Leg aches are a frequent complaint across all age groups. Whether it’s a dull throb after a long day on your feet or a sharp pain that wakes you at night, discomfort in the legs can disrupt daily life. While many causes are benign and resolve with rest or minor lifestyle changes, some point to serious underlying conditions. Understanding what’s behind your leg pain—and knowing when to take action—can prevent complications and support faster recovery.
Common Causes of Leg Aching
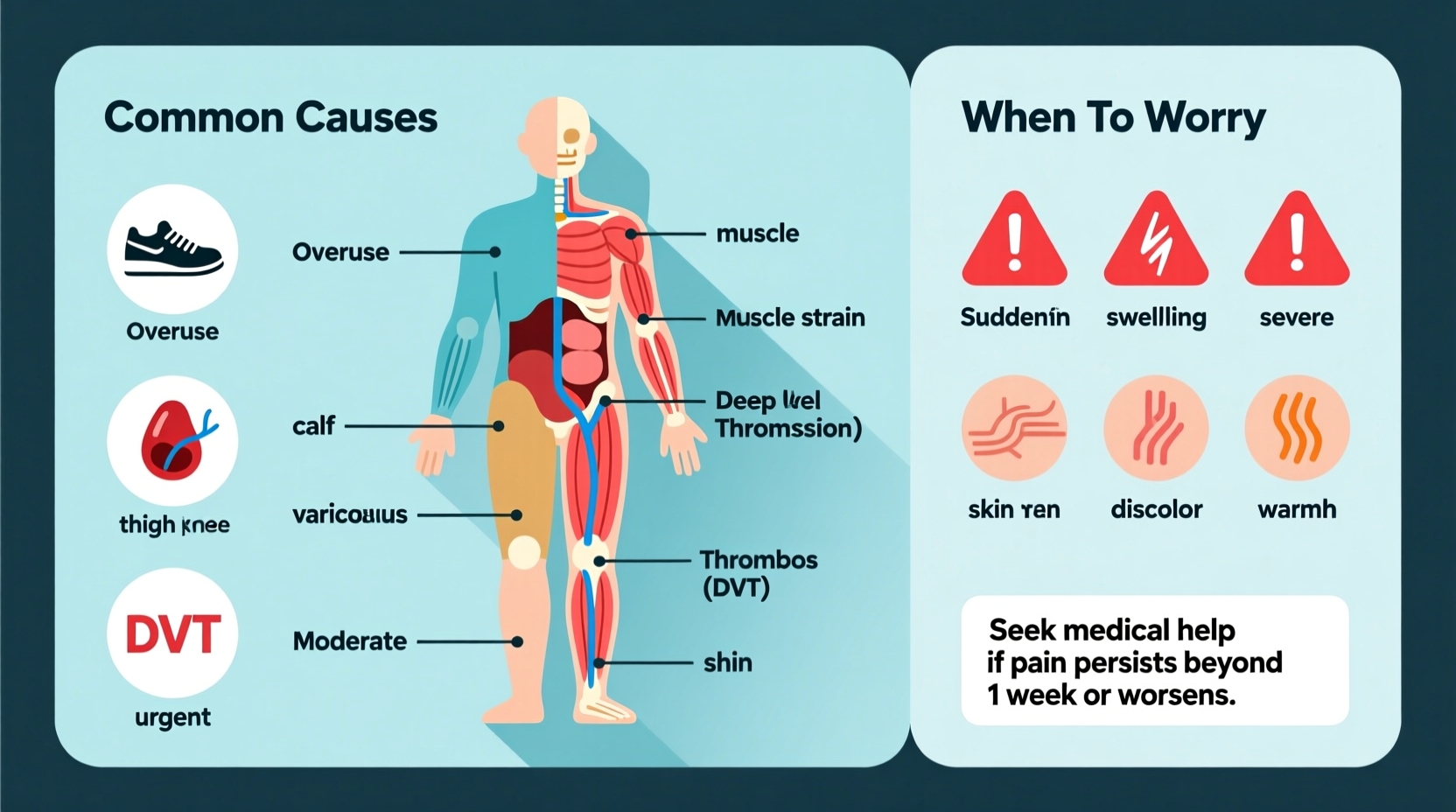
Leg pain arises from issues affecting muscles, nerves, blood vessels, bones, or joints. The location, type, and timing of the ache offer clues about its origin.
- Muscle strain or overuse: Exertion during exercise, prolonged standing, or sudden physical activity can lead to micro-tears in muscle fibers, causing soreness, especially in the calves or thighs.
- Varicose veins: Swollen, twisted veins due to poor circulation often cause a heavy, achy feeling in the lower legs, worsened by sitting or standing for long periods.
- Peripheral artery disease (PAD): Narrowed arteries reduce blood flow to the limbs, leading to cramping in the calves during walking—a symptom known as intermittent claudication.
- Nerve compression: Sciatica or lumbar spinal stenosis can radiate pain down the leg, often accompanied by tingling or numbness.
