Seeing prominent veins in the whites of your eyes can be unsettling, especially if it’s a recent change. While visible eye veins are often harmless and temporary, they can sometimes signal underlying health issues. The delicate blood vessels in the conjunctiva—the clear membrane covering the sclera—are easily influenced by environmental, physiological, and medical factors. Understanding what causes these veins to become more noticeable helps determine whether it's a minor irritation or something requiring medical attention.
Common Causes of Veiny Eyes
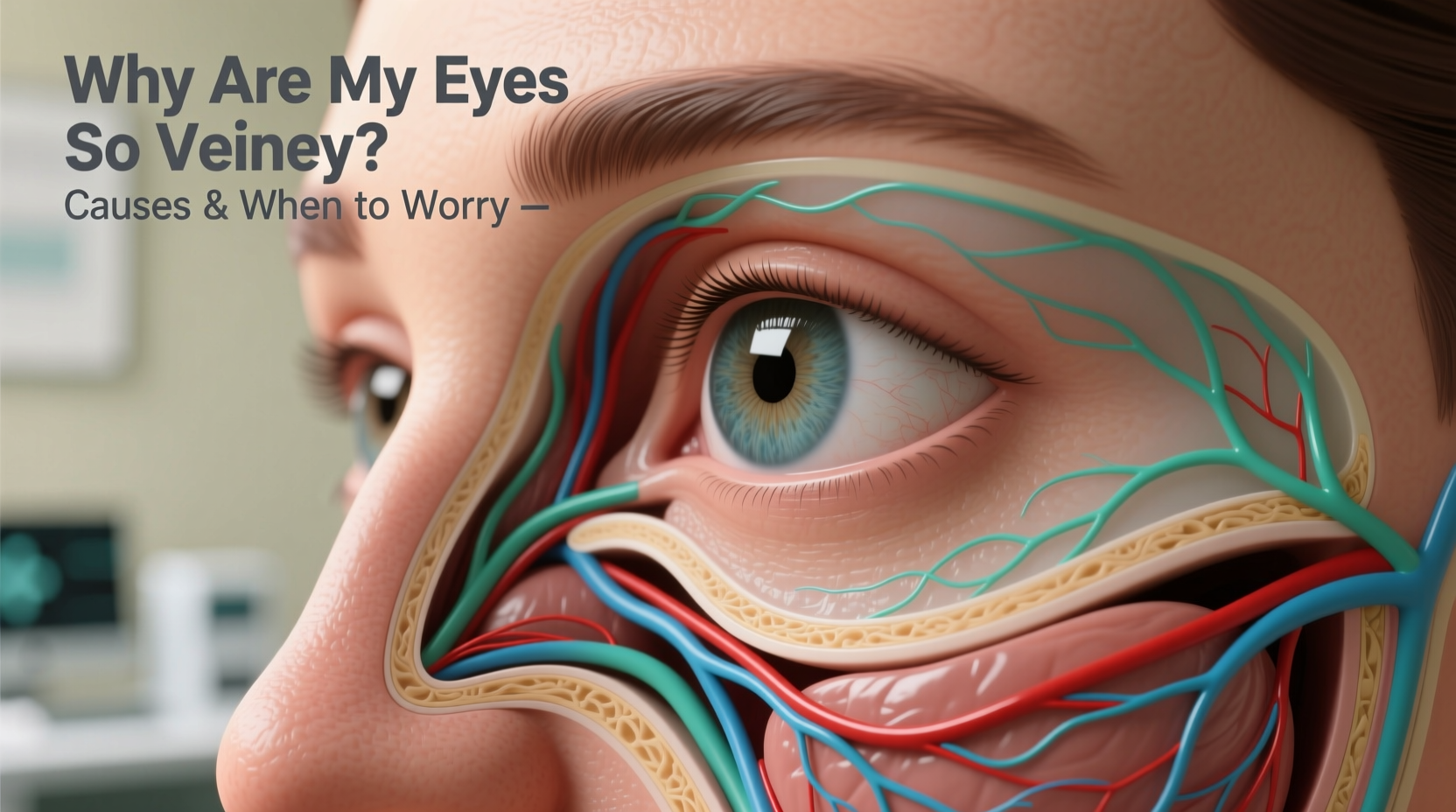
The appearance of veiny eyes is usually due to dilation, inflammation, or increased visibility of the superficial blood vessels in the conjunctiva. These changes are typically benign but can vary in cause and duration.
- Dryness: Prolonged screen use, low humidity, or insufficient tear production can dry out the eyes, prompting blood vessels to expand for increased oxygen delivery.
- Allergies: Seasonal or environmental allergens trigger histamine release, leading to redness and swollen vessels.
- Fatigue: Lack of sleep increases ocular surface stress, causing vasodilation and visible veins.
- Contact lens overuse: Extended wear reduces oxygen flow to the cornea, prompting compensatory vessel growth and dilation.
- Bright light exposure: UV rays and glare strain the eyes, leading to vascular response.
- Aging: Thinning of the conjunctival tissue with age makes underlying vessels more apparent.
