You may have noticed a faint transparency or glassy appearance at the bottom edges of your front teeth—particularly near the tips. This isn't just an optical illusion; translucent teeth can signal underlying dental issues, especially when it occurs along the lower edge or near the gumline. While mild translucency can be normal in thin areas of enamel, widespread or progressive transparency often points to enamel erosion or demineralization. Understanding why this happens and what you can do about it is essential for preserving both the health and aesthetics of your smile.
Understanding Tooth Enamel and Translucency
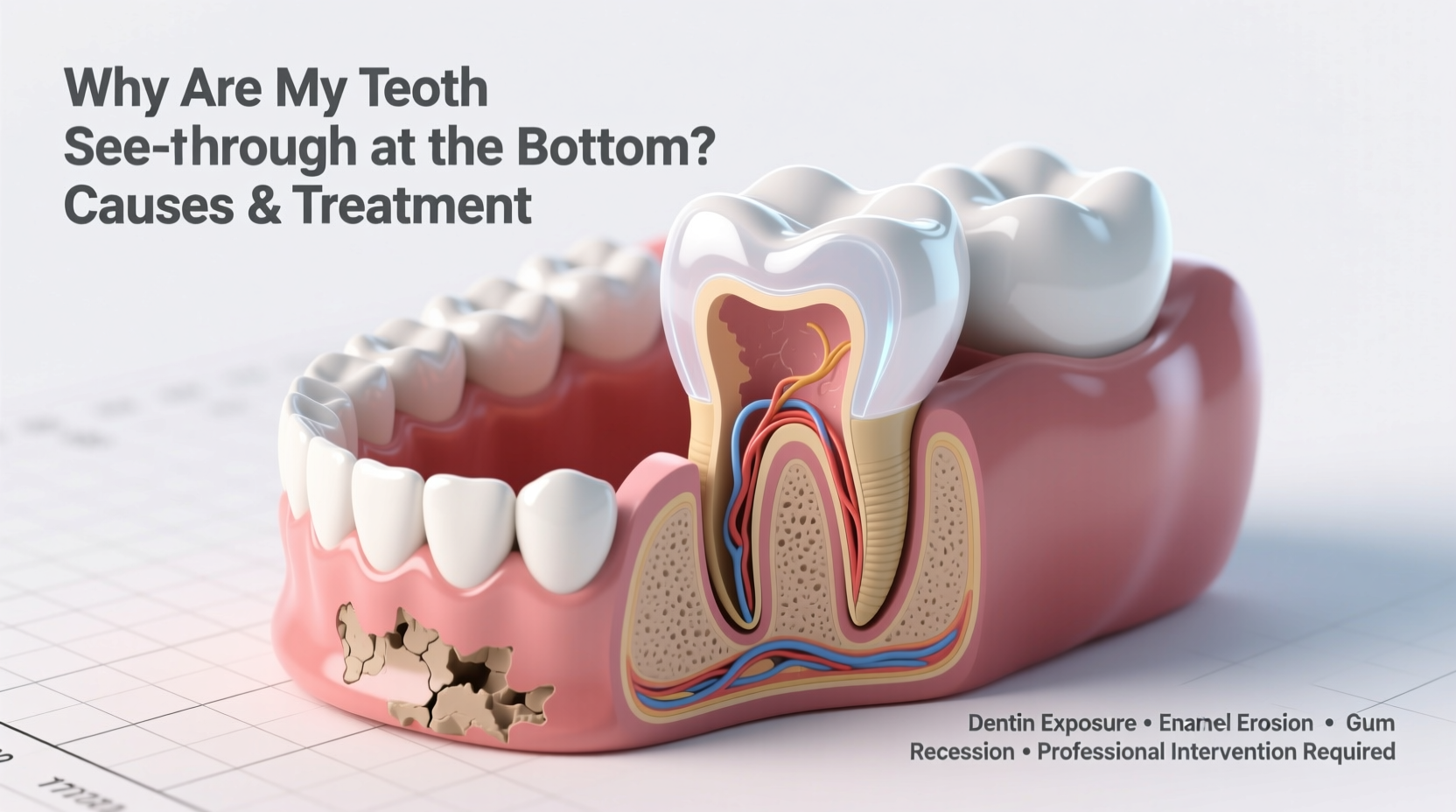
Tooth enamel is the hardest substance in the human body, designed to protect the inner layers of the tooth from decay and temperature changes. Healthy enamel is semi-translucent, which allows light to pass through slightly—this is why teeth aren’t completely opaque like plastic. However, when enamel wears down or loses minerals, it becomes thinner and more transparent, particularly at the edges where it’s naturally less dense.
The bottom edges of front teeth—especially central incisors—are common sites for visible translucency because these areas endure constant biting forces and are more prone to wear. When enamel thins here, the underlying dentin doesn’t extend all the way to the tip, leaving a translucent \"window\" effect that many describe as looking “see-through.”
“Translucency at the biting edges of teeth is often one of the first clinical signs of significant enamel loss,” says Dr. Lena Torres, a cosmetic dentist with over 15 years of experience in restorative care. “It's not always painful, but it’s a red flag we take seriously.”
Common Causes of See-Through Teeth at the Bottom
Several factors contribute to enamel thinning and the resulting transparent appearance. Identifying the root cause is critical for effective treatment and prevention.
- Acid Erosion (Dental Erosion): Frequent exposure to acidic foods and drinks—like citrus fruits, soda, sports drinks, and wine—softens enamel over time. Once softened, even gentle brushing can wear it away.
