For many people who menstruate, cramps are a monthly reality. While mild discomfort is normal, severe pain that interferes with daily life is not something you should simply endure. Understanding the reasons behind intense menstrual cramps—and knowing when they signal a deeper issue—is essential for long-term health and well-being.
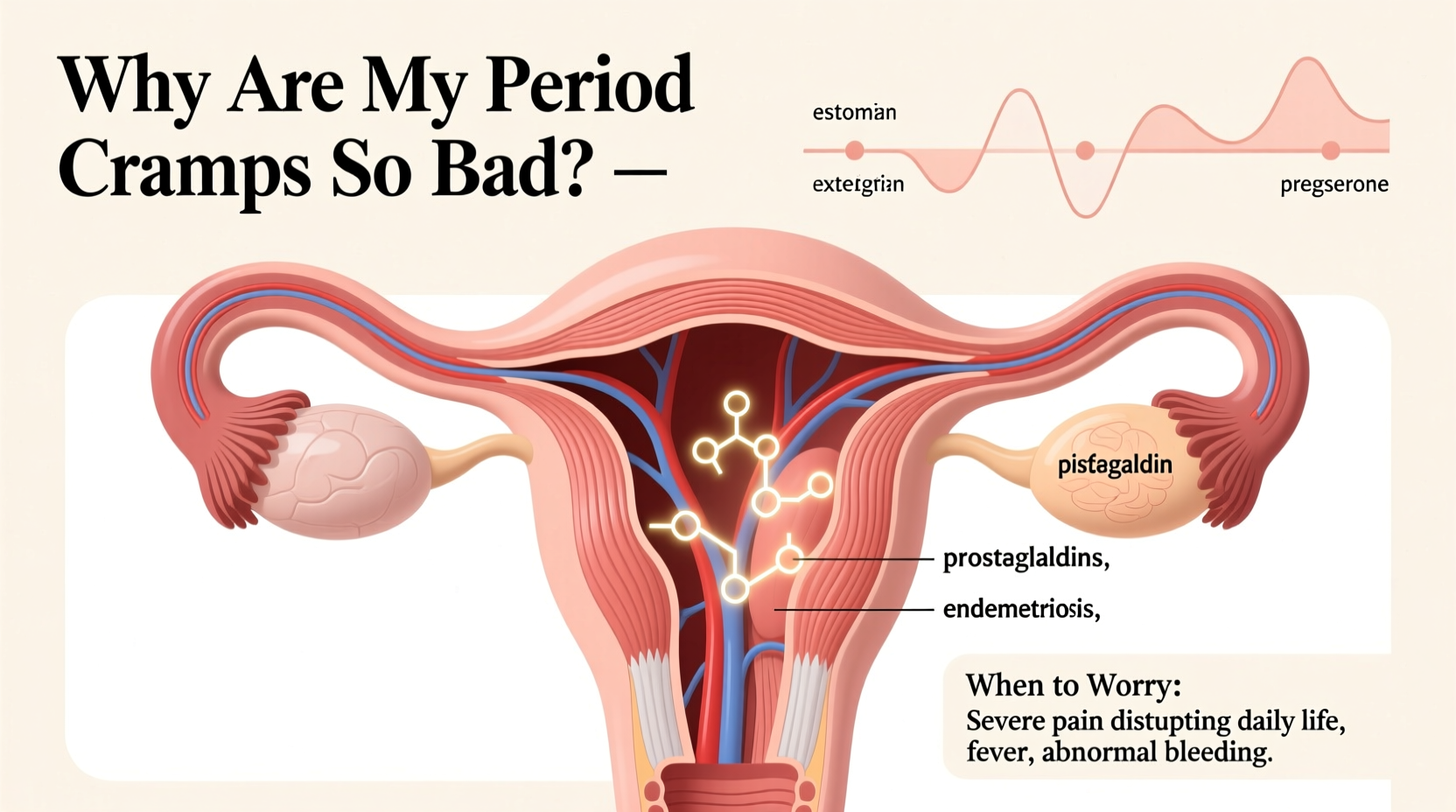
Period pain, or dysmenorrhea, occurs when the uterus contracts to shed its lining. These contractions are triggered by hormone-like substances called prostaglandins. Higher levels of prostaglandins are linked to stronger, more painful cramps. But when pain becomes debilitating—forcing you to miss work, school, or social events—it’s time to look beyond typical menstrual discomfort.
Primary vs. Secondary Dysmenorrhea: What’s the Difference?
There are two main types of menstrual cramps: primary and secondary dysmenorrhea.
- Primary dysmenorrhea begins shortly after menstruation starts, typically in adolescence. It's caused by natural chemical processes in the body, mainly elevated prostaglandin levels, and isn't linked to any underlying condition.
- Secondary dysmenorrhea develops later in life and is often due to an identifiable medical issue affecting the reproductive organs. Pain may start earlier in the cycle and last longer than typical cramps.
While primary cramps tend to improve with age or after childbirth, secondary dysmenorrhea usually worsens over time without treatment.
Common Causes of Severe Period Cramps
Several factors can intensify menstrual pain. Some are lifestyle-related; others point to medical conditions requiring attention.
1. High Prostaglandin Levels
The body releases prostaglandins to stimulate uterine contractions. When levels are too high, contractions become stronger and more painful, sometimes restricting blood flow to the uterus.
2. Endometriosis
A condition where tissue similar to the uterine lining grows outside the uterus—on the ovaries, fallopian tubes, or pelvic lining. This tissue still responds to hormonal changes, bleeding each month but with no way to exit the body. The result is inflammation, scarring, and severe pain.
