The human respiratory system is a marvel of biological engineering, designed to extract oxygen from the air we breathe and expel carbon dioxide with remarkable efficiency. At the heart of this process lies the alveolus—tiny, balloon-like structures in the lungs where gas exchange occurs. One of the most distinctive features of these structures is the extreme thinness of their walls. But why are alveolar walls so thin? The answer lies in a combination of structural necessity, physiological demand, and evolutionary optimization for survival.
The Role of Alveoli in Gas Exchange
Alveoli are the terminal ends of the respiratory tree, clustered at the tips of bronchioles like bunches of grapes. Each adult human lung contains approximately 450 million alveoli, collectively creating a surface area of about 70 square meters—roughly the size of a tennis court. This vast surface area is essential for efficient gas exchange, but it's not just surface area that matters. The distance gases must travel between the air and the bloodstream is equally crucial.
Oxygen from inhaled air diffuses across the alveolar wall into the surrounding capillaries, where it binds to hemoglobin in red blood cells. Simultaneously, carbon dioxide—a waste product of metabolism—moves in the opposite direction, from the blood into the alveoli, to be exhaled. This entire process depends on passive diffusion, which is highly sensitive to distance: the shorter the path, the faster and more effective the transfer.
“Diffusion efficiency drops exponentially with distance. In the lungs, minimizing the barrier between air and blood was a key evolutionary breakthrough.” — Dr. Lena Torres, Pulmonary Biologist, University of Colorado
Anatomical Reasons for Thin Alveolar Walls
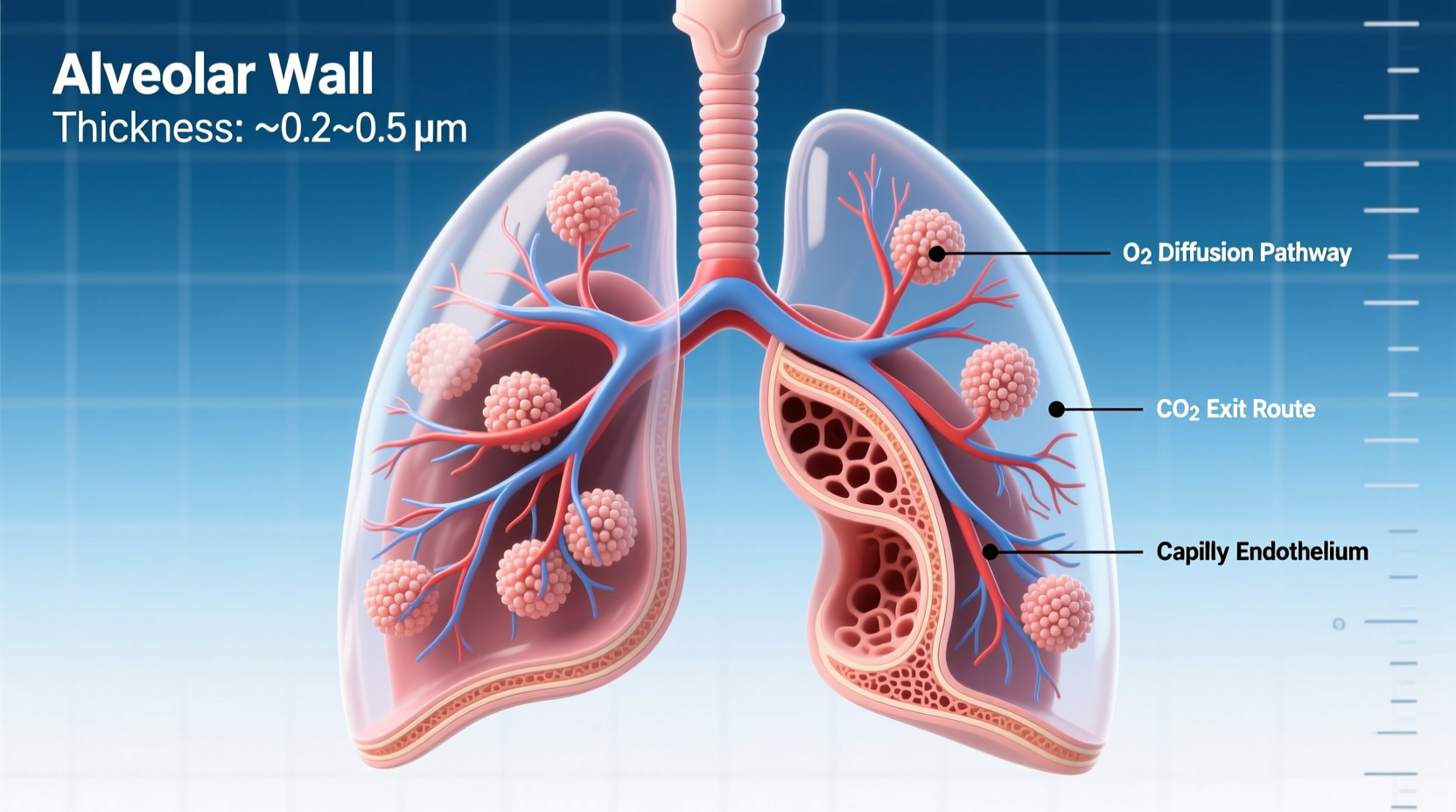
The alveolar wall, also known as the respiratory membrane, is composed of several ultra-thin layers:
- Type I pneumocytes: Flat, squamous epithelial cells that form the primary lining of the alveolus.
- Fused basement membranes: Shared by both alveolar and capillary endothelial cells.
- Capillary endothelial cells: Lining the pulmonary capillaries.
