Hard stools are a common digestive issue that can range from mildly uncomfortable to severely painful. They often signal constipation, but the root causes vary widely — from diet and hydration to medications and underlying health conditions. While occasional hard bowel movements are normal, persistent issues can affect quality of life and may indicate a need for lifestyle changes or medical evaluation. Understanding the triggers, how to prevent them, and when to take action is essential for maintaining digestive wellness.
What Causes Hard Stools?
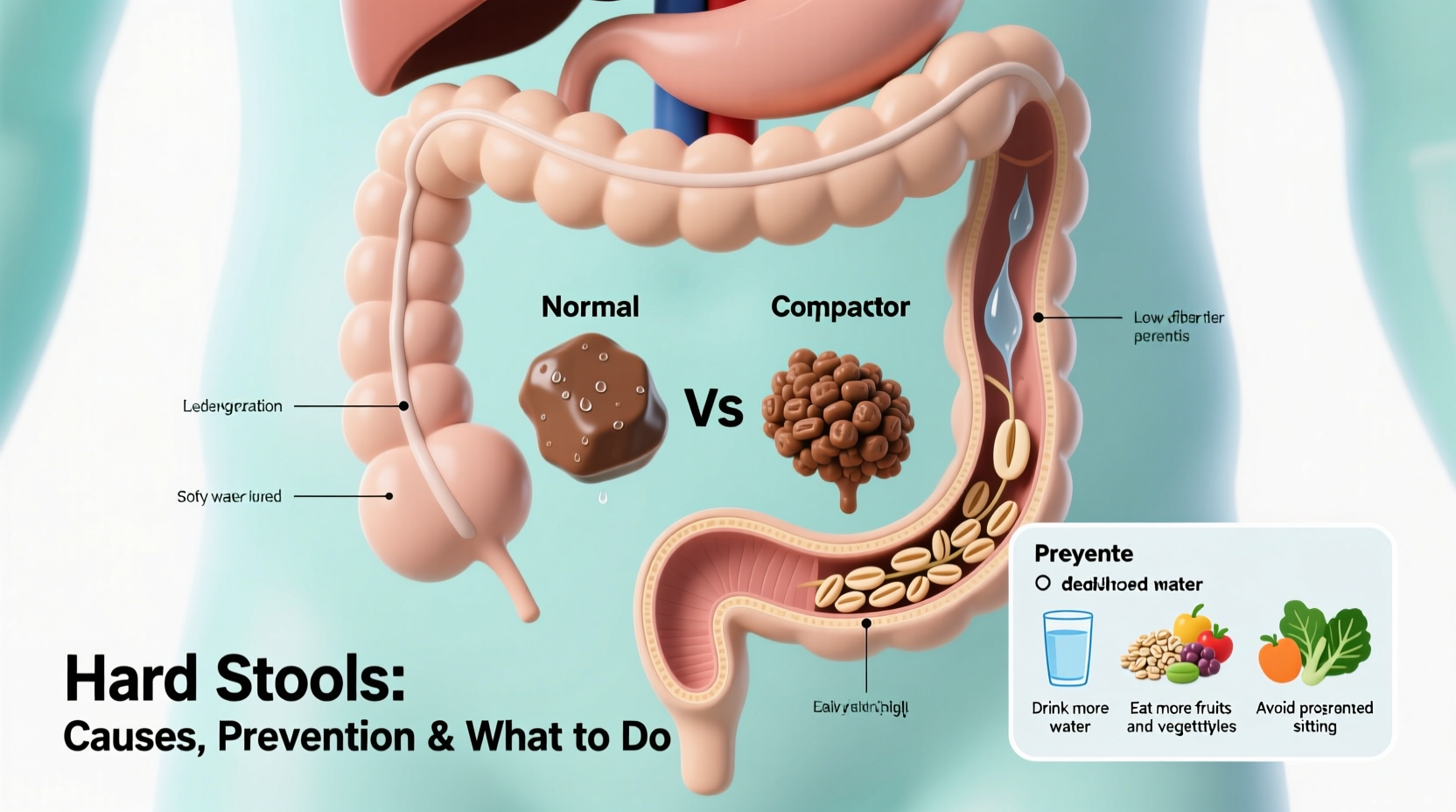
Stool hardness occurs when waste moves too slowly through the digestive tract, allowing the colon to absorb excess water. The result is dry, compacted feces that are difficult to pass. Several factors contribute to this slowdown:
- Inadequate fiber intake: Fiber adds bulk and softness to stool. A diet low in fruits, vegetables, legumes, and whole grains reduces intestinal motility.
- Dehydration: Not drinking enough fluids leads to drier stools. Water helps keep stool soft and promotes smooth transit.
- Sedentary lifestyle: Physical inactivity slows digestion. Regular movement stimulates intestinal contractions.
- Ignoring the urge to go: Delaying bowel movements allows more water absorption, making stool harder over time.
- Medications: Opioids, certain antidepressants, iron supplements, and some blood pressure drugs can cause constipation.
