Swelling in both feet—medically known as bilateral edema—is a surprisingly common complaint, especially among adults over 50 or those with chronic health conditions. While occasional puffiness after standing for hours or during hot weather may be harmless, persistent or sudden swelling can signal underlying issues that require attention. Understanding the root causes, recognizing warning signs, and knowing when to act can make a significant difference in long-term health outcomes.
Understanding Bilateral Foot Swelling
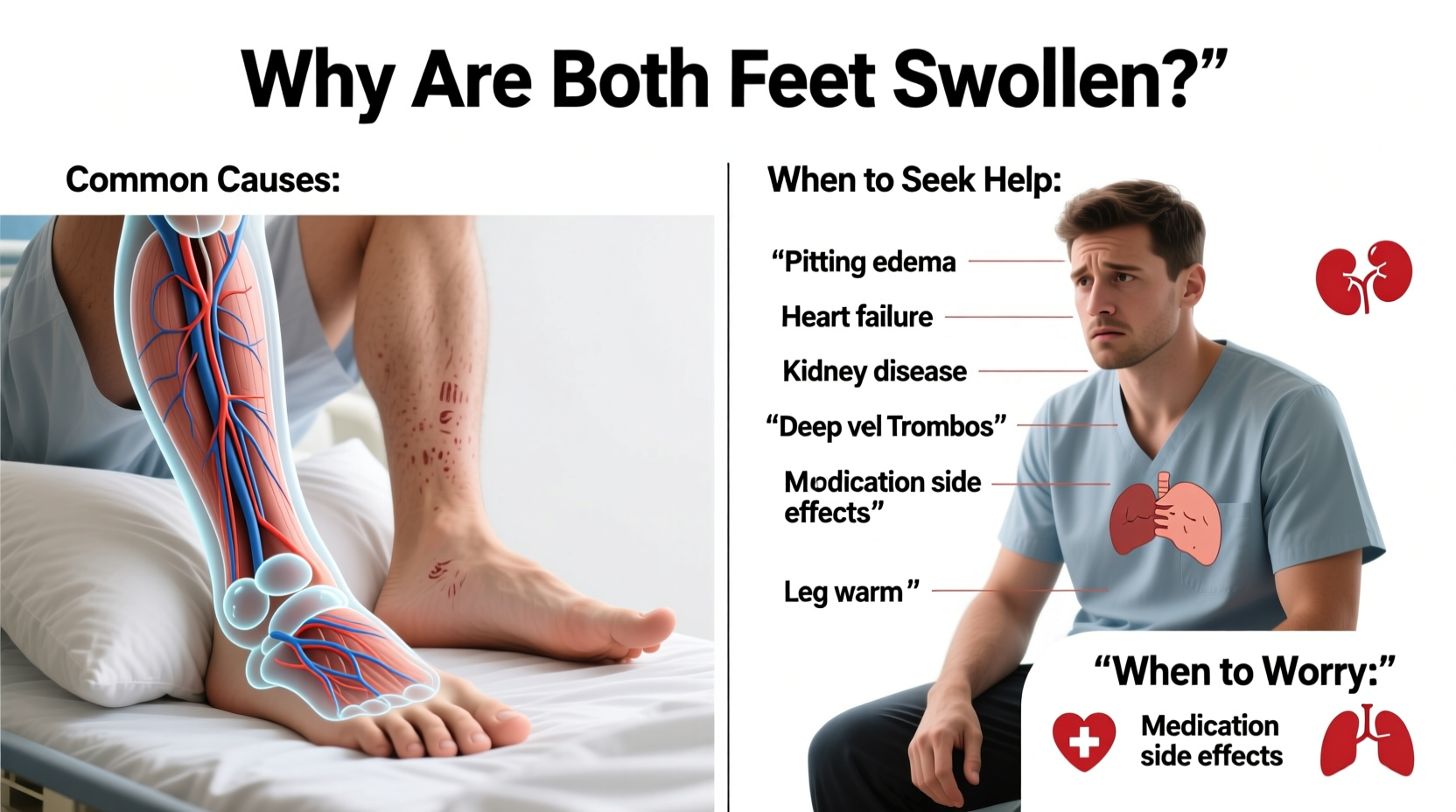
Bilateral foot swelling occurs when excess fluid accumulates in the tissues of both feet and lower legs. This condition, called peripheral edema, typically affects both sides of the body symmetrically, distinguishing it from unilateral swelling, which may point to localized problems like injury or infection.
The body maintains fluid balance through complex interactions between the circulatory system, kidneys, and lymphatic system. When this equilibrium is disrupted—due to heart strain, kidney dysfunction, or prolonged immobility—fluid can pool in the lower extremities due to gravity.
“Bilateral edema isn’t always dangerous, but it should never be ignored if it’s new, worsening, or accompanied by other symptoms like shortness of breath.” — Dr. Alan Reyes, Internal Medicine Specialist
Common Causes of Swollen Feet in Both Legs
Many factors contribute to bilateral foot swelling. Some are lifestyle-related and easily reversible; others stem from systemic diseases requiring medical management.
- Heart failure: When the heart can't pump efficiently, blood backs up in the veins, forcing fluid into surrounding tissues. Swelling often starts in the feet and progresses upward.
- Kidney disease: Impaired kidney function leads to sodium and water retention. This causes generalized swelling, particularly in the legs, feet, and around the eyes.
- Liver cirrhosis: Advanced liver disease reduces protein production (especially albumin), lowering blood osmotic pressure and allowing fluid to leak into tissues.
