stuffiness; understanding the “why” behind your congestion is the key to lasting relief.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?