Sinus infections—medically known as sinusitis—affect millions of people each year. While occasional congestion or mild inflammation is normal, some individuals seem to battle recurring sinus issues with frustrating frequency. If you're asking, \"Why are my sinuses so susceptible to infection?\" you're not alone. The answer lies in a combination of anatomical, environmental, immunological, and lifestyle factors that influence how well your sinuses function and defend against pathogens.
The sinuses are air-filled cavities in the skull that produce mucus, which helps trap dust, allergens, and microbes. When drainage pathways become blocked or inflamed, mucus accumulates, creating an ideal breeding ground for bacteria and viruses. Understanding what makes your sinuses vulnerable is the first step toward lasting relief.
Anatomical Factors That Increase Susceptibility
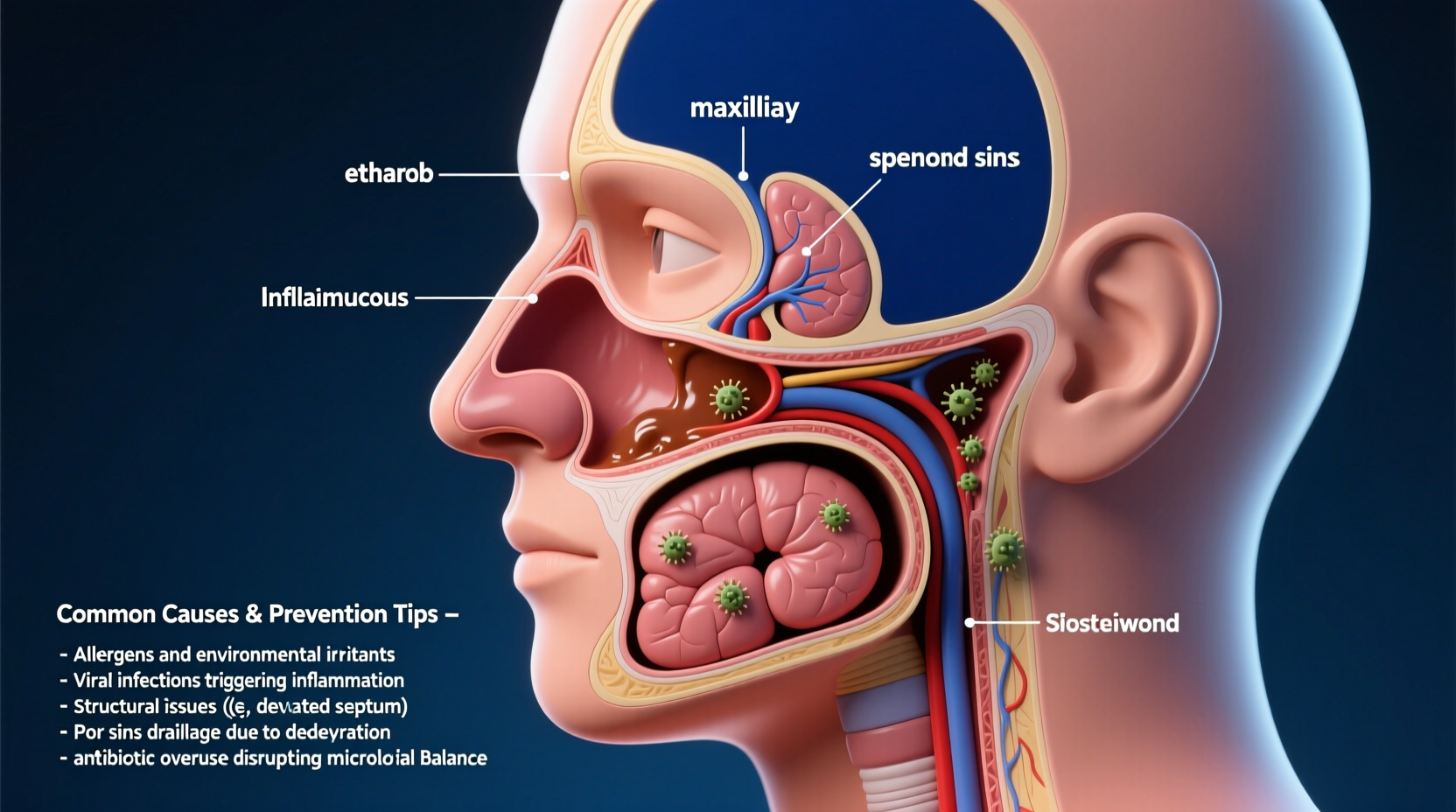
Your physical structure plays a significant role in sinus health. Some people are born with narrow sinus passages or deviated septums, which can impede proper mucus drainage. A deviated nasal septum—where the thin wall between nostrils is displaced to one side—can block airflow and lead to chronic congestion.
Other structural issues include:
- Nasal polyps: Noncancerous growths that obstruct nasal passages.
- Enlarged turbinates: Bony structures inside the nose that swell due to irritation or allergies.
- Concha bullosa: An air-filled middle turbinate that narrows sinus openings.
These conditions don’t always cause symptoms, but under stress from allergens or illness, they can turn minor irritation into full-blown sinusitis.