- Gastroesophageal Reflux Disease (GERD): Stomach acid that regularly reaches the mouth during acid reflux episodes can severely erode enamel, especially on the back surfaces and lower edges of teeth.
- Bulimia or Eating Disorders: Repeated vomiting exposes teeth to high concentrations of gastric acid, leading to rapid enamel degradation, often most noticeable on the lingual (tongue-side) surfaces and incisal edges.
- Bruxism (Teeth Grinding): Chronic grinding, especially during sleep, accelerates wear at the biting edges, thinning enamel and creating a translucent look.
- Poor Oral Hygiene or Overbrushing: Using a hard-bristled toothbrush or brushing too aggressively can abrade enamel, particularly near the gumline and tooth tips.
- Natural Aging: Enamel gradually wears down over decades, making mild translucency more common in adults over 30—but sudden or severe changes should never be dismissed as “just aging.”
Treatment Options Based on Severity
Restoring the appearance and strength of translucent teeth depends on how much enamel remains and the underlying cause. Early intervention prevents further damage and avoids costly restorations later.
| Condition | Treatment Approach | Expected Outcome |
|---|---|---|
| Mild Enamel Thinning | Fluoride treatments, remineralizing toothpaste (e.g., NovaMin or CPP-ACP), dietary adjustments | Improved enamel hardness, reduced sensitivity, stabilized translucency |
| Moderate Wear with Aesthetic Concerns | Dental bonding with composite resin to rebuild edges | Immediate improvement in appearance and protection of exposed areas |
| Severe Enamel Loss | Veneers or crowns to cover and strengthen compromised teeth | Long-term structural support and natural-looking restoration |
| Underlying Medical Cause (e.g., GERD) | Referral to physician, acid suppression therapy, custom night guard | Prevention of further erosion and systemic health improvement |
In-office fluoride varnishes applied every 3–6 months can help reharden early lesions. For patients with bruxism, a custom-fitted night guard redistributes grinding forces and protects vulnerable edges from additional wear.
Step-by-Step Guide to Protecting and Restoring Translucent Teeth
- Schedule a Dental Evaluation: Visit your dentist for a clinical assessment. They’ll examine enamel thickness, check for sensitivity, and possibly take intraoral photos to monitor progression.
- Identify and Eliminate Acid Sources: Keep a 3-day diet and symptom journal to track acidic intake and reflux episodes. Replace soda with water, and avoid snacking on citrus between meals.
- Switch to a Soft-Bristled Brush and Non-Abrasive Toothpaste: Use a toothpaste formulated for sensitivity and enamel protection (e.g., Sensodyne Repair & Protect or Colgate Sensitive Pro-Relief).
- Rinse After Acid Exposure: After eating or drinking something acidic—or after vomiting—swish with water or a baking soda solution (1 tsp in 1 cup water) to neutralize pH.
- Apply Remineralizing Agents Daily: Use a prescription-strength fluoride gel or over-the-counter products containing hydroxyapatite to support enamel repair.
- Consider Restorative Options: If translucency affects your confidence or leads to chipping, discuss bonding or veneers with your dentist.
- Monitor Progress Every 6 Months: Return for follow-up exams to ensure no further erosion is occurring.
Real-Life Example: Sarah’s Experience with Translucent Incisors
Sarah, a 28-year-old graphic designer, began noticing her front teeth looked “thin” and almost ghost-like at the tips. She didn’t have pain, but she avoided smiling widely in photos. During her dental checkup, her hygienist observed significant enamel loss on the incisal edges. Upon questioning, Sarah revealed she drank two energy drinks daily and often experienced heartburn at night. Her dentist diagnosed acid erosion compounded by undiagnosed GERD. After switching to a low-acid diet, using a prescription fluoride tray nightly, and starting antacid medication, her enamel stabilized within six months. She opted for minor bonding to restore the shape of her two central incisors, regaining both function and confidence.
FAQ
Can translucent teeth be reversed?
No, once enamel is lost, it cannot regenerate. However, early-stage demineralization can be stabilized and strengthened through remineralization therapies. The goal is to prevent further loss and restore appearance with cosmetic solutions if needed.
Is it normal for teeth to be see-through at the bottom?
A slight translucency at the very tip of front teeth can be normal, especially in younger individuals. But pronounced or spreading transparency—especially if accompanied by sensitivity or chipping—is not normal and requires evaluation.
Can whitening make translucent teeth worse?
Yes. Many whitening products increase enamel porosity and can exacerbate the see-through effect, particularly near the edges. Patients with existing enamel issues should avoid over-the-counter whitening and consult a dentist before any bleaching treatment.
Essential Prevention Checklist
- ✔️ Reduce consumption of acidic foods and drinks
- ✔️ Wait 30 minutes after eating/drinking before brushing
- ✔️ Use fluoride or hydroxyapatite toothpaste twice daily
- ✔️ Floss daily to prevent gum recession that exposes root surfaces
- ✔️ Wear a night guard if you grind your teeth
- ✔️ Treat acid reflux or eating disorders with medical support
- ✔️ Attend dental checkups every six months
Take Action Before It Gets Worse
Translucent teeth at the bottom edges are more than a cosmetic concern—they’re an early warning system. Left unaddressed, enamel erosion can lead to sensitivity, decay, chipping, and costly restorations. The good news is that with timely care, most cases can be managed effectively. Whether it’s adjusting your diet, improving oral hygiene habits, or seeking professional treatment, the steps you take today will determine the resilience of your smile tomorrow.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?