Varicose veins are more than a cosmetic concern—they are a visible sign of underlying circulatory problems. While many people dismiss them as harmless bulging veins on the legs, the reality is that untreated varicose veins can lead to serious medical complications. From chronic pain and skin ulcers to life-threatening blood clots, the risks associated with these damaged veins should not be ignored. Understanding why varicose veins are bad goes beyond aesthetics; it's about protecting your long-term vascular health.
The Hidden Dangers Behind Bulging Veins
