Suddenly noticing that your ears are red, warm to the touch, or even tender can be alarming. While it’s often harmless and temporary, persistent or recurring ear redness and heat can signal underlying health issues ranging from skin conditions to emotional responses. Understanding the root cause is essential to determining whether home care is sufficient or if medical attention is needed. This article explores the most common reasons behind red, hot ears, backed by medical insights, practical remedies, and real-life scenarios to help you respond wisely.
Common Causes of Red and Hot Ears
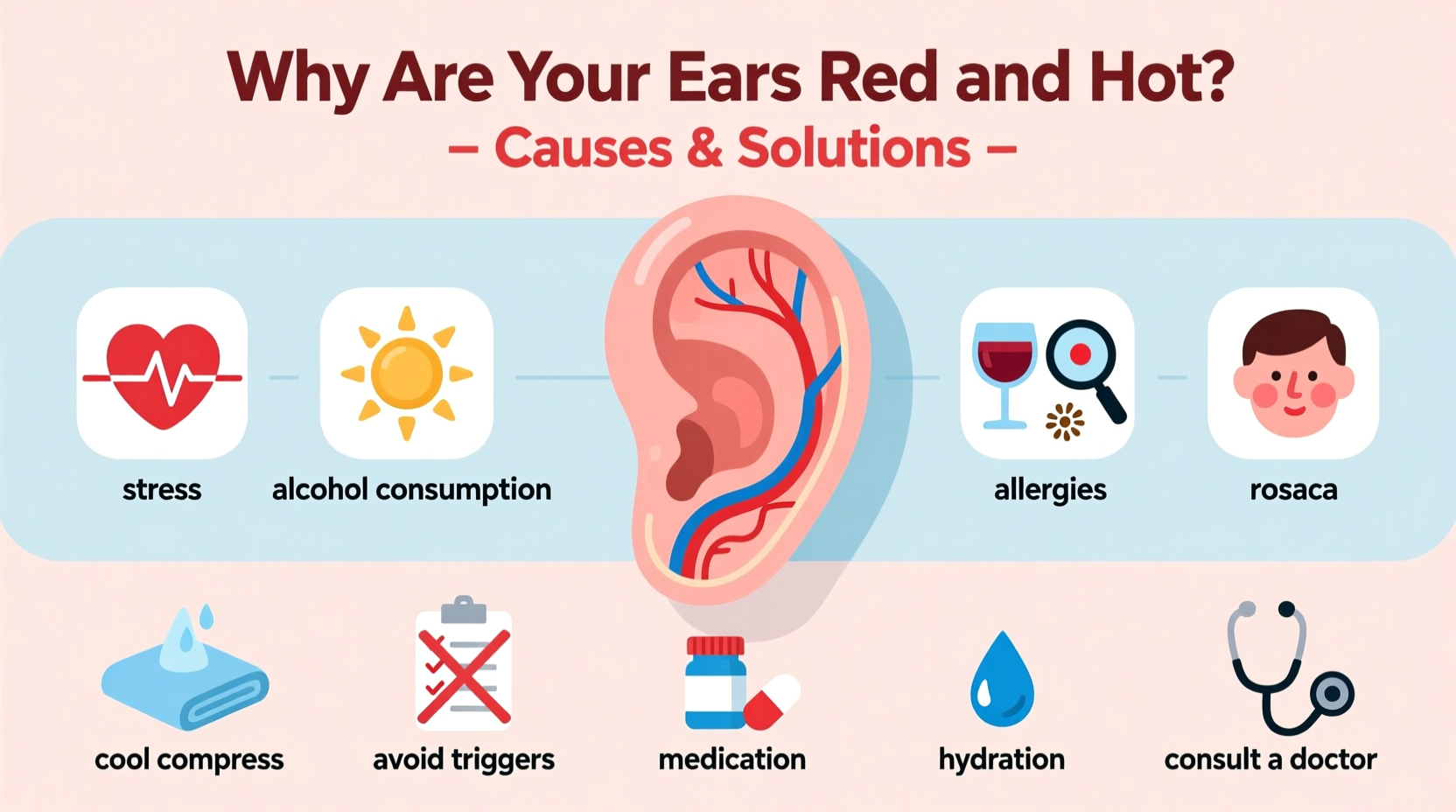
Redness and warmth in the ears typically result from increased blood flow to the area. Blood vessels dilate in response to various internal and external triggers, causing the skin to appear flushed and feel warm. The following are among the most frequent causes:
- Emotional flushing: Blushing due to embarrassment, anxiety, or anger activates the sympathetic nervous system, increasing circulation to facial areas including the ears.
- Temperature changes: Exposure to cold wind or extreme heat can trigger vasodilation or irritation, especially in sensitive skin.
- Alcohol consumption: Alcohol causes blood vessels to expand, particularly in individuals with alcohol flush reaction or Asian flush syndrome.
- Sunburn: Ultraviolet exposure without protection can burn the thin skin on the ears, leading to redness, pain, and peeling.
- Exercise-induced flushing: Physical activity raises body temperature and increases blood flow, commonly affecting the face and ears.
Skin Conditions That Affect the Ears
Beyond transient flushing, chronic skin disorders may target the ears specifically. These conditions often come with additional symptoms such as itching, scaling, or swelling.
