Suddenly noticing that your ears feel warm or even burning can be unsettling. While it's often harmless, a sensation of heat in the ears can stem from various physical, emotional, or environmental factors. Unlike pain or swelling, which are more clearly indicative of an issue, hot ears are subtle—yet they may signal underlying conditions ranging from emotional stress to infections. Understanding why this happens is key to determining whether it’s a fleeting reaction or something requiring medical attention.
Common Causes of Hot Ears
Hot ears are rarely dangerous on their own, but they can be symptoms of broader physiological processes. The warmth typically results from increased blood flow to the area. Blood vessels in the ears dilate (expand) in response to certain triggers, causing a flushed, heated sensation. Below are the most frequent explanations:
- Emotional Flushing: Feelings of embarrassment, anxiety, or anger trigger the sympathetic nervous system, increasing circulation to the face and ears.
- Fever: When body temperature rises due to infection, blood flow increases to the skin’s surface—including the ears—to release heat.
- Allergic Reactions: Allergens such as pollen, food, or skincare products can cause localized inflammation and flushing.
- Alcohol Consumption: Alcohol dilates blood vessels, particularly in facial areas, leading to redness and warmth in the ears.
- Skin Conditions: Rosacea, eczema, or contact dermatitis can affect the ears, causing redness, heat, and sometimes itching.
- Hormonal Changes: Menopause or hormonal fluctuations may lead to hot flashes that include the ears.
- Environmental Heat: Prolonged exposure to sun, saunas, or high temperatures can overheat the skin on thin ear tissue.
When Hot Ears Signal a Medical Concern
While most cases resolve on their own, persistent or recurring ear heat—especially when paired with other symptoms—should not be ignored. Certain conditions require prompt evaluation by a healthcare provider.
Otitis Externa (Swimmer’s Ear)
An infection of the outer ear canal often caused by trapped moisture. Symptoms include ear warmth, pain, swelling, and sometimes discharge. Left untreated, it can progress to severe discomfort and hearing issues.
Autoimmune Disorders
Conditions like lupus or Sjögren’s syndrome can cause chronic inflammation, including in the ears. Systemic symptoms such as fatigue, joint pain, and dry eyes may accompany ear warmth.
Carotid Artery Issues
Rarely, unilateral (one-sided) ear heat could relate to vascular problems. Inflammation or abnormalities in the carotid artery may alter blood flow and produce localized warmth.
“Facial and auricular flushing should be evaluated if recurrent or asymmetrical. It could indicate an underlying inflammatory or vascular condition.” — Dr. Lena Torres, Otolaryngologist
Do’s and Don’ts: Managing Hot Ears at Home
| Action | Recommendation | Reason |
|---|---|---|
| Apply a cool compress | ✅ Do | Reduces surface temperature and soothes irritated skin |
| Use harsh soaps on ears | ❌ Don’t | Irritates sensitive skin and worsens inflammation |
| Monitor for additional symptoms | ✅ Do | Helps identify patterns linked to allergies, fever, or infection |
| Scratch or rub hot ears aggressively | ❌ Don’t | Can break skin and introduce bacteria |
| Stay hydrated | ✅ Do | Supports healthy circulation and reduces flushing severity |
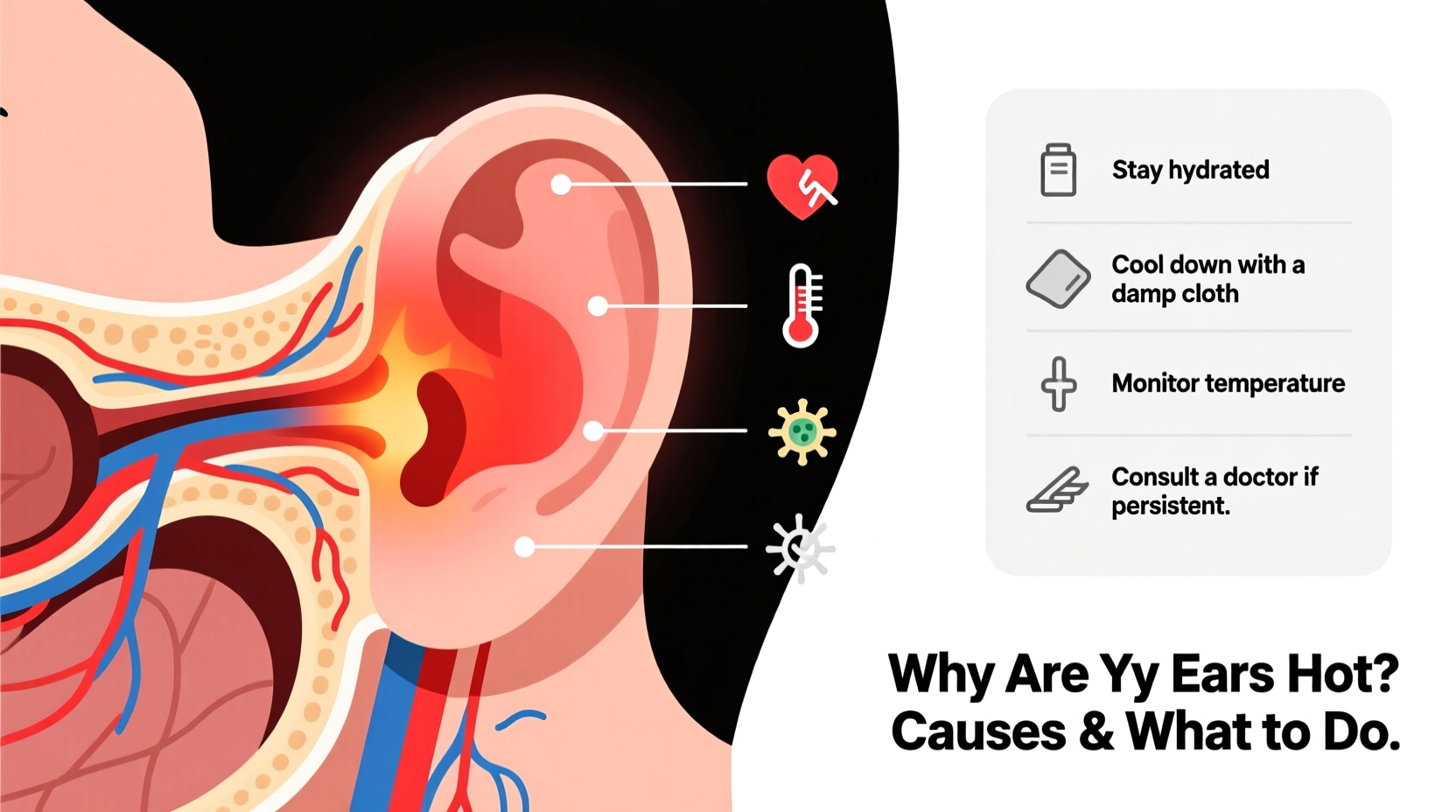
Step-by-Step Guide: What to Do When Your Ears Feel Hot
Follow this practical sequence to assess and manage the sensation effectively:
- Pause and Observe: Note when the heat started, how long it lasts, and whether it affects one or both ears.
- Check for Triggers: Reflect on recent activities—did you consume alcohol, experience stress, or apply new skincare products?
- Take Your Temperature: Use a thermometer to rule out fever, especially if you feel unwell.
- Cool the Area Gently: Dampen a clean cloth with cool water and hold it against the ears for 5–10 minutes.
- Hydrate and Rest: Drink water and sit in a well-ventilated space to help regulate body temperature.
- Monitor for Escalation: Watch for pain, swelling, rash, or hearing changes over the next 24 hours.
- Seek Medical Advice: If symptoms persist beyond a day or worsen, consult a doctor—especially if only one ear is affected.
Real-Life Example: Sarah’s Experience with Recurring Ear Heat
Sarah, a 34-year-old teacher, began noticing her ears turning red and feeling hot several times a week. At first, she dismissed it as stress-related, especially since it happened before presentations. But when the warmth started occurring at random times—even while relaxing at home—she grew concerned. After tracking her symptoms, she realized the episodes often followed meals containing spicy foods or red wine. She consulted an allergist, who identified a mild histamine intolerance. By adjusting her diet and taking natural antihistamines like quercetin, Sarah reduced the frequency of flare-ups significantly.
This case illustrates how keeping a symptom journal can uncover hidden triggers that aren't immediately obvious.
Prevention Checklist
To minimize episodes of hot ears, use this actionable checklist:
- ✔ Track when your ears feel hot and any potential triggers (food, emotions, environment)
- ✔ Limit alcohol and spicy foods if they correlate with flare-ups
- ✔ Practice stress-reduction techniques like meditation or box breathing
- ✔ Protect ears from extreme temperatures with hats or shade
- ✔ Avoid using fragranced lotions or earrings made of nickel, which may cause allergic reactions
- ✔ Maintain good ear hygiene without inserting objects into the ear canal
- ✔ Stay hydrated throughout the day to support stable circulation
Frequently Asked Questions
Can high blood pressure cause hot ears?
Not directly. While hypertension affects blood vessels, it doesn’t typically cause isolated ear warmth. However, anxiety related to high blood pressure might trigger flushing. Always monitor blood pressure if you have cardiovascular concerns.
Is it normal for only one ear to feel hot?
Occasionally, yes—due to localized irritation or minor nerve activity. But persistent one-sided heat warrants evaluation to rule out infection, nerve inflammation, or vascular irregularities.
Can menopause cause hot ears?
Absolutely. Hot flashes during perimenopause and menopause often begin in the chest and spread upward, affecting the face, neck, and ears. These episodes may last from seconds to minutes and occur multiple times a day.
Final Thoughts: Listen to Your Body
Your ears may be small, but they’re highly sensitive indicators of your internal state. Whether it’s a fleeting blush from embarrassment or a recurring warmth tied to deeper health patterns, the sensation deserves attention—not alarm, but awareness. Most causes are benign and manageable with simple lifestyle adjustments. However, consistency, symmetry, and accompanying symptoms matter. When in doubt, seeking professional insight ensures peace of mind and timely care.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?