- Prolonged sitting or standing: Long flights, desk jobs, or extended periods on your feet can impair circulation and lead to temporary swelling.
- Medication side effects: Common culprits include calcium channel blockers (for high blood pressure), NSAIDs, steroids, and some diabetes medications like thiazolidinediones.
- Pregnancy: Hormonal changes and increased blood volume can cause mild to moderate swelling, especially in the third trimester. However, sudden or severe swelling may indicate preeclampsia.
- Venous insufficiency: Damaged or weak valves in leg veins allow blood to pool, leading to chronic swelling, heaviness, and sometimes skin changes.
When to Worry: Red Flags That Demand Medical Attention
Not all foot swelling requires emergency care, but certain symptoms suggest a serious underlying condition. Immediate evaluation is warranted if you experience:
- Sudden onset of severe swelling without clear cause
- Shortness of breath, chest pain, or palpitations (possible heart or lung issue)
- Swelling accompanied by fatigue, foamy urine, or high blood pressure (kidney concern)
- Abdominal swelling or jaundice (signs of liver disease)
- Swelling that leaves a dent when pressed (pitting edema) and worsens daily
- Unexplained weight gain over days or weeks
These signs may indicate decompensated heart failure, nephrotic syndrome, or deep vein thrombosis (DVT)—a potentially life-threatening clot. While DVT typically affects one leg, bilateral involvement can occur in rare cases, especially with pelvic vein obstruction or severe immobility.
Diagnostic Process: What to Expect at the Doctor’s Office
If your swelling persists beyond a few days or is associated with other symptoms, a healthcare provider will likely conduct a thorough assessment. This includes:
- Medical history review: Questions about medications, recent travel, chronic illnesses, and symptom progression.
- Physical examination: Checking for pitting edema, jugular venous pressure, lung sounds, and abdominal distension.
- Lab tests: Blood work to assess kidney and liver function, electrolyte levels, and cardiac markers.
- Imaging: Echocardiogram to evaluate heart function, ultrasound to rule out clots, or abdominal imaging for liver/kidney structure.
Accurate diagnosis is essential because treatment varies widely depending on the cause. For example, diuretics help in heart failure but can worsen kidney-related edema if not carefully managed.
Action Plan: Managing and Preventing Swollen Feet
Depending on the cause, managing bilateral foot swelling involves a combination of medical treatment and lifestyle adjustments. Here’s a practical checklist to follow:
✅ Swelling Management Checklist
- Monitor daily weight—sudden increases may signal fluid retention.
- Limit salt intake to less than 2,300 mg per day (ideally 1,500 mg if advised).
- Avoid tight clothing or shoes that restrict circulation.
- Stay active—walking improves venous return and reduces pooling.
- Wear compression stockings if recommended by your doctor.
- Stay hydrated—paradoxically, adequate water helps regulate fluid balance.
- Review medications with your physician to identify possible contributors.
Comparison Table: Common Causes vs. Key Features
| Cause | Swelling Pattern | Associated Symptoms | Diagnostic Clues |
|---|---|---|---|
| Heart Failure | Both legs, progressive, worse at end of day | Fatigue, shortness of breath, orthopnea | Elevated BNP, abnormal echocardiogram |
| Kidney Disease | Generalized (face, hands, legs) | Foamy urine, high blood pressure, fatigue | Proteinuria, elevated creatinine |
| Liver Cirrhosis | Legs + abdomen (ascites) | Jaundice, easy bruising, spider angiomas | Low albumin, abnormal LFTs |
| Medication Side Effect | Mild to moderate, bilateral | No other systemic symptoms | Temporal link to drug initiation |
| Chronic Venous Insufficiency | Lower legs, often with skin discoloration | Heaviness, varicose veins, ulcers | Visible vein changes, positive venous Doppler |
Real-Life Example: Recognizing a Silent Warning
Martha, a 68-year-old woman with hypertension, noticed her shoes felt tighter over two weeks. She dismissed it as aging until she struggled to climb stairs without gasping for air. Her primary care doctor checked her weight—up 5 pounds in a week—and heard crackles in her lungs. Blood tests revealed elevated BNP, and an echocardiogram showed reduced ejection fraction. She was diagnosed with congestive heart failure. With medication adjustments and dietary changes, her swelling improved within days. Martha’s case illustrates how seemingly minor swelling can mask a serious cardiac condition.
Frequently Asked Questions
Is it normal for feet to swell during pregnancy?
Yes, mild swelling in the feet and ankles is common during the third trimester due to increased blood volume and pressure from the growing uterus. However, sudden or severe swelling, especially with headaches or vision changes, could indicate preeclampsia and requires immediate evaluation.
Can drinking more water help reduce swelling?
Yes. Staying well-hydrated helps the kidneys flush excess sodium and fluid. Dehydration can actually worsen fluid retention because the body holds onto water when it senses low intake.
Should I take diuretics for swollen feet?
Only under medical supervision. While “water pills” can relieve symptoms, they don’t treat the underlying cause and may lead to electrolyte imbalances or kidney stress if used improperly.
Conclusion: Listen to Your Body
Bilateral foot swelling is more than a comfort issue—it’s a potential window into your cardiovascular, renal, or hepatic health. While lifestyle-related puffiness often resolves with rest and elevation, persistent or symptomatic swelling demands investigation. Early detection of conditions like heart failure or kidney disease can significantly improve prognosis and quality of life.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?