Amitriptyline, a tricyclic antidepressant developed in the 1960s, remains in clinical use today for treating depression, chronic pain, migraines, and certain sleep disorders. While effective for many patients, its use carries significant risks that demand careful consideration. Unlike newer antidepressants, amitriptyline affects multiple neurotransmitter systems, which increases both its therapeutic potential and its danger profile. This broad mechanism of action contributes to why amitriptyline can be high risk—especially when used without proper monitoring or at higher-than-recommended doses.
The drug’s ability to influence serotonin, norepinephrine, histamine, and acetylcholine receptors means it can produce widespread physiological effects. These include not only mood stabilization but also sedation, dry mouth, constipation, blurred vision, and cardiac changes. For some patients, particularly older adults or those with pre-existing health conditions, these effects can escalate into life-threatening complications.
Mechanism of Action and Systemic Impact
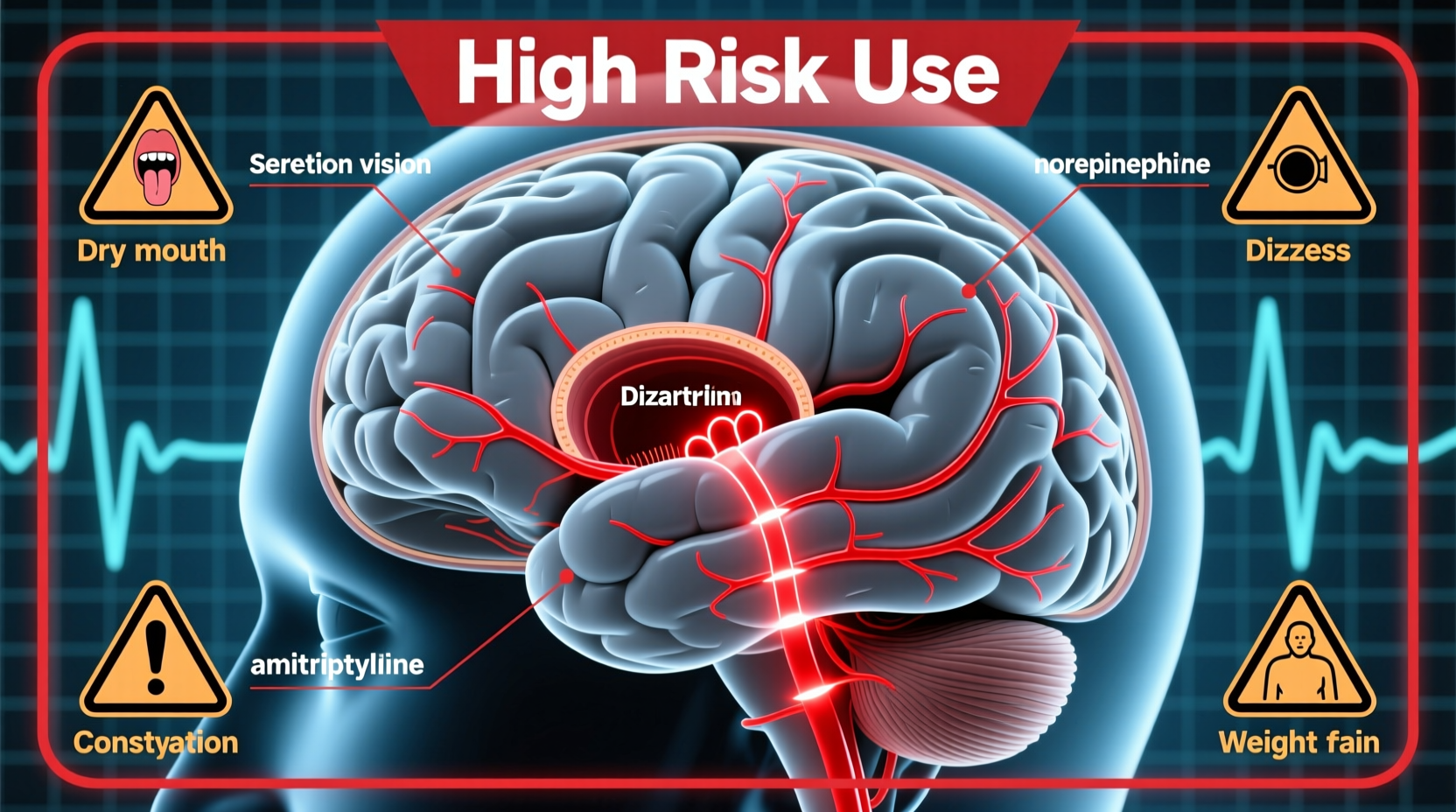
Amitriptyline primarily works by inhibiting the reuptake of serotonin and norepinephrine in the brain, enhancing their availability and improving mood regulation. However, it also blocks several other receptor types:
- Anticholinergic receptors: Causes dry mouth, urinary retention, constipation, and cognitive fog.
- Alpha-1 adrenergic receptors: Leads to orthostatic hypotension (a sudden drop in blood pressure upon standing).
- Histamine (H1) receptors: Results in pronounced drowsiness and weight gain.
- Cardiac sodium channels: At high doses, this can disrupt heart rhythm, increasing the risk of arrhythmias.
