It’s not uncommon to notice prominent veins on the tops of your feet—especially after standing for long periods or during exercise. For many people, this is a normal anatomical variation. However, sudden changes, discomfort, or accompanying symptoms may signal an underlying condition that warrants attention. Understanding why your feet appear veiny helps distinguish between harmless visibility and potential vascular concerns.
Anatomy of Foot Veins: Why They’re Visible
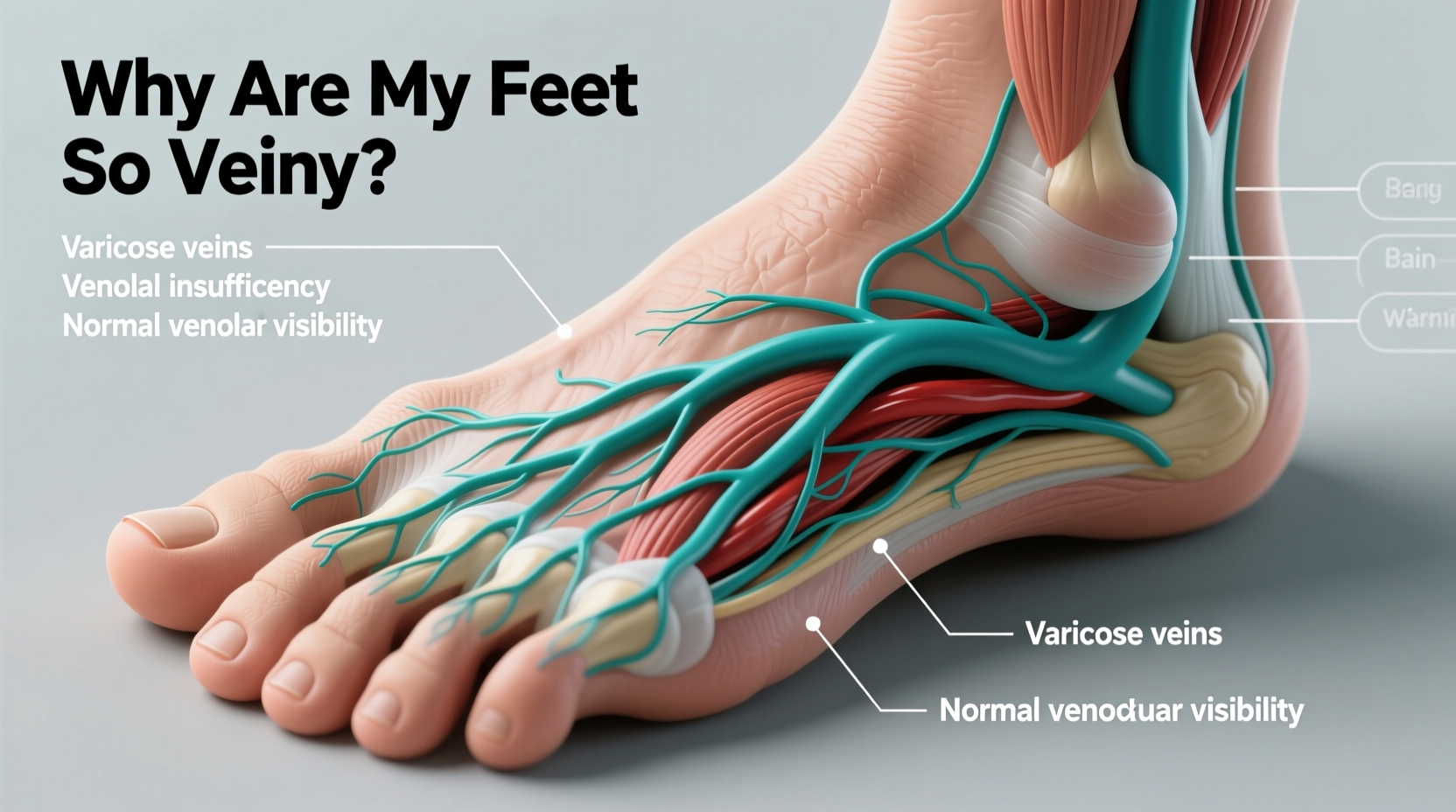
The human foot contains a network of superficial and deep veins responsible for returning deoxygenated blood back to the heart. The superficial veins lie just beneath the skin, making them more visible than deeper vessels. Several natural factors contribute to their prominence:
- Skin thickness: Thinner skin on the top of the foot allows veins to show more clearly.
- Fat distribution: Lower body fat, particularly in lean individuals, reduces cushioning under the skin, increasing vein visibility.
- Genetics: Some people naturally have more pronounced venous patterns due to inherited traits.
- Age: As skin loses elasticity and thins over time, veins become more apparent.
In most cases, visible foot veins are simply a reflection of individual physiology rather than a health issue.
Common Causes of Prominent Foot Veins
Beyond natural anatomy, several everyday factors can make foot veins more noticeable:
Physical Activity and Blood Flow
Exercise increases circulation and causes temporary dilation of veins. During or after workouts—especially running or weight training—blood volume in the lower limbs rises, pushing veins closer to the skin’s surface. This effect usually resolves within minutes to hours post-exercise.