3. Uterine Fibroids
Noncancerous growths in the uterine wall that can cause heavy bleeding and intense cramping. Larger fibroids may press on nearby organs, leading to bloating, frequent urination, or pelvic pressure.
4. Adenomyosis
This occurs when endometrial tissue grows into the muscular wall of the uterus, causing it to enlarge. Symptoms include prolonged, heavy periods and deep, aching cramps.
5. Pelvic Inflammatory Disease (PID)
An infection of the reproductive organs, often stemming from untreated sexually transmitted infections. PID can lead to chronic pelvic pain and fertility issues if not addressed early.
6. Ovarian Cysts
Fluid-filled sacs on the ovaries that may rupture or twist, causing sudden, sharp pain. Most cysts are harmless, but large or persistent ones can contribute to discomfort during menstruation.
When to Worry: Red Flags That Demand Medical Attention
Not all severe cramps indicate a serious problem, but certain symptoms should never be ignored. These are signs that your pain may stem from an underlying condition requiring diagnosis and treatment.
| Symptom | Possible Implication | Action Step |
|---|---|---|
| Pain lasting more than 2–3 days into your period | Endometriosis or adenomyosis | Consult a gynecologist for imaging or laparoscopy |
| Heavy bleeding soaking through pads hourly | Fibroids or hormonal imbalance | Seek evaluation for anemia and structural causes |
| Pain during sex (dyspareunia) | Endometriosis or pelvic adhesions | Discuss with doctor; consider ultrasound |
| Nausea, vomiting, or diarrhea with cramps | Elevated prostaglandins or endometriosis | Track symptoms and report severity |
| Inability to perform daily activities despite medication | Severe dysmenorrhea needing intervention | Request further investigation beyond ibuprofen |
“Severe menstrual pain is not a normal part of being a woman. If someone is missing school, work, or life because of their period, they deserve a thorough evaluation.” — Dr. Alicia Nguyen, OB-GYN and Women’s Health Advocate
Managing and Reducing Menstrual Pain
Whether your cramps are mild or severe, several strategies can help reduce discomfort and improve quality of life.
Diet and Lifestyle Adjustments
- Reduce intake of red meat, caffeine, and sugar, which can increase inflammation.
- Increase omega-3 fatty acids (found in fish, flaxseeds) to help regulate prostaglandins.
- Stay hydrated to minimize bloating and muscle tension.
Exercise and Heat Therapy
Gentle movement like walking or yoga improves blood flow and releases endorphins, the body’s natural painkillers. Applying a heating pad to the lower abdomen relaxes uterine muscles and reduces cramping intensity.
Over-the-Counter Medications
NSAIDs like ibuprofen or naproxen are most effective when taken at the first sign of pain—or even a day before your period starts—to block prostaglandin production.
Hormonal Treatments
Birth control pills, patches, rings, or IUDs (like Mirena) can significantly reduce or eliminate menstrual pain by thinning the uterine lining and suppressing ovulation. They’re often prescribed for both symptom relief and long-term management of conditions like endometriosis.
Mini Case Study: Recognizing Endometriosis Early
Sophia, a 24-year-old graduate student, had experienced worsening period pain since her late teens. She assumed it was normal until she began fainting from the pain during exams. Over-the-counter painkillers stopped working, and she missed multiple classes each month. After visiting a specialist, an ultrasound and laparoscopy confirmed stage III endometriosis. With a combination of hormonal therapy and minimally invasive surgery, her symptoms improved dramatically within six months. Her story highlights how delayed diagnosis can impact education, career, and mental health—but also how timely intervention can restore function and comfort.
Checklist: When to See a Doctor About Your Cramps
- Cramps prevent you from going to work, school, or social events.
- Pain persists beyond the first few days of your period.
- You experience pain during intercourse.
- Bleeding is so heavy you change pads or tampons every hour.
- Nausea, vomiting, dizziness, or fainting accompany your cramps.
- Pain doesn’t improve with NSAIDs or heat therapy.
- You’ve started having cramps later in life after years of normal periods.
Frequently Asked Questions
Can stress make my period cramps worse?
Yes. Chronic stress affects hormone balance and increases sensitivity to pain. Elevated cortisol can disrupt the menstrual cycle and amplify discomfort. Stress management techniques like mindfulness, breathing exercises, or therapy may help reduce symptom severity.
Is it possible to have endometriosis without a family history?
Absolutely. While genetics can play a role, endometriosis can develop in anyone regardless of family history. Environmental factors, immune system function, and retrograde menstruation are also contributing theories.
Do birth control methods stop period cramps completely?
They don’t work for everyone, but many people experience significant reduction—or complete elimination—of cramps while using hormonal contraception. Continuous regimens (skipping placebo pills) can even stop periods altogether, which often provides the greatest relief for those with severe dysmenorrhea.
Take Control of Your Menstrual Health
Severe period cramps are not something you must accept as inevitable. While some discomfort is common, debilitating pain is a signal—not a sentence. By understanding potential causes, tracking your symptoms, and advocating for proper care, you can uncover the root of your pain and find effective solutions.
If your cramps are disrupting your life, don’t wait. Schedule an appointment with a healthcare provider who listens, believes your experience, and is willing to investigate further. Whether it’s adjusting your diet, starting medication, or exploring diagnostic tests, taking action today can lead to meaningful relief tomorrow.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?