- Restless legs syndrome (RLS): An urge to move the legs, usually at night, paired with uncomfortable sensations, often described as crawling or aching.
- Deep vein thrombosis (DVT): A blood clot in a deep leg vein causes localized pain, swelling, warmth, and redness—this is a medical emergency.
When Leg Pain Signals Something Serious
Most leg aches are temporary and manageable at home. However, certain symptoms should not be ignored. These could indicate conditions requiring prompt medical evaluation.
“Persistent leg pain, especially with swelling or discoloration, should never be dismissed. It might be the only warning sign of a dangerous clot.” — Dr. Lena Torres, Vascular Medicine Specialist
Serious red flags include:
- Sudden, severe pain with swelling in one leg
- Warmth, redness, or visible bulging veins
- Chest pain or shortness of breath (possible pulmonary embolism)
- Loss of sensation, inability to move the leg, or foot drop
- Pain that worsens at rest or disrupts sleep consistently
- Sores that won’t heal, especially in people with diabetes
These signs may point to DVT, arterial blockage, infection, or nerve damage. Immediate assessment can be life-saving.
Do’s and Don’ts: Managing Leg Discomfort at Home
| Do | Avoid |
|---|---|
| Elevate legs above heart level for 15–20 minutes several times a day | Sitting or standing in one position for too long |
| Stay hydrated and maintain electrolyte balance | Ignoring persistent swelling or discoloration |
| Wear supportive footwear and consider compression stockings if advised | Self-treating suspected clots with massage or heat |
| Stretch gently, especially after prolonged sitting | Overusing NSAIDs without medical guidance |
| Walk regularly to promote circulation | Smoking, which impairs vascular health |
Real-Life Scenario: Recognizing DVT Early
Sarah, a 48-year-old office worker, began noticing a deep ache in her left calf after a week of working from home. She assumed it was from sitting too long. Over three days, the pain intensified, the calf became warm and slightly swollen, and she felt unusually tired. Concerned, she visited urgent care. An ultrasound confirmed a deep vein thrombosis. Thanks to early detection, she started anticoagulant therapy immediately and avoided a potential pulmonary embolism.
Sarah’s case highlights how seemingly ordinary discomfort can mask a dangerous condition. Had she waited longer, the outcome could have been far worse.
Step-by-Step Guide: Responding to Leg Pain
Follow this timeline to assess and act on leg aches appropriately:
- Day 1 – Monitor symptoms: Note the location, intensity, and triggers of pain. Is it bilateral or one-sided? Does movement improve or worsen it?
- Days 2–3 – Try conservative care: Rest, elevate, apply cold or warm compresses, hydrate, and stretch gently. Use over-the-counter pain relief if needed.
- Day 4 – Reassess: If pain persists or worsens, especially with swelling, redness, or fever, contact a healthcare provider.
- Immediate action if red flags present: Seek emergency care for sudden swelling, chest pain, or breathing difficulty.
- Follow-up: Schedule a visit with your doctor for chronic or recurring leg pain, particularly if you have risk factors like diabetes, obesity, or a history of blood clots.
Prevention Checklist
Reduce your risk of recurrent leg aches with these proactive steps:
- ✅ Stay physically active with regular walking or low-impact exercise
- ✅ Maintain a healthy weight to reduce pressure on legs and veins
- ✅ Avoid crossing legs while sitting to preserve circulation
- ✅ Wear compression socks during long flights or extended standing
- ✅ Quit smoking to improve vascular function
- ✅ Manage chronic conditions like diabetes and high blood pressure
- ✅ Stretch daily, focusing on hamstrings, calves, and hip flexors
Frequently Asked Questions
Why do my legs ache at night?
Nighttime leg aches can stem from restless legs syndrome, poor circulation, nerve issues, or muscle fatigue. Dehydration or low magnesium levels may also contribute. If the pain interferes with sleep regularly, consult a doctor to rule out neuropathy or vascular problems.
Can dehydration cause leg pain?
Yes. Inadequate fluid intake leads to electrolyte imbalances, increasing the risk of muscle cramps and spasms, especially in the calves. Athletes and older adults are particularly vulnerable. Drinking water throughout the day and consuming potassium- and magnesium-rich foods can help prevent this.
Is leg pain a sign of heart problems?
Not directly, but it can signal circulatory issues linked to cardiovascular disease. Peripheral artery disease, which causes leg pain during activity, shares risk factors with heart disease—such as smoking, high cholesterol, and hypertension. Treating PAD often reduces overall cardiovascular risk.
Conclusion: Listen to Your Body
Occasional leg aches are normal, especially after physical exertion. But persistent, worsening, or one-sided pain demands attention. By understanding the common causes—from overuse to vascular disorders—you empower yourself to respond wisely. Simple habits like staying active, staying hydrated, and avoiding prolonged immobility go a long way in prevention. When in doubt, err on the side of caution and consult a healthcare professional. Your legs carry you through life; treat them with the care they deserve.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?