Heat and Temperature Changes
Warm environments cause blood vessels to dilate. Standing in hot weather or wearing non-breathable footwear can lead to transient vein prominence. Similarly, prolonged sitting with legs down enhances gravitational pooling, making veins more visible.
Hormonal Fluctuations
Women may notice increased vein visibility during menstruation, pregnancy, or while using hormonal contraceptives. Estrogen and progesterone affect vascular tone and fluid retention, which can influence how veins appear.
Dehydration
When the body is dehydrated, blood volume decreases slightly, causing veins to constrict and sometimes appear more defined. While counterintuitive, dehydration can also reduce tissue turgor, making superficial structures like veins stand out.
When Vein Visibility Signals a Health Concern
While most cases are benign, certain signs suggest a need for medical evaluation. Persistent or worsening symptoms could indicate circulatory problems such as venous insufficiency, varicose veins, or deep vein thrombosis (DVT).
Chronic Venous Insufficiency (CVI)
This condition occurs when valves in leg veins fail to function properly, allowing blood to pool in the lower extremities. Symptoms include:
- Swollen, achy feet or ankles
- Heaviness or cramping in the legs
- Itchy or discolored skin near the ankles
- Development of varicose veins beyond the feet
“Persistent swelling and skin changes around the ankle should never be ignored—they can be early signs of chronic venous disease.” — Dr. Lena Torres, Vascular Medicine Specialist
Varicose and Spider Veins
Though typically associated with legs, varicose veins can develop on the feet due to pressure buildup. These veins are enlarged, twisted, and often bluish-purple. Spider veins are smaller but may cluster in web-like patterns.
Deep Vein Thrombosis (DVT)
A potentially life-threatening condition where a blood clot forms in a deep vein, usually in the leg. Warning signs include:
- Sudden swelling in one foot or calf
- Redness or warmth over the area
- Sharp or throbbing pain, especially when walking
DVT requires immediate medical attention due to the risk of pulmonary embolism.
Do’s and Don’ts: Managing Vein Health in Your Feet
| Do’s | Don’ts |
|---|---|
| Elevate your feet when resting to improve circulation | Stand or sit for hours without moving |
| Wear compression socks if recommended by a doctor | Ignore persistent swelling or discoloration |
| Stay hydrated and maintain healthy body weight | Cross your legs tightly for extended periods |
| Engage in regular low-impact exercise (walking, swimming) | Wear tight shoes or high heels daily |
| Monitor changes and take photos for comparison | Self-diagnose serious vascular conditions |
Real-Life Example: Recognizing a Warning Sign
Mark, a 47-year-old office worker, noticed his left foot had become increasingly veiny over six months. Initially dismissing it as aging, he began experiencing mild swelling and a dull ache after workdays. One morning, his ankle appeared redder than usual and felt warm to the touch. He consulted a vascular specialist, who diagnosed early-stage venous insufficiency. With lifestyle adjustments and graduated compression therapy, Mark reversed symptom progression and prevented complications.
His story underscores the importance of paying attention to subtle changes—not just appearance, but sensation and function.
Step-by-Step Guide to Assessing Foot Vein Changes
- Observe regularly: Check both feet in consistent lighting. Note symmetry and any new bulges or discoloration.
- Check for symptoms: Ask yourself: Is there pain, itching, swelling, or heaviness?
- Elevate and wait: Raise your feet above heart level for 15 minutes. Do veins diminish in size?
- Review lifestyle factors: Consider recent activity levels, shoe choices, travel, or hormonal shifts.
- Consult a professional: If changes persist beyond a few days or worsen, see a primary care provider or vascular specialist.
FAQ: Common Questions About Veiny Feet
Is it bad if my feet veins are very visible?
Not necessarily. Many healthy people have prominent foot veins due to genetics, low body fat, or fitness level. However, if accompanied by pain, swelling, or skin changes, seek evaluation.
Can being overweight or underweight affect vein visibility?
Yes. Underweight individuals often have less subcutaneous fat, making veins more visible. Overweight individuals may experience increased venous pressure, contributing to varicosities or poor circulation.
Should I wear compression socks for veiny feet?
Only if advised by a healthcare provider. Compression socks help with circulation but aren’t necessary for everyone. Misuse can cause skin irritation or restricted blood flow.
Conclusion: Know Your Body, Trust Your Instincts
Visible veins on the feet are usually a normal part of human variation. But your body communicates through changes—some subtle, some urgent. Learning the difference between cosmetic appearance and clinical warning signs empowers you to act wisely. Don’t dismiss persistent discomfort or asymmetrical changes. Early intervention can prevent minor issues from becoming major health concerns.
If you’ve noticed new or worsening vein patterns, take a moment to assess. Use the checklist and guidance here to determine next steps. When in doubt, consult a medical professional. Your vascular health is foundational to overall well-being—and worth protecting.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?