Waking up to vomit that looks like white or yellowish foam can be alarming. It’s not a typical symptom most people expect, and when it happens repeatedly, it raises serious concerns. While occasional foamy vomit may stem from something as simple as an empty stomach, persistent episodes could signal underlying digestive issues. Understanding why this occurs—and knowing how to respond—is essential for both immediate relief and long-term health.
Foam in vomit usually results from a mix of air, mucus, and gastric fluids. When your stomach is empty, bile and digestive enzymes can combine with saliva and air, creating a frothy appearance. However, multiple factors ranging from acid reflux to more severe gastrointestinal conditions can contribute. This article explores the primary causes, symptoms to watch for, and practical steps you can take to manage and prevent recurrence.
Common Causes of Foamy Vomiting
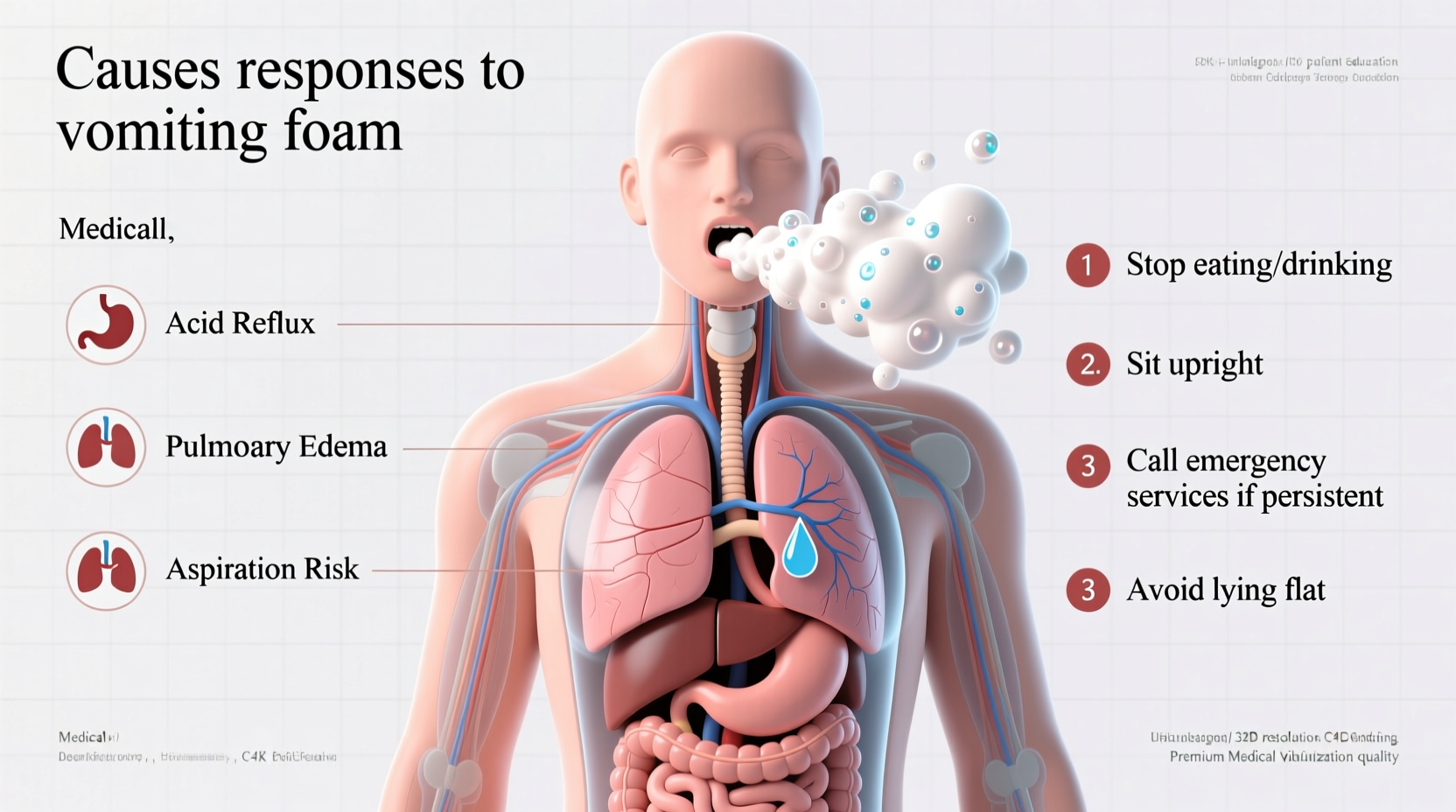
Several physiological and lifestyle-related factors can lead to vomiting foam. Identifying the root cause is crucial in determining whether home care is sufficient or if medical evaluation is necessary.
- Empty Stomach Vomiting: When you vomit on an empty stomach, there’s little solid content to expel. The body instead brings up gastric juices, mucus, and air—mixing into a foamy substance.
- Gastroesophageal Reflux Disease (GERD): Chronic acid reflux allows stomach acid to back up into the esophagus. In severe cases, especially during sleep, this can result in regurgitation of frothy, bitter-tasting fluid.
- Excessive Alcohol Consumption: Alcohol irritates the stomach lining and increases acid production. Heavy drinking, particularly on an empty stomach, can trigger nausea and foamy vomiting.
- Pancreatitis: Inflammation of the pancreas often presents with severe abdominal pain, nausea, and vomiting—sometimes including foamy or frothy discharge, especially if bile is involved.
