Itching in the lower legs, particularly the calves, is a surprisingly common complaint. While often dismissed as a minor irritation, persistent or intense calf itchiness can interfere with sleep, concentration, and daily life. The causes range from simple dry skin to underlying medical conditions. Understanding what’s behind the itch—and how to respond appropriately—can make the difference between temporary discomfort and long-term relief.
Common Causes of Itchy Calves
The skin on the lower legs is thinner and has fewer oil glands than other areas of the body, making it more prone to dryness and irritation. Several factors contribute to itching specifically in the calf region.
- Dry Skin (Xerosis): Especially prevalent in winter or low-humidity environments, dry skin on the calves can crack and become intensely itchy.
- Atopic Dermatitis (Eczema): A chronic condition that often affects the creases of elbows and knees but can spread to the calves, causing red, inflamed, and itchy patches.
- Contact Dermatitis: Exposure to irritants like laundry detergents, synthetic fabrics, or certain lotions can trigger localized allergic reactions.
- Insect Bites or Infestations: Bedbugs, fleas, or mites may target exposed lower limbs at night, leading to clustered itchy bumps.
- Varicose Eczema (Stasis Dermatitis): Common in older adults or those with poor circulation, this condition results from blood pooling in the lower legs, leading to swelling, discoloration, and itchiness.
- Fungal Infections: Athlete’s foot can extend beyond the feet to the lower calves, especially if moisture is trapped under socks or tight clothing.
When Internal Health Issues Are to Blame
Sometimes, itchy calves signal deeper health concerns. These systemic conditions don’t originate in the skin but manifest through dermatological symptoms.
Liver disease, such as cholestasis, impairs bile flow and leads to a buildup of bile salts in the bloodstream, which can deposit in the skin and cause widespread itching—often worse at night and concentrated on the limbs.
Kidney failure, particularly in advanced stages, results in uremic pruritus due to toxin accumulation. Patients often report persistent itching on the legs and back.
Diabetes contributes to itchy skin through multiple pathways: poor circulation, nerve damage (neuropathy), and increased susceptibility to infections. Diabetic dermopathy can appear as light brown, scaly patches on the shins and calves.
Less commonly, thyroid disorders (both hypo- and hyperthyroidism) disrupt skin metabolism and moisture balance, leading to dry, flaky, and itchy skin.
“Persistent leg itching without a rash should prompt evaluation for metabolic or vascular issues.” — Dr. Lena Torres, Board-Certified Dermatologist
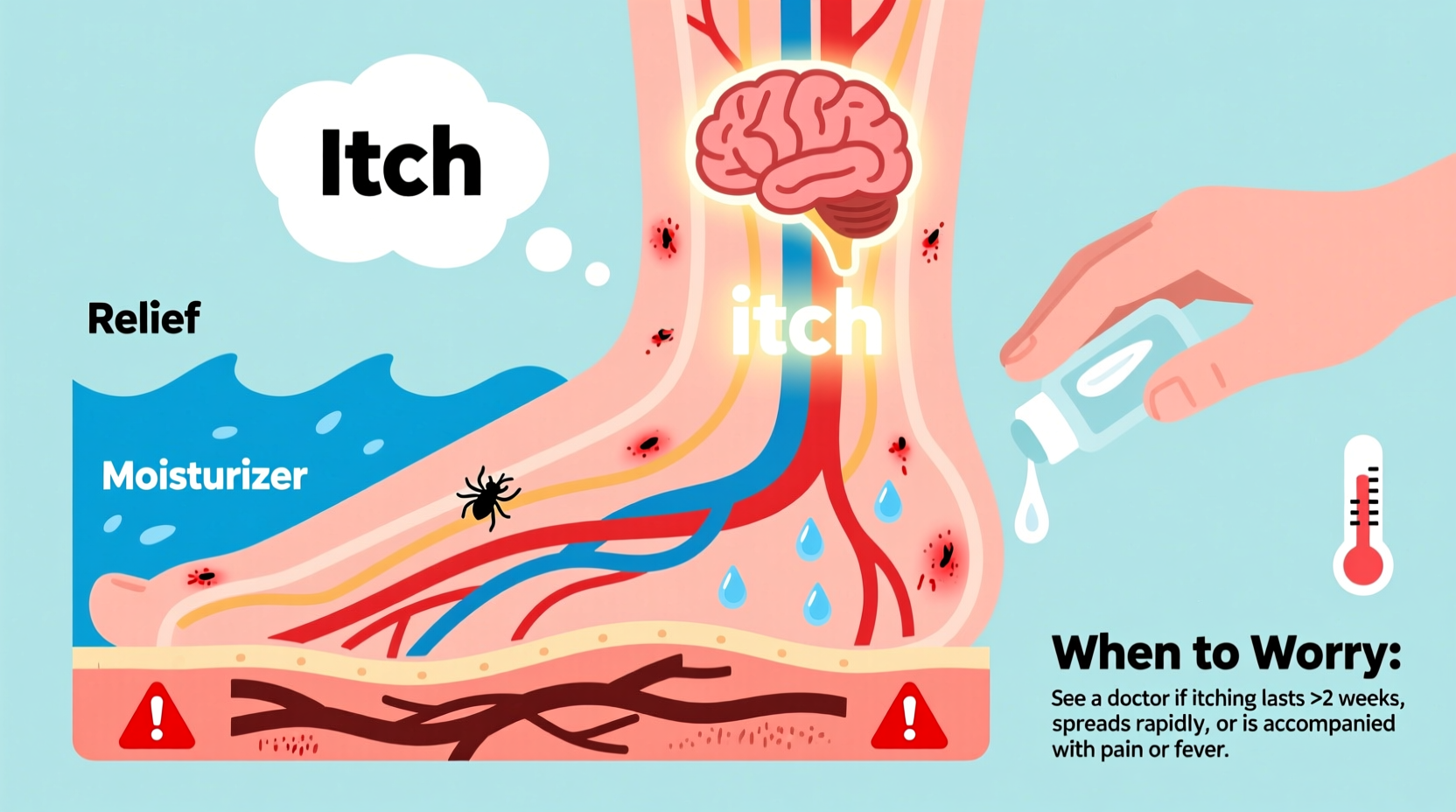
Immediate Relief Strategies
While identifying the root cause is essential, managing symptoms quickly improves quality of life. The following steps can reduce itching within hours.
