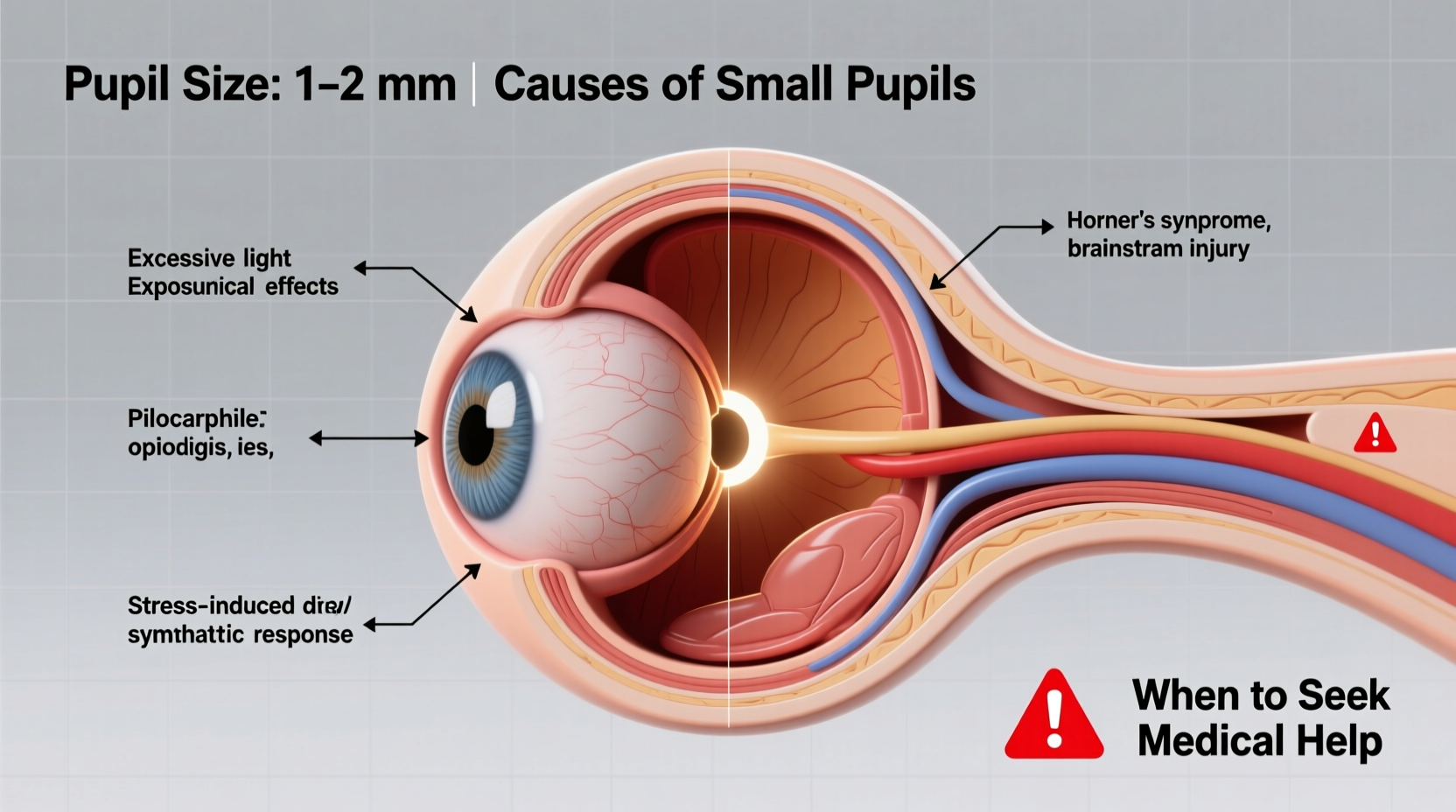
Pupil size is a dynamic feature of the eye, constantly adjusting in response to light, emotions, medications, and overall neurological function. While most people focus on dilated (enlarged) pupils, persistently small or abnormally constricted pupils—known medically as miosis—can also signal underlying issues. Understanding why your pupils might be smaller than usual, recognizing associated symptoms, and knowing when to seek medical evaluation can help protect both your vision and overall health.
What Controls Pupil Size?
The size of your pupils is regulated by two sets of muscles in the iris: the sphincter pupillae, which constricts the pupil, and the dilator pupillae, which enlarges it. These muscles respond to signals from the autonomic nervous system—specifically the parasympathetic and sympathetic pathways. Light levels are the most immediate influence: in bright environments, pupils constrict to reduce light entry; in dim settings, they dilate. But beyond lighting, numerous internal and external factors can lead to sustained miosis.
Common Causes of Small Pupils
Small pupils are not always a cause for alarm. Many everyday influences can temporarily or consistently reduce pupil size. These include:
- Low light adaptation aftermath: After prolonged exposure to bright light, pupils may remain slightly constricted even when moving into darker areas.
- Aging: As people age, the muscles in the iris lose some responsiveness, often resulting in smaller baseline pupil size.
- Focusing on near objects: The pupillary reflex during close-up tasks like reading naturally causes constriction.
- Emotional states: Concentration, fear, or mental effort can trigger temporary miosis via increased parasympathetic activity.