This multi-receptor activity explains why amitriptyline has such a broad side effect profile. While low-dose use (e.g., 10–25 mg nightly) for nerve pain or insomnia may be well-tolerated, higher doses significantly increase the likelihood of adverse events.
“Tricyclics like amitriptyline are potent medications with narrow therapeutic windows. The line between benefit and toxicity can be thin, especially in vulnerable populations.” — Dr. Lena Reyes, Clinical Pharmacologist
Serious Side Effects and High-Risk Scenarios
Certain side effects associated with amitriptyline are not merely uncomfortable—they can be dangerous. The most concerning include:
- Cardiotoxicity: Amitriptyline can prolong the QT interval, leading to torsades de pointes, a potentially fatal arrhythmia. This risk is heightened in patients with pre-existing heart disease or electrolyte imbalances.
- Orthostatic hypotension: Sudden drops in blood pressure increase fall risk, particularly in elderly patients.
- Anticholinergic delirium: Confusion, hallucinations, and memory issues can occur, especially in older adults. In severe cases, this mimics dementia.
- Seizure threshold reduction: Amitriptyline lowers the seizure threshold, posing a risk to individuals with epilepsy or brain injuries.
- Overdose potential: Even modest overdoses can be lethal due to cardiac conduction disturbances. It remains one of the most dangerous antidepressants in overdose scenarios.
Risk Factors That Amplify Danger
Not all patients face equal risk. Certain factors dramatically increase the likelihood of severe side effects:
| Risk Factor | Impact on Amitriptyline Safety |
|---|---|
| Age over 60 | Increased sensitivity to anticholinergic and cardiovascular effects; higher fall and delirium risk. |
| Heart disease | Elevated risk of arrhythmias and conduction delays. |
| Glaucoma | Can worsen angle-closure glaucoma due to pupil dilation. |
| Prostate enlargement | May cause acute urinary retention. |
| Concurrent use of CNS depressants | Increases sedation and respiratory depression risk (e.g., with opioids or benzodiazepines). |
Real-World Example: A Case of Anticholinergic Toxicity
Mr. Thompson, a 72-year-old man with diabetic neuropathy, was prescribed 50 mg of amitriptyline nightly for nerve pain. Within two weeks, he began experiencing confusion, inability to urinate, and episodes of dizziness upon standing. His family brought him to the emergency room, where he was diagnosed with anticholinergic delirium and acute urinary retention. After discontinuation of the drug and supportive care, his symptoms resolved over several days. This case illustrates how quickly amitriptyline can lead to serious complications in older adults, even at standard therapeutic doses.
Safe Use Guidelines and Monitoring Protocol
To mitigate risks, clinicians must follow strict prescribing practices. The following checklist outlines essential steps for safe amitriptyline use:
📋 Safe Use Checklist- Perform a baseline ECG in patients over 50 or with cardiac history.
- Avoid in patients with recent myocardial infarction, arrhythmias, or QT prolongation.
- Start low (e.g., 10–25 mg at bedtime) and titrate slowly.
- Assess renal and hepatic function—dose adjustments needed in impairment.
- Screen for glaucoma, BPH, and seizure disorders before prescribing.
- Monitor for signs of delirium, constipation, or orthostatic hypotension.
- Educate patients about overdose risks—store securely and never increase dose without consultation.
Step-by-Step: Initiating Amitriptyline Safely
- Week 1: Start with 10 mg at bedtime. Monitor for drowsiness and dizziness.
- Week 2: Assess tolerability. If no adverse effects, consider increasing to 25 mg if clinically indicated.
- Week 3–4: Re-evaluate symptom response and side effects. Further increases should be cautious and rare beyond 50 mg/day.
- Ongoing: Schedule follow-ups every 4–6 weeks. Check blood pressure, mental status, and bowel/bladder function.
- Discontinuation: Taper gradually over 2–4 weeks to avoid rebound insomnia or nausea.
Frequently Asked Questions
Can amitriptyline cause permanent damage?
In rare cases, prolonged use at high doses may contribute to cognitive decline in older adults due to cumulative anticholinergic burden. While not always permanent, some studies suggest an association between long-term anticholinergic use and increased dementia risk. Cardiac effects, if they lead to arrhythmias, can also result in lasting heart damage if untreated.
Is amitriptyline still prescribed despite the risks?
Yes, but selectively. It remains a valuable option for treatment-resistant depression, neuropathic pain, and migraine prevention—particularly when newer agents fail. Its sedative properties also make it useful for patients with comorbid insomnia. However, it is no longer a first-line treatment due to safety concerns.
What should I do if I miss a dose?
If you miss one dose, skip it and take the next dose at the regular time. Do not double up, as this increases the risk of side effects. Consistency is key, but abrupt changes in blood levels can trigger withdrawal-like symptoms such as headache or nausea.
Conclusion: Balancing Benefit and Risk
Amitriptyline exemplifies the delicate balance between therapeutic benefit and patient safety. Its broad pharmacological activity makes it effective for complex conditions, yet the same properties elevate its risk profile. When used appropriately—with careful patient selection, low starting doses, and vigilant monitoring—it can provide meaningful relief. But without these safeguards, the consequences can be severe.
Patients should never self-prescribe or adjust dosages without medical guidance. Physicians must weigh individual risk factors and consider safer alternatives—such as SSRIs or SNRIs—before initiating amitriptyline therapy. Open communication between patient and provider is essential to ensure that treatment remains both effective and safe.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?