When Veiny Eyes Signal a Health Concern
While most cases resolve on their own, persistent or worsening vein prominence may point to more serious conditions. Recognizing warning signs early improves outcomes.
Conjunctivitis (Pink Eye)
Inflammation from viral, bacterial, or allergic sources causes redness, discharge, and discomfort. Viral forms are highly contagious and often accompany colds.
Subconjunctival Hemorrhage
A burst blood vessel creates a bright red patch on the white of the eye. Though alarming in appearance, it’s usually painless and resolves within 1–2 weeks.
Uveitis
Inflammation inside the eye affects deeper structures and can cause redness around the iris, light sensitivity, blurred vision, and pain. Requires prompt treatment to prevent vision loss.
Glaucoma
Elevated intraocular pressure damages the optic nerve. While not always visibly red, some forms like acute angle-closure glaucoma present with sudden redness, pain, nausea, and vision disturbances.
Ocular Rosacea
A skin condition affecting the face can extend to the eyelids and eyes, causing chronic redness, burning, and dilated vessels.
“Persistent redness that doesn’t improve in a few days should be evaluated. It could be a sign of inflammation or elevated eye pressure.” — Dr. Lena Torres, Ophthalmologist, Massachusetts Eye Institute
Lifestyle and Environmental Triggers
Daily habits significantly influence eye health. Even without disease, external stressors can make veins more visible.
| Factor | Effect on Eyes | Prevention Strategy |
|---|---|---|
| Screen Time | Reduced blinking leads to dryness and strain | Follow the 20-20-20 rule; use artificial tears |
| Smoking | Chemicals impair circulation and irritate eyes | Quit smoking; avoid secondhand smoke |
| Dehydration | Reduces tear volume and increases vessel visibility | Drink adequate water daily (at least 8 glasses) |
| Pollution | Particulates cause irritation and inflammation | Wear wraparound sunglasses outdoors |
| Caffeine & Alcohol | Can dehydrate and alter blood flow | Moderate intake; balance with hydration |
Mini Case Study: Office Worker with Persistent Eye Redness
Mark, a 34-year-old software developer, noticed increasingly veiny eyes after transitioning to remote work. He spent 10+ hours daily on screens, often skipped breaks, and worked in a dry, air-conditioned room. Initially dismissing it as fatigue, he later developed burning sensations and light sensitivity. An optometrist diagnosed him with digital eye strain complicated by mild dry eye syndrome. After implementing ergonomic adjustments, using lubricating drops, and reducing screen time, his symptoms improved within three weeks. This case highlights how modern work environments contribute to ocular stress—even without infection.
When to Seek Medical Attention
Not all veiny eyes require urgent care, but certain symptoms warrant professional evaluation. Ignoring them can lead to complications like corneal damage or permanent vision changes.
- Pain or throbbing in the eye
- Sudden vision changes (blurriness, halos, blind spots)
- Sensitivity to light
- Discharge or crusting
- Swelling of eyelids or surrounding tissue
- Symptoms lasting more than 7–10 days without improvement
- History of glaucoma or autoimmune disorders
Step-by-Step Guide to Managing Mild Veiny Eyes at Home
- Stop wearing contact lenses temporarily to allow the eyes to breathe and recover.
- Apply a cold compress for 5–10 minutes twice daily to constrict blood vessels and reduce inflammation.
- Use preservative-free artificial tears 3–4 times a day to combat dryness.
- Limit screen exposure and follow the 20-20-20 rule: every 20 minutes, look at something 20 feet away for 20 seconds.
- Avoid rubbing your eyes, which can worsen irritation and rupture small vessels.
- Stay hydrated and reduce alcohol and caffeine intake for 48–72 hours.
- Evaluate your environment: add a humidifier, reduce dust, and wear blue-light glasses if needed.
Frequently Asked Questions
Are veiny eyes dangerous?
Most of the time, no. Temporary vein prominence due to fatigue, dryness, or minor irritation is not dangerous. However, if accompanied by pain, vision changes, or persistent redness, it may indicate an underlying condition that needs diagnosis and treatment.
Can high blood pressure cause veiny eyes?
Indirectly, yes. Chronic hypertension can damage blood vessels throughout the body, including those in the eyes. While it doesn’t typically cause immediate redness, long-term uncontrolled high blood pressure increases the risk of hypertensive retinopathy, which affects retinal vessels and can be detected during an eye exam.
Do eye whitening drops help?
Over-the-counter redness relievers (like tetrahydrozoline) constrict blood vessels temporarily, making eyes appear whiter. However, frequent use can lead to rebound redness—where the eyes become more irritated once the effect wears off. They should be used sparingly and not for more than 2–3 days consecutively.
Conclusion: Know Your Normal, Act When Needed
Veiny eyes are a common occurrence, often tied to lifestyle and environment rather than disease. Most cases respond well to rest, hydration, and simple adjustments. But because the eyes are windows to overall health, persistent changes deserve attention. Regular eye exams not only monitor vision but also detect systemic conditions like diabetes or hypertension before other symptoms arise.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?