Together, these layers average only **0.2 to 0.5 micrometers** in thickness—about one-hundredth the width of a human hair. This minimal thickness drastically reduces the diffusion distance for oxygen and carbon dioxide, enabling rapid gas transfer even during high metabolic demand such as exercise.
Functional Advantages of Thin Alveolar Walls
The thinness of alveolar walls provides several key functional benefits:
- Maximized Diffusion Rate: According to Fick’s Law of Diffusion, the rate of gas transfer is inversely proportional to the thickness of the membrane. Thinner walls mean faster oxygen delivery to tissues.
- Energy Efficiency: Passive diffusion requires no cellular energy. A thin barrier allows the body to maintain gas exchange without expending ATP on active transport.
- High Surface Area-to-Thickness Ratio: The combination of enormous surface area and minimal thickness creates optimal conditions for bulk gas transfer per unit time.
- Responsive to Physiological Demand: During physical activity, cardiac output increases, and blood flows more rapidly through pulmonary capillaries. Thin walls ensure sufficient gas exchange even with shortened transit time.
This design allows humans to sustain aerobic activity far beyond what would be possible with thicker respiratory membranes.
How Structure Supports Function: A Closer Look
The architecture of the alveolar-capillary interface is a textbook example of structure-function correlation in biology. Consider the following anatomical adaptations:
| Feature | Description | Functional Benefit |
|---|---|---|
| Type I Pneumocytes | Extremely thin, flattened cells covering 95% of alveolar surface | Minimize diffusion distance |
| Fused Basement Membranes | Shared layer between alveolar and capillary cells | Reduces total barrier thickness |
| Dense Capillary Network | Each alveolus surrounded by 100s of capillaries | Maximizes contact between air and blood |
| Surfactant Secretion (by Type II cells) | Lipid-protein mix reducing surface tension | Prevents alveolar collapse, maintaining open diffusion pathways |
Consequences of Thickened Alveolar Walls
When the delicate alveolar structure is compromised, gas exchange suffers. Conditions such as interstitial lung disease, pulmonary fibrosis, or chronic inflammation cause scarring and thickening of the alveolar walls. This increases the diffusion distance, slowing oxygen transfer and resulting in hypoxemia—even when breathing room air.
In patients with idiopathic pulmonary fibrosis (IPF), for example, the alveolar wall can thicken up to 10 times its normal thickness. This leads to progressive shortness of breath, fatigue, and reduced exercise tolerance. Diagnosing such conditions often involves measuring diffusion capacity (DLCO), a test that directly assesses how well gases cross the alveolar-capillary membrane.
“In my clinic, we see patients who climb stairs and feel dizzy—not because of heart issues, but because their lungs can’t transfer oxygen fast enough due to thickened membranes.” — Dr. Rajiv Mehta, Pulmonologist, Cleveland Clinic
Mini Case Study: High-Altitude Adaptation
Consider a mountaineer ascending Mount Everest. At 8,848 meters, atmospheric pressure is less than one-third of sea level, meaning fewer oxygen molecules per breath. Yet climbers can survive—temporarily—because their bodies adapt to maximize every bit of available oxygen.
One adaptation is increased capillary density in the alveoli, enhancing surface contact. But critically, the thinness of the alveolar wall remains unchanged—and that’s vital. If the wall were thicker, even minor drops in oxygen pressure would make diffusion impossible. Evolution has preserved this thin barrier precisely because it enables survival under low-oxygen stress.
This real-world example underscores how the thin alveolar wall isn't just a biological curiosity—it's a lifeline under extreme conditions.
Checklist: Factors That Maintain Healthy Alveolar Walls
To preserve the integrity and thinness of alveolar walls, consider the following protective measures:
- ✅ Avoid smoking and secondhand smoke – major causes of alveolar destruction
- ✅ Minimize exposure to air pollutants and occupational dusts (e.g., silica, asbestos)
- ✅ Manage chronic conditions like COPD and asthma with proper medical care
- ✅ Practice deep breathing exercises to enhance alveolar ventilation
- ✅ Stay hydrated – mucus clearance helps prevent infection and inflammation
- ✅ Exercise regularly – improves lung elasticity and capillary perfusion
Frequently Asked Questions
Can alveolar walls regenerate if damaged?
Adult human alveoli have limited regenerative capacity. While some repair occurs after mild injury, significant damage—such as from emphysema or fibrosis—is usually permanent. Recent research into stem cell therapies offers hope, but clinical applications remain experimental.
Do all animals have similarly thin alveolar walls?
Not exactly. Mammals generally share this adaptation, but species with higher metabolic rates (like birds and small mammals) often have even more efficient gas exchange systems. Birds, for instance, use a cross-current flow system in air capillaries that surpasses mammalian efficiency, though their structural approach differs.
Why don’t thin alveolar walls rupture easily?
Despite their thinness, alveolar walls are reinforced by elastic and collagen fibers in the interstitial space. Additionally, pulmonary surfactant reduces surface tension, preventing collapse during exhalation. This balance of fragility and resilience is tightly regulated by biochemical and mechanical factors.
Conclusion: The Thin Line Between Life and Suffocation
The thinness of alveolar walls is not an accident of anatomy—it is a precise solution honed by millions of years of evolution to meet the relentless demand for oxygen. Every breath you take relies on a barrier thinner than a cell, yet strong enough to withstand constant mechanical stress. It is a testament to nature’s ability to optimize form for function.
Understanding this delicate structure empowers us to protect it. From avoiding toxins to managing respiratory health proactively, the choices we make today influence how efficiently our lungs perform tomorrow. The next time you inhale deeply, remember: life flows across a membrane so thin it defies imagination.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?