- Intestinal Obstruction: A partial or complete blockage in the intestines can cause vomiting of a greenish or foamy substance due to bile accumulation.
- Hiatal Hernia: When part of the stomach pushes through the diaphragm, it can disrupt normal digestion and promote reflux, leading to foamy regurgitation.
Symptoms That Warrant Immediate Medical Attention
Not all cases of foamy vomiting are emergencies, but certain accompanying symptoms should prompt urgent care. These may indicate serious conditions such as bowel obstruction, pancreatitis, or gastritis with bleeding.
“Persistent vomiting of foam, especially when paired with severe pain or dehydration, should never be ignored. It can be a sign of significant gastrointestinal distress.” — Dr. Lena Patel, Gastroenterologist
Seek medical help immediately if you experience any of the following:
- Severe or worsening abdominal pain
- Vomiting blood or material resembling coffee grounds
- Inability to keep liquids down for more than 12 hours
- Signs of dehydration (dry mouth, dizziness, reduced urination)
- Fever over 101°F (38.3°C)
- Swollen or rigid abdomen
Do’s and Don’ts: Managing Foamy Vomiting at Home
For mild, infrequent episodes linked to diet or temporary illness, home management can provide relief. However, doing the wrong thing may worsen symptoms.
| Do’s | Don’ts |
|---|---|
| Stay hydrated with small sips of water, electrolyte drinks, or ice chips | Drink large amounts of fluid at once—this can trigger more vomiting |
| Eat bland foods like rice, bananas, or toast once nausea subsides | Consume spicy, fatty, or acidic foods too soon |
| Rest in an upright position to reduce acid reflux | Lie flat immediately after eating or vomiting |
| Use over-the-counter antacids if heartburn is present | Take NSAIDs like ibuprofen, which can further irritate the stomach |
| Monitor symptoms for changes over 24–48 hours | Ignore worsening symptoms or assume it will “pass on its own” |
Step-by-Step Guide to Responding to Foamy Vomiting
If you find yourself vomiting foam, follow this structured approach to assess severity and take appropriate action:
- Pause and Assess: Note the color and consistency of the foam. Is it clear, white, yellow, or green? Yellow or green may indicate bile, suggesting possible intestinal involvement.
- Hydrate Gradually: After vomiting stops, wait 30 minutes, then sip small amounts of water or oral rehydration solution every 5–10 minutes.
- Avoid Eating Immediately: Wait at least 1–2 hours before trying light, bland food. Start with a few saltine crackers or a banana.
- Elevate Your Head: If lying down, use pillows to keep your head above your stomach to minimize acid reflux.
- Track Symptoms: Keep a log of when vomiting occurs, what you ate, and any other symptoms (pain, fever, etc.). This helps doctors make a diagnosis.
- Determine Need for Medical Care: If symptoms persist beyond 24 hours, worsen, or include red flags (pain, blood, dehydration), contact a healthcare provider or visit urgent care.
Real-Life Example: A Case of Misdiagnosed Morning Foam
Sarah, a 34-year-old teacher, began waking up several mornings in a row with a sour taste in her mouth and traces of white foam on her pillow. She assumed it was postnasal drip or mild indigestion. Over two weeks, the episodes increased, and she developed a burning sensation in her chest. She tried antacids with limited success.
After consulting her doctor, she was diagnosed with nocturnal GERD exacerbated by late-night meals and stress. Her treatment plan included dietary adjustments, elevating the head of her bed, and taking a proton pump inhibitor at night. Within two weeks, her symptoms resolved completely.
Sarah’s case illustrates how seemingly minor symptoms like foamy regurgitation can point to chronic conditions that benefit from early intervention.
Prevention Strategies and Long-Term Care
Preventing recurrent foamy vomiting involves managing triggers and supporting digestive health. For many, lifestyle changes make a dramatic difference.
- Eat Smaller, Frequent Meals: Large meals increase stomach pressure and the risk of reflux.
- Avoid Late-Night Eating: Finish eating at least 2–3 hours before bedtime to allow digestion to begin.
- Limit Alcohol and Caffeine: Both relax the lower esophageal sphincter and stimulate acid production.
- Manage Stress: Chronic stress can affect gut motility and acid secretion. Techniques like meditation, breathing exercises, or yoga may help.
- Maintain a Healthy Weight: Excess abdominal fat increases pressure on the stomach, promoting reflux.
Frequently Asked Questions
Is throwing up foam always a sign of a serious condition?
No. Occasional foamy vomit, especially after drinking alcohol or on an empty stomach, is usually not dangerous. However, frequent or persistent episodes should be evaluated by a doctor.
Can acid reflux cause me to vomit foam in the morning?
Yes. Nocturnal acid reflux can lead to regurgitation of stomach contents, including foam, while you're asleep. This is often accompanied by a sour or bitter taste.
What does yellow foam in vomit mean?
Yellow foam typically contains bile, a digestive fluid produced by the liver. It may appear when the stomach is empty or in cases of intestinal issues like obstruction or delayed gastric emptying.
Conclusion: Take Action Before It Escalates
Vomiting foam isn’t something to dismiss lightly, even if it seems minor at first. While many causes are manageable with lifestyle changes, others require medical diagnosis and treatment. Pay attention to your body’s signals, act early, and don’t hesitate to seek professional guidance when symptoms persist.
Small adjustments—like changing your eating schedule, reducing alcohol intake, or elevating your bed—can have a profound impact on your digestive comfort. If you’ve been experiencing this symptom regularly, now is the time to take control. Your gut health matters, and addressing issues early can prevent long-term complications.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?