- Medical conditions: Irritable bowel syndrome (IBS), hypothyroidism, diabetes, and neurological disorders like Parkinson’s disease may impair bowel function.
- Changes in routine: Travel, stress, or altered eating patterns disrupt regularity.
“Chronic hard stools aren’t something to ignore. They can lead to complications like hemorrhoids or anal fissures if left unmanaged.” — Dr. Lena Torres, Gastroenterologist
Prevention: Building Better Bowel Habits
Preventing hard stools isn’t about quick fixes — it’s about consistent, sustainable habits. The foundation of healthy digestion lies in daily routines that support gut motility and hydration.
Dietary Adjustments That Work
Increase both soluble and insoluble fiber gradually. Soluble fiber (found in oats, apples, beans) forms a gel-like substance that softens stool, while insoluble fiber (in whole wheat, broccoli, nuts) adds bulk and speeds transit.
Aim for 25–30 grams of fiber daily. Sudden increases can cause bloating, so add fiber slowly and drink plenty of water to help it move through the system.
Hydration Matters More Than You Think
Water is critical. Without enough fluid, fiber cannot do its job effectively. Many people underestimate their daily needs. As a general rule, aim for at least 8 cups (64 ounces), more if you're active or live in a hot climate.
Beverages like herbal teas, broths, and water-rich fruits (e.g., watermelon, oranges) also contribute to hydration. Limit caffeine and alcohol, which can dehydrate.
What to Do When Stools Are Already Hard
If you're already experiencing hard, difficult-to-pass stools, several safe interventions can bring relief.
- Boost fluid intake immediately: Drink water, clear soups, or electrolyte solutions to rehydrate and soften existing stool.
- Add high-fiber foods: Prunes, pears, kiwi, chia seeds, and bran cereals act as natural laxatives.
- Try gentle physical activity: A brisk walk or light stretching can stimulate bowel movement.
- Use over-the-counter aids cautiously: Options include osmotic laxatives (like polyethylene glycol), stool softeners, or glycerin suppositories. Avoid stimulant laxatives long-term without medical guidance.
- Adopt the optimal bathroom posture: Use a small footstool to elevate your knees above your hips, mimicking a squatting position. This aligns the rectum and eases passage.
| Action | Effectiveness | Time to Relief |
|---|---|---|
| Drink 2–3 glasses of water | Moderate (especially with fiber) | 6–24 hours |
| Eat 2–3 prunes | High (natural sorbitol effect) | 6–12 hours |
| Take polyethylene glycol (MiraLAX) | Very High | 12–72 hours |
| Use glycerin suppository | Immediate (local effect) | 15–60 minutes |
Real-Life Example: Maria’s Turnaround
Maria, a 42-year-old office worker, struggled with hard stools for months. She sat most of the day, drank little water, and relied on processed meals. After developing an anal fissure from straining, she consulted her doctor. With guidance, she began packing salads for lunch, set hourly reminders to drink water, and started walking 20 minutes after dinner. Within three weeks, her bowel movements normalized. “I didn’t realize how much my desk job was affecting my gut,” she said. “Small changes made a big difference.”
When to See a Doctor
Most cases of hard stools improve with lifestyle adjustments. However, seek medical advice if you experience any of the following:
- Constipation lasting more than two weeks despite home care
- Severe pain or bleeding during bowel movements
- Unexplained weight loss or fatigue
- Frequent reliance on laxatives
- Family history of colon cancer or inflammatory bowel disease
A healthcare provider may perform tests to rule out conditions like colorectal obstruction, slow-transit constipation, or pelvic floor dysfunction. In some cases, prescription medications or biofeedback therapy may be recommended.
Checklist: Your Action Plan for Softer Stools
✅ Daily Prevention Checklist:
- Drink at least 8 cups of water
- Eat 5 servings of fruits/vegetables
- Include whole grains or legumes in one meal
- Move your body for 30 minutes
- Respond promptly to bowel urges
- Avoid excessive dairy or red meat
- Limit processed foods and refined carbs
FAQ
Can stress really make my stools hard?
Yes. Chronic stress affects the enteric nervous system — often called the “second brain” of the gut. It can slow digestion and alter gut motility, contributing to constipation and harder stools.
Are bananas good or bad for hard stools?
It depends on ripeness. Unripe (green) bananas contain resistant starch, which can worsen constipation. Ripe bananas, with their softer texture and higher sugar content, are generally beneficial and provide fiber.
Is it dangerous to push hard when having a bowel movement?
Occasional straining is common, but chronic or forceful pushing increases the risk of hemorrhoids, rectal prolapse, and anal fissures. If you find yourself regularly straining, address the underlying cause rather than enduring it.
Conclusion: Take Control of Your Digestive Health
Hard stools are not just an inconvenience — they’re a signal from your body that something needs attention. Whether it’s adjusting your diet, moving more, or reevaluating medications, the power to improve your bowel health lies in consistent, informed choices. Don’t wait for discomfort to become chronic. Start today by hydrating, adding fiber, and listening to your body’s cues. Small steps lead to lasting change.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?