- Moor moisturizer into damp skin immediately after bathing to lock in hydration. Look for ceramides, glycerin, or shea butter.
- Use fragrance-free products to avoid further irritation. Scented lotions often contain allergens.
- Cool compresses applied for 10–15 minutes soothe inflammation and numb nerve endings.
- Wear loose, breathable clothing made from cotton or bamboo to minimize friction.
- Try over-the-counter antihistamines like cetirizine or loratadine, especially if itching worsens at night.
- Apply topical hydrocortisone cream (1%) sparingly for up to one week to reduce localized inflammation.
| Remedy | Best For | Caution |
|---|---|---|
| Emollient creams | Dry skin, eczema | Avoid if infected skin present |
| Antihistamines | Allergic reactions, nighttime itch | May cause drowsiness |
| Hydrocortisone cream | Inflammatory rashes | Do not use long-term; consult doctor |
| Colloidal oatmeal baths | Irritated, sensitive skin | Ensure no fungal infection |
When to Worry: Red Flags That Demand Medical Attention
Most cases of itchy calves resolve with home care. However, certain signs indicate a need for professional evaluation.
- Itching that lasts longer than two weeks despite treatment
- Visible swelling, redness, warmth, or pain—possible sign of infection or deep vein thrombosis
- Open sores, oozing, or crusting
- Darkening or thickening of the skin (lichenification)
- Itch without a visible rash, especially at night
- History of diabetes, kidney disease, or liver conditions
If you notice varicose veins accompanied by swollen, discolored, and itchy skin, you may be developing venous stasis dermatitis. Left untreated, this can progress to ulcers. Similarly, generalized itching with no clear source could point to internal disease and warrants blood tests for liver and kidney function.
Real Example: Recognizing Stasis Dermatitis Early
Mark, a 62-year-old office worker, noticed his calves had been itchy for months. He assumed it was dry skin and used lotion regularly. Over time, the skin turned reddish-brown, felt leathery, and began to weep slightly near the ankles. After visiting a dermatologist, he was diagnosed with stasis dermatitis linked to chronic venous insufficiency. With compression stockings, topical treatments, and lifestyle changes, his symptoms improved significantly within six weeks. His case underscores the danger of dismissing persistent leg itch as mere dryness.
Prevention and Long-Term Care Checklist
Preventing recurrence involves consistent habits and awareness of personal risk factors.
- ✅ Moisturize calves daily, especially after showering
- ✅ Wear compression socks if you stand or sit for long periods
- ✅ Elevate legs when resting to improve circulation
- ✅ Avoid scratching—keep nails short and consider wearing cotton gloves at night
- ✅ Choose mild, pH-balanced cleansers for bathing
- ✅ Stay hydrated and maintain a balanced diet rich in omega-3 fatty acids
- ✅ Monitor for changes in skin color, texture, or sensation—especially if diabetic
Frequently Asked Questions
Can stress make my calves itch?
Yes. Stress activates the nervous system and can exacerbate existing skin conditions like eczema or psoriasis. It may also lead to neurogenic pruritus, where the brain perceives itch signals even without a rash.
Is it safe to scratch itchy calves?
Scratching provides temporary relief but damages the skin barrier, increasing the risk of infection and worsening inflammation. Repeated scratching can lead to lichen simplex chronicus—a thickened, leathery patch of skin that itches more as it heals.
Why are my calves itchier at night?
Nighttime itching is common due to lower distraction levels, increased body temperature, and natural circadian fluctuations in cortisol (an anti-inflammatory hormone). Conditions like liver disease or neuropathy often peak at night.
Take Control of Your Skin Health
Itchy calves are more than just a nuisance—they’re a signal from your body. Whether the cause is environmental, dermatological, or systemic, addressing it early prevents complications. Simple changes in skincare and habits can bring fast relief, but knowing when to see a doctor is equally important. Don’t normalize persistent itching. Listen to your body, take proactive steps, and seek expert guidance when needed.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?