“Anatomical variations are common, but when combined with environmental triggers, they significantly increase the risk of chronic sinus disease.” — Dr. Lena Patel, Otolaryngologist at Boston Sinus Center
Environmental and Lifestyle Triggers
Even with optimal anatomy, external factors can compromise sinus health. Urban living, indoor pollutants, and seasonal changes all contribute to increased vulnerability.
Common environmental irritants include:
- Tobacco smoke (firsthand or secondhand)
- Dust mites and pet dander
- Mold spores in damp environments
- Strong perfumes, cleaning agents, and chemical fumes
- Dry indoor air from heating or air conditioning systems
Lifestyle habits also play a role. Dehydration thickens mucus, making it harder to clear. Poor sleep weakens immune defenses, while diets high in processed foods may promote systemic inflammation.
Underlying Health Conditions Linked to Recurrent Infections
Chronic sinus issues are often symptoms of deeper health imbalances. Identifying and managing these conditions is essential for long-term improvement.
| Condition | How It Affects Sinuses | Management Approach |
|---|---|---|
| Allergic Rhinitis | Triggers inflammation and excess mucus production | Allergy testing, antihistamines, nasal corticosteroids |
| Asthma | Linked to chronic upper airway inflammation | Inhalers, anti-inflammatory meds, trigger avoidance |
| Gastroesophageal Reflux Disease (GERD) | Acid reflux irritates throat and sinuses | Diet modification, proton-pump inhibitors |
| Immune Deficiency Disorders | Reduced ability to fight off infections | Blood tests, immunoglobulin therapy if needed |
| Cystic Fibrosis | Produces thick mucus that blocks sinuses | Specialized respiratory care, mucolytics |
If you experience more than four sinus infections per year, consider consulting an allergist or ENT specialist to rule out underlying disorders.
Step-by-Step Guide to Strengthening Sinus Resilience
Preventing recurrent infections requires a proactive, multi-layered strategy. Follow this timeline to build stronger sinus defenses over time.
- Week 1–2: Assess Your Environment
Identify and eliminate common irritants. Replace HVAC filters, wash bedding weekly in hot water, and remove mold-prone items like old shower curtains. - Week 3–4: Optimize Hydration and Diet
Drink at least 2 liters of water daily. Incorporate anti-inflammatory foods such as leafy greens, fatty fish, garlic, and citrus fruits. Reduce sugar and dairy, which can thicken mucus. - Month 2: Begin Nasal Hygiene Routine
Perform daily saline irrigation using a neti pot or squeeze bottle. This flushes out allergens and keeps mucous membranes hydrated. - Month 3: Evaluate Immune Function
Schedule blood work to check vitamin D levels, immune markers, and allergy profiles. Supplement if deficient—vitamin D and zinc are critical for mucosal immunity. - Ongoing: Monitor and Adjust
Keep a symptom journal tracking flare-ups, diet, sleep, and potential triggers. Use insights to refine your prevention plan.
Real-Life Example: Overcoming Chronic Sinusitis
Sarah, a 34-year-old teacher from Chicago, suffered from sinus infections nearly every winter for over a decade. Despite antibiotics and decongestants, her symptoms returned within weeks. After seeing an ENT specialist, she discovered she had both a deviated septum and undiagnosed mold allergies.
Her treatment plan included nasal corticosteroid sprays, saline rinses twice daily, and replacing her bedroom carpet (a reservoir for mold spores). She also started taking a probiotic and vitamin D supplement. Within six months, her infection frequency dropped from five per year to just one mild episode.
Sarah’s case highlights how combining medical evaluation with consistent self-care can transform chronic susceptibility into lasting relief.
Essential Tips for Daily Sinus Protection
Checklist: Daily Habits to Prevent Sinus Infections
- ✅ Perform saline nasal rinse (morning or evening)
- ✅ Drink 8–10 glasses of water
- ✅ Avoid known allergens or irritants
- ✅ Use a HEPA air purifier in bedrooms
- ✅ Practice stress-reducing techniques (e.g., deep breathing, meditation)
- ✅ Get 7–8 hours of quality sleep
Frequently Asked Questions
Can allergies really cause sinus infections?
Yes. Allergies provoke inflammation in the nasal passages, leading to swelling and blocked sinus drainage. This stagnant mucus becomes a breeding ground for bacteria, increasing the risk of secondary bacterial infection.
Are antibiotics always necessary for sinus infections?
No. Most acute sinus infections are viral and resolve on their own within 7–10 days. Antibiotics are only effective against bacterial infections and should be used sparingly to prevent resistance. Your doctor can determine if antibiotics are appropriate based on symptom duration and severity.
Is it safe to use nasal sprays every day?
It depends on the type. Saline sprays and steroid nasal sprays (like fluticasone) are generally safe for daily, long-term use. However, decongestant sprays (such as oxymetazoline) should not be used for more than 3 consecutive days, as they can cause rebound congestion.
Take Control of Your Sinus Health
Recurrent sinus infections don’t have to be your normal. By understanding the root causes—whether anatomical, environmental, or immunological—you gain the power to make informed changes. Small, consistent actions like staying hydrated, cleaning your indoor air, and practicing nasal hygiene can dramatically reduce your risk over time.
If you’ve been battling frequent sinus issues, don’t settle for temporary fixes. Seek professional evaluation, implement sustainable habits, and give your body the tools it needs to maintain clear, healthy sinuses year-round.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?