Teeth sensitivity, especially near the gum line or at the top of the tooth, is a common but often misunderstood condition. It can range from a mild twinge when drinking cold water to sharp, persistent pain that interferes with daily life. Unlike general toothaches, sensitivity at the top of the tooth—typically where the crown meets the gumline—is frequently linked to enamel loss, gum recession, or exposed dentin. Understanding the root causes and available treatments can help you regain comfort and protect your long-term oral health.
Understanding Tooth Anatomy and Sensitivity
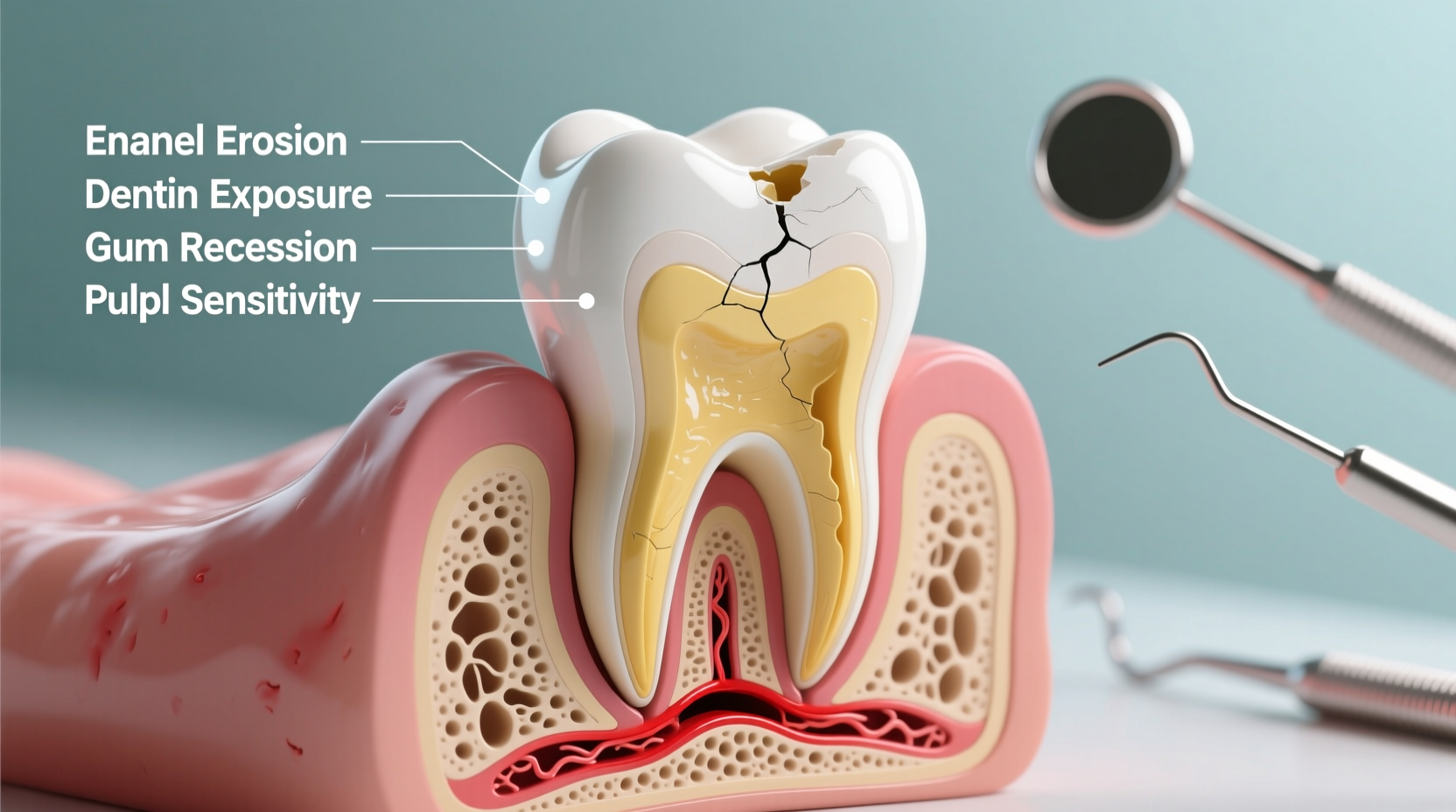
Tooth sensitivity occurs when the protective layers of the tooth are compromised. The outer layer, enamel, shields the crown. Beneath it lies dentin—a porous tissue containing microscopic tubules leading directly to the nerve. When enamel wears down or gums recede, these tubules become exposed, allowing external stimuli like hot, cold, sweet, or acidic substances to reach the nerve, triggering pain.
The \"top\" of the tooth—specifically the cervical area near the gumline—is particularly vulnerable. This region has thinner enamel and is more prone to wear from brushing, grinding, or acid erosion. Because this zone often lacks full enamel coverage, even minor damage can expose dentin quickly.
“Dentin exposure at the gumline is one of the most frequent causes of localized sensitivity. Early intervention prevents progression.” — Dr. Lena Torres, Clinical Dentist and Oral Health Researcher
Common Causes of Sensitivity at the Top of the Tooth
- Gum Recession: Periodontal disease, aggressive brushing, or aging can cause gums to pull back, exposing sensitive root surfaces.