Rosacea
A chronic inflammatory condition primarily affecting the face, rosacea can extend to the ears. It often causes persistent redness, visible blood vessels, and sometimes acne-like bumps. Triggers include spicy foods, stress, and temperature extremes.
Eczema (Atopic Dermatitis)
This condition leads to dry, itchy, inflamed skin. When eczema affects the outer ear or ear canal, it can cause redness, flaking, and discomfort. Scratching may worsen inflammation and lead to infection.
Seborrheic Dermatitis
Characterized by greasy, scaly patches, this form of dermatitis commonly appears on oily areas like the scalp, nose, and ears. It may cause redness around the ear folds or behind the ears.
“Facial flushing, especially when recurrent, should not be dismissed as just ‘blushing.’ In clinical practice, we often find undiagnosed rosacea or hormonal imbalances behind persistent ear redness.” — Dr. Lena Torres, Board-Certified Dermatologist
Medical and Systemic Causes
In some cases, red and hot ears point to deeper physiological processes. These require proper diagnosis and management.
High Blood Pressure (Hypertension)
While not a direct symptom, some people report facial and ear flushing during sudden blood pressure spikes. This is more common in individuals with uncontrolled hypertension or during episodes of stress.
Autoimmune Disorders
Conditions like lupus or relapsing polychondritis can cause inflammation of cartilage, including in the ears. Relapsing polychondritis, though rare, presents with painful, red ears, joint pain, and sometimes hearing changes.
Medication Side Effects
Some drugs—especially vasodilators like nifedipine, niacin supplements, or certain chemotherapy agents—can induce flushing. Niacin, in particular, is known for causing intense warmth and redness in the face and ears within minutes of ingestion.
Infections
Otitis externa (swimmer’s ear) or cellulitis of the ear can cause localized redness, heat, swelling, and pain. These infections require prompt treatment with antibiotics.
Step-by-Step Guide to Identifying and Addressing the Cause
Follow this timeline to assess and manage red, hot ears effectively:
- Observe the pattern: Note when the redness occurs—after eating, drinking, exercising, or during stress. Keep a symptom diary for one week.
- Check for other symptoms: Look for itching, pain, scaling, fever, or joint discomfort that could suggest an underlying condition.
- Eliminate obvious triggers: Avoid alcohol, spicy foods, extreme temperatures, and harsh skincare products temporarily.
- Apply cool compresses: Use a clean, damp cloth to soothe the area. Do not rub or scratch.
- Use gentle skincare: Apply fragrance-free moisturizers if skin is dry. Avoid exfoliants or alcohol-based cleansers near the ears.
- Consult a healthcare provider: If symptoms persist beyond a few days, worsen, or recur frequently, seek evaluation from a dermatologist or primary care physician.
Do’s and Don’ts: Managing Ear Redness
| Action | Do | Don't |
|---|---|---|
| Cleansing | Use mild, fragrance-free soap | Scrub aggressively or use alcohol wipes |
| Moisturizing | Apply hypoallergenic lotion | Use petroleum-based products without patch testing |
| Exposure | Wear hats in sun or cold weather | Stay in extreme temperatures unprotected |
| Treatment | Try OTC hydrocortisone for mild inflammation | Self-diagnose or use steroid creams long-term without guidance |
Real Example: When Stress Turned Ears Crimson
Mark, a 34-year-old teacher, began noticing his ears turning bright red during parent-teacher meetings. At first, he dismissed it as nerves, but the flushing became more frequent—even occurring at home. He also developed small bumps around his earlobes and jawline. After consulting a dermatologist, Mark was diagnosed with subtype 1 rosacea, triggered by stress and caffeine. With a regimen that included topical metronidazole, stress-reduction techniques, and avoiding coffee after noon, his symptoms improved significantly within six weeks.
This case highlights how emotional triggers can amplify underlying skin conditions—and why early intervention matters.
Prevention and Long-Term Care Tips
Whether your red ears stem from environment, emotion, or illness, proactive habits can reduce flare-ups:
- Wear sunscreen daily, including on the ears, especially if bald or with short hair.
- Limit alcohol and spicy foods if they consistently trigger flushing.
- Manage stress through mindfulness, breathing exercises, or therapy.
- Use lukewarm water when washing your face; hot water can worsen redness.
- Choose skincare products labeled “non-comedogenic” and “for sensitive skin.”
Frequently Asked Questions
Can high blood pressure cause red ears?
Not directly. While sudden spikes in blood pressure may coincide with facial flushing, red ears alone are not a reliable sign of hypertension. However, chronic flushing should prompt a check-up to rule out cardiovascular or endocrine issues.
Is it normal for ears to get hot during exercise?
Yes. Increased circulation and body heat during physical activity commonly cause temporary redness and warmth in the ears. This usually resolves within minutes of cooling down. If accompanied by dizziness or chest pain, consult a doctor.
When should I worry about red ears?
Seek medical advice if redness is painful, spreading, associated with fever, or lasts more than a few days without explanation. Sudden onset with swelling or hearing changes requires urgent evaluation.
Final Thoughts and Call to Action
Red and hot ears are more than just a cosmetic concern—they’re signals from your body. Whether it’s a fleeting blush or a recurring rash, understanding the cause empowers you to take control. Simple lifestyle adjustments often make a big difference, but don’t hesitate to seek professional insight when symptoms persist. Your skin’s health reflects your overall well-being.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?