If you've noticed that your allergies have intensified recently—whether it's constant sneezing, itchy eyes, or difficulty breathing—you're not alone. Many people report a sudden worsening of allergy symptoms even if they’ve had mild or no issues in the past. Allergies don’t always follow a predictable pattern. What once felt manageable can escalate quickly due to a range of biological, environmental, and lifestyle factors. Understanding why this shift occurs is the first step toward regaining control.
Allergic reactions happen when your immune system overreacts to otherwise harmless substances like pollen, dust mites, pet dander, or mold. While genetics play a role, external triggers and internal changes can dramatically influence symptom severity. The key lies in identifying what’s changed—both around you and within your body.
Environmental Triggers Behind Worsening Allergies
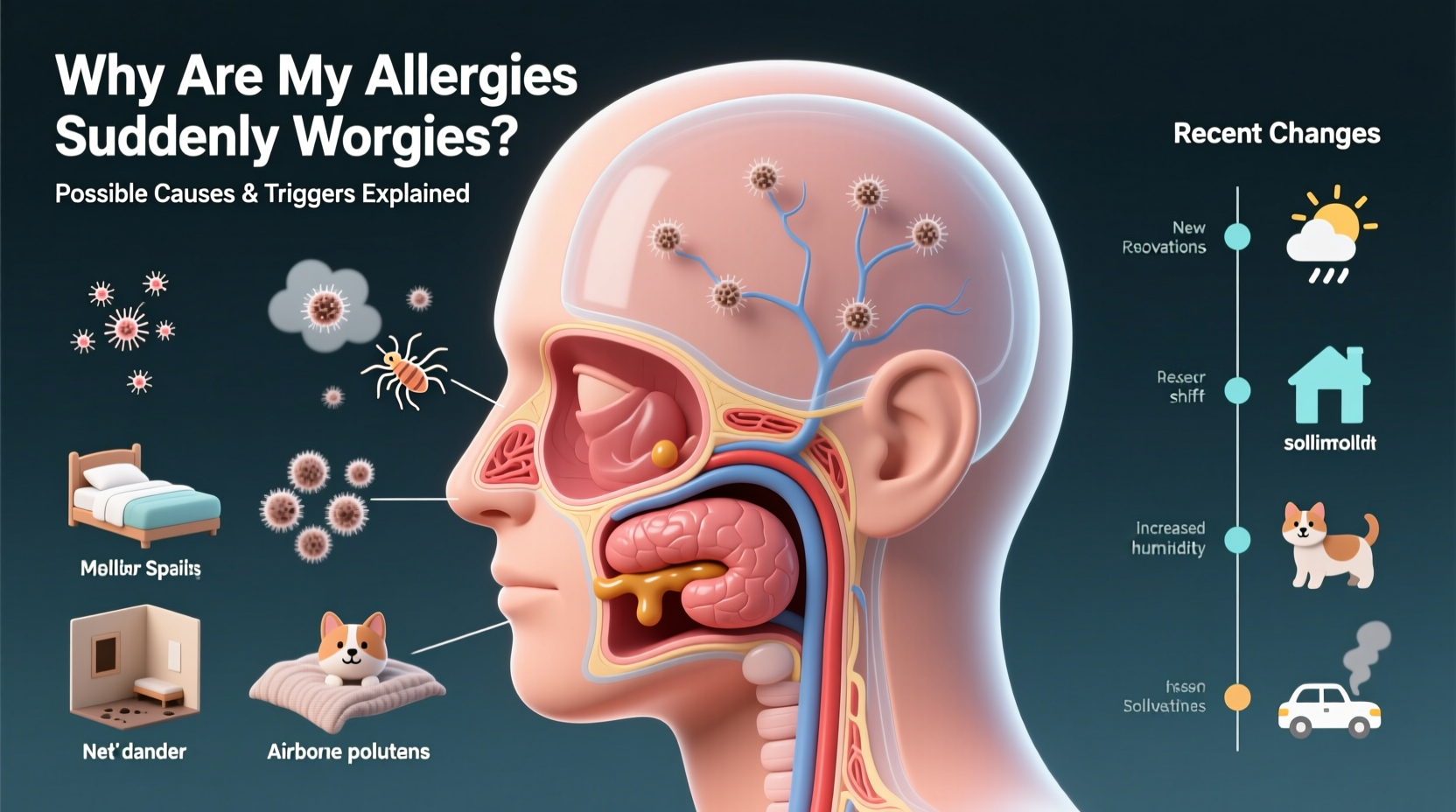
The world around us is constantly changing, and so are the allergens we’re exposed to. Climate change, urban development, and seasonal shifts all contribute to higher concentrations of airborne irritants.
- Pollen levels are rising: Warmer temperatures and increased CO₂ emissions promote longer growing seasons and more potent pollen production. Trees, grasses, and weeds now release pollen earlier in spring and later into fall.
- Mold proliferation: Damp weather, flooding, or poor indoor ventilation can lead to mold growth in homes, which releases spores that trigger allergic reactions.
- Urban air pollution: Diesel exhaust and ozone interact with pollen, making it more irritating and easier for your body to detect as a threat.
- New home or location: Moving to a different city or even redecorating can introduce new allergens such as carpet fibers, older insulation, or region-specific plants.