- Enamel Erosion: Frequent consumption of acidic foods (citrus, soda, wine) softens enamel over time, making it easier to wear away.
- Tooth Grinding (Bruxism): Clenching or grinding, often during sleep, wears down enamel, especially at the neck of the tooth.
- Improper Brushing Technique: Using a hard-bristled brush or brushing too vigorously can abrade enamel and irritate gums.
- Dental Procedures: Whitening treatments, fillings, or professional cleanings may cause temporary sensitivity.
- Cracked Teeth or Leaky Fillings: Microfractures or worn restorations allow bacteria and temperature changes to penetrate deeper layers.
Effective Treatments and Professional Interventions
While over-the-counter remedies can offer relief, lasting solutions often require professional diagnosis and treatment. A dentist can identify whether sensitivity stems from structural damage, gum disease, or occlusal (bite) issues.
Professional Treatment Options
| Treatment | How It Works | Expected Outcome |
|---|---|---|
| Fluoride Varnish | Applied professionally to strengthen enamel and reduce dentin permeability | Reduced sensitivity within days; protection lasts several months |
| Bonding or Sealants | Resin applied to cover exposed root surfaces | Immediate protection and cosmetic improvement |
| Gum Graft Surgery | Tissue taken from palate or donor source to cover receded areas | Long-term solution for severe recession and root exposure |
| Mouthguard for Bruxism | Custom-fitted night guard prevents enamel wear | Preserves tooth structure and reduces jaw tension |
In-office desensitizing agents provide faster results than home products. For example, oxalate or resin-based sealers block dentinal tubules, reducing nerve stimulation. These are often applied after cleanings or as part of a sensitivity management plan.
Step-by-Step Guide to Managing Sensitivity at Home
Home care plays a crucial role in both treating and preventing sensitivity. Follow this timeline to manage symptoms effectively:
- Week 1: Identify Triggers – Keep a log of when pain occurs (e.g., after coffee, ice cream, brushing). Note location and intensity.
- Week 2: Switch to Sensitive Formula – Use a toothpaste with potassium nitrate or stannous fluoride twice daily. Avoid rinsing immediately after brushing to prolong contact.
- Week 3: Adjust Brushing Habits – Use gentle pressure and a 45-degree angle at the gumline. Replace your toothbrush every three months.
- Week 4: Limit Acidic Intake – Reduce consumption of citrus, carbonated drinks, and vinegar-based foods. Wait 30 minutes after eating before brushing.
- Ongoing: Schedule Dental Checkups – Visit your dentist every six months for early detection of erosion, decay, or gum issues.
“Patients who follow a structured sensitivity routine see up to 70% improvement within four weeks.” — American Dental Association, Patient Management Guidelines
Real-Life Example: Maria’s Experience with Gum Recession
Maria, a 38-year-old teacher, began noticing sharp pain when drinking cold tea. The discomfort was isolated to her upper front teeth, right at the gumline. After ruling out cavities, her dentist diagnosed moderate gum recession caused by years of aggressive brushing. She was using a hard-bristled brush and scrubbing vertically, which wore down enamel and pushed gums back.
Her treatment plan included switching to a soft electric toothbrush, applying prescription fluoride gel nightly, and wearing a custom mouthguard due to nighttime clenching. Within two months, her sensitivity decreased significantly. Six months later, a minor gum graft restored lost tissue and eliminated discomfort entirely.
Maria’s case highlights how multiple factors—brushing technique, bruxism, and delayed dental visits—can combine to create sensitivity. Addressing each element led to full recovery.
Do’s and Don’ts: Quick Reference Checklist
- ✅ Do: Use fluoride toothpaste designed for sensitivity
- ✅ Do: Brush with a soft-bristled brush using gentle circular motions
- ✅ Do: Rinse with alcohol-free, neutral-pH mouthwash
- ✅ Do: Wear a night guard if you grind your teeth
- ❌ Don’t: Brush immediately after consuming acidic foods
- ❌ Don’t: Use whitening toothpastes—they’re highly abrasive
- ❌ Don’t: Ignore persistent pain—it may signal deeper issues like decay or infection
Frequently Asked Questions
Can tooth sensitivity go away on its own?
Minor sensitivity caused by recent dental work or temporary gum irritation may resolve within a few days. However, chronic sensitivity due to enamel loss or gum recession won’t improve without intervention. Left untreated, it can worsen over time.
Is it normal for only one tooth to be sensitive?
Yes. Localized sensitivity often points to a specific issue such as a cracked tooth, deep cavity, or failed filling. It’s important to have isolated pain evaluated by a dentist to rule out serious conditions.
Are natural remedies effective for sensitive teeth?
Some people find temporary relief using clove oil or green tea rinses due to their anti-inflammatory properties. However, these lack clinical evidence for long-term efficacy. They should never replace professional care.
Take Control of Your Oral Comfort Today
Tooth sensitivity at the top of the tooth isn’t something you have to live with. Whether caused by everyday habits or underlying dental conditions, effective solutions exist. From adjusting your brushing technique to seeking professional treatments like fluoride therapy or gum grafts, proactive steps can restore comfort and prevent further damage.
Your smile is meant to feel good—not flinch at every sip of coffee. Start by evaluating your current routine, identifying potential causes, and scheduling a checkup with your dentist. Small changes today can lead to lasting relief tomorrow.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?