Medical and Pharmacological Causes
More concerning causes of small pupils involve medications, toxins, or medical conditions affecting the nervous system. Some of the most frequent contributors include:
Medications That Constrict Pupils
Certain drugs stimulate the parasympathetic nervous system or inhibit sympathetic tone, leading to miosis. Common examples:
| Medication Type | Examples | Mechanism |
|---|---|---|
| Opioids | Morphine, oxycodone, fentanyl | Activate mu-opioid receptors in the brainstem, increasing parasympathetic output |
| Glaucoma eye drops | Pilocarpine, carbachol | Directly contract the iris sphincter muscle |
| Organophosphate pesticides | Malathion, parathion | Inhibit acetylcholinesterase, causing excess acetylcholine and pupil constriction |
| Some antipsychotics and antiepileptics | Clonidine, reserpine | Reduce central sympathetic outflow |
If you're taking any of these medications, especially opioids or glaucoma treatments, small pupils may be an expected side effect. However, sudden or asymmetric changes should still prompt evaluation.
Neurological Conditions Linked to Miosis
Sustained unilateral (one-sided) miosis can indicate a neurological disorder. One of the most notable is Horner’s syndrome, which results from disruption of the sympathetic nerve pathway to the eye.
Horner’s syndrome typically presents with a triad of symptoms:
- Constricted pupil (miosis)
- Drooping eyelid (ptosis)
- Lack of facial sweating (anhidrosis) on the affected side
Causes of Horner’s syndrome range from benign (like cluster headaches) to life-threatening (such as carotid artery dissection, tumors in the lung apex, or stroke). A key diagnostic clue is that the affected pupil will dilate more slowly in the dark compared to the healthy side.
“Persistent unequal pupil size, especially when accompanied by eyelid droop or facial asymmetry, warrants urgent neuroimaging.” — Dr. Lena Patel, Neuro-Ophthalmologist at Boston Vision Institute
Other Neurological Concerns
Severe brain injuries, pontine strokes, or opioid overdoses can also lead to pinpoint pupils. In cases of pontine hemorrhage, for example, bilateral miosis is often one of the earliest signs due to disruption of sympathetic pathways in the brainstem.
When to Worry: Red Flags for Small Pupils
While small pupils alone aren’t necessarily dangerous, certain accompanying symptoms suggest a need for immediate medical attention. Be alert for:
- Pinpoint pupils unresponsive to dim light
- Unequal pupil size (anisocoria) that’s new or worsening
- Drooping eyelids or facial asymmetry
- Headaches, dizziness, or vision changes
- Nausea, confusion, or respiratory depression – especially if opioid use is suspected
- Recent head or neck trauma
Mini Case Study: Recognizing Horner’s Syndrome Early
James, a 52-year-old construction worker, noticed his left pupil had become smaller over several weeks. He also observed mild drooping of the left eyelid and less sweating on that side of his face. Initially dismissing it as fatigue, he visited an optometrist during a routine exam. The clinician recognized the pattern of Horner’s syndrome and referred him urgently. Imaging revealed a tumor at the top of his left lung—a Pancoast tumor—impacting the sympathetic chain. Early detection allowed for timely treatment, including surgery and radiation, significantly improving his prognosis.
This case underscores the importance of not ignoring subtle ocular changes. Even seemingly minor pupil differences can be the first sign of serious systemic disease.
Step-by-Step: What to Do If You Notice Small Pupils
- Assess the context: Are you in bright light? Reading closely? Taking new medication?
- Check symmetry: Look in a mirror or ask someone to observe both pupils in dim and bright light.
- Review medications: List all prescriptions, supplements, and eye drops you’re using.
- Note additional symptoms: Record any headaches, vision changes, eyelid droop, or neurological issues.
- Seek professional evaluation: Consult an ophthalmologist, neurologist, or primary care provider for assessment.
- Follow through with testing: Depending on suspicion, tests may include cocaine or apraclonidine eye drop tests, MRI, CT, or carotid ultrasound.
FAQ
Can stress cause small pupils?
Stress typically activates the sympathetic nervous system, leading to dilated pupils. However, intense concentration or anxiety involving focused visual tasks may indirectly contribute to temporary miosis. Chronic stress alone is unlikely to cause persistent small pupils.
Are small pupils reversible?
Yes, in many cases. If caused by medication, pupil size often returns to normal after discontinuation. In neurological cases, recovery depends on treating the underlying condition. Some damage, such as from a stroke or tumor, may result in permanent miosis.
Is it normal for pupils to be different sizes?
Up to 20% of people have slight natural anisocoria (unequal pupils) of less than 1 mm, which remains stable over time and isn't associated with other symptoms. However, new-onset or changing anisocoria requires evaluation.
Checklist: When to Seek Immediate Medical Help
- ☑ Pupils remain pinpoint even in low light
- ☑ Sudden onset of unequal pupil size
- ☑ Drooping eyelid or facial weakness
- ☑ Severe headache or neck pain
- ☑ Confusion, difficulty speaking, or weakness on one side of the body
- ☑ Known or suspected opioid overdose
- ☑ Recent trauma to head or neck
Conclusion
Small pupils can stem from harmless, everyday causes—or they can be early warning signs of serious medical conditions. The key lies in context: duration, symmetry, associated symptoms, and medication use all matter. Never dismiss persistent or asymmetric miosis without professional input. Your eyes are windows not just to the world, but to your brain and nervous system. Paying attention to changes in pupil size empowers you to act early, potentially preventing complications or catching treatable conditions before they escalate.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?