Internal Body Changes That Amplify Reactions
Sometimes, the culprit isn’t outside—it’s within your own physiology. Your immune system can become more sensitive due to age, stress, or health conditions.
For example, chronic stress elevates cortisol and inflammatory markers, priming your immune system for exaggerated responses. Similarly, hormonal fluctuations—such as those during pregnancy, menopause, or thyroid imbalances—can alter how your body reacts to allergens.
Another overlooked factor is gut health. Emerging research shows a strong link between the microbiome and immune regulation. Antibiotic use, poor diet, or digestive disorders may reduce beneficial bacteria, weakening immune tolerance and increasing allergy susceptibility.
“Adult-onset allergies are more common than people realize. The immune system remains dynamic throughout life, and sensitization can develop at any age.” — Dr. Lena Patel, Board-Certified Allergist & Immunologist
Common New Exposure Sources You Might Overlook
You may not realize you’ve introduced a new allergen into your daily environment. These subtle changes often fly under the radar but can have significant effects:
| Change | Potential Allergen Introduced | Symptom Impact |
|---|---|---|
| Adopted a pet | Pet dander, saliva, urine | Nasal congestion, asthma flare-ups |
| Bought new furniture | Dust mites, off-gassing chemicals (VOCs) | Eye irritation, coughing |
| Started using scented products | Fragrance compounds, phthalates | Headaches, respiratory tightness |
| Rented a basement apartment | Mold, dampness, rodent droppings | Wheezing, skin rashes |
| Switched laundry detergent | Synthetic fragrances, dyes | Contact dermatitis, sneezing |
Even small additions—like a new houseplant or storing old books in your bedroom—can increase allergen load over time. Cumulative exposure matters more than single events.
Step-by-Step Guide to Identifying the Cause
Pinpointing why your allergies have worsened requires systematic evaluation. Follow these steps to isolate potential triggers:
- Track your symptoms daily: Note timing, severity, location, and possible exposures. Use a journal or app to identify patterns.
- Assess recent lifestyle changes: Have you moved, adopted a pet, started a new job, or remodeled your home?
- Inspect your living space: Check for mold in bathrooms, basements, or under sinks. Vacuum upholstery and test for dust mites.
- Review medication history: Some drugs (like beta-blockers or NSAIDs) can worsen allergic responses or mask symptoms.
- Consult an allergist: Skin prick tests or blood tests (IgE testing) can confirm specific sensitivities.
- Try an elimination approach: Remove one suspected trigger at a time (e.g., switch detergents, keep pets out of bedrooms) and monitor changes over 2–3 weeks.
Mini Case Study: Sarah’s Sudden Spring Symptoms
Sarah, a 34-year-old teacher from Portland, Oregon, had only mild seasonal allergies in her youth. But last year, she began experiencing severe nasal congestion, fatigue, and wheezing every April—symptoms that lasted for months. Confused by the sudden intensity, she visited an allergist.
After reviewing her history, the doctor learned Sarah had moved into a ground-floor apartment near a park filled with cedar trees. She also started jogging outdoors each morning—right when pollen counts were highest. Skin testing confirmed a new sensitivity to cedar pollen, likely exacerbated by increased regional pollen loads due to climate shifts.
With a combination of daily antihistamines, nasal corticosteroids, and shifting her exercise routine to evenings, Sarah reduced her symptoms by 80% within four weeks. Her case illustrates how environment, behavior, and biology intersect to intensify allergies.
Checklist: Immediate Actions to Reduce Allergy Severity
- ✅ Replace HVAC filters with HEPA-rated ones
- ✅ Wash bedding weekly in hot water (130°F or higher)
- ✅ Use allergen-proof covers on pillows and mattresses
- ✅ Keep windows closed during high pollen seasons
- ✅ Shower and change clothes after being outdoors
- ✅ Clean floors with a vacuum equipped with a HEPA filter
- ✅ Avoid hanging laundry outside where pollen can cling
- ✅ Install a dehumidifier if basement or bathroom moisture exceeds 50%
FAQ
Can allergies get worse with age?
Yes. While some children outgrow allergies, adults can develop new sensitivities or experience heightened reactions due to immune system changes, hormonal shifts, or prolonged exposure to allergens.
Is there a connection between COVID-19 and worse allergies?
Some individuals report worsened allergies post-COVID. Researchers believe lingering inflammation or altered immune function (“long COVID”) may lower the threshold for allergic reactions, though more studies are ongoing.
Should I start taking allergy meds before symptoms appear?
Yes. For seasonal allergies, starting antihistamines or nasal sprays 1–2 weeks before your usual symptom onset can prevent inflammation from escalating and improve long-term control.
Conclusion: Take Control Before Symptoms Escalate
Sudden allergy flare-ups are rarely random. They’re signals from your body indicating a shift in your environment, immune function, or exposure habits. By systematically evaluating your surroundings, tracking symptoms, and seeking professional testing when needed, you can uncover the root cause and take meaningful action.
Don’t dismiss worsening allergies as just “part of getting older” or “this season being worse.” With the right strategies—from improving indoor air quality to adjusting daily routines—you can significantly reduce discomfort and protect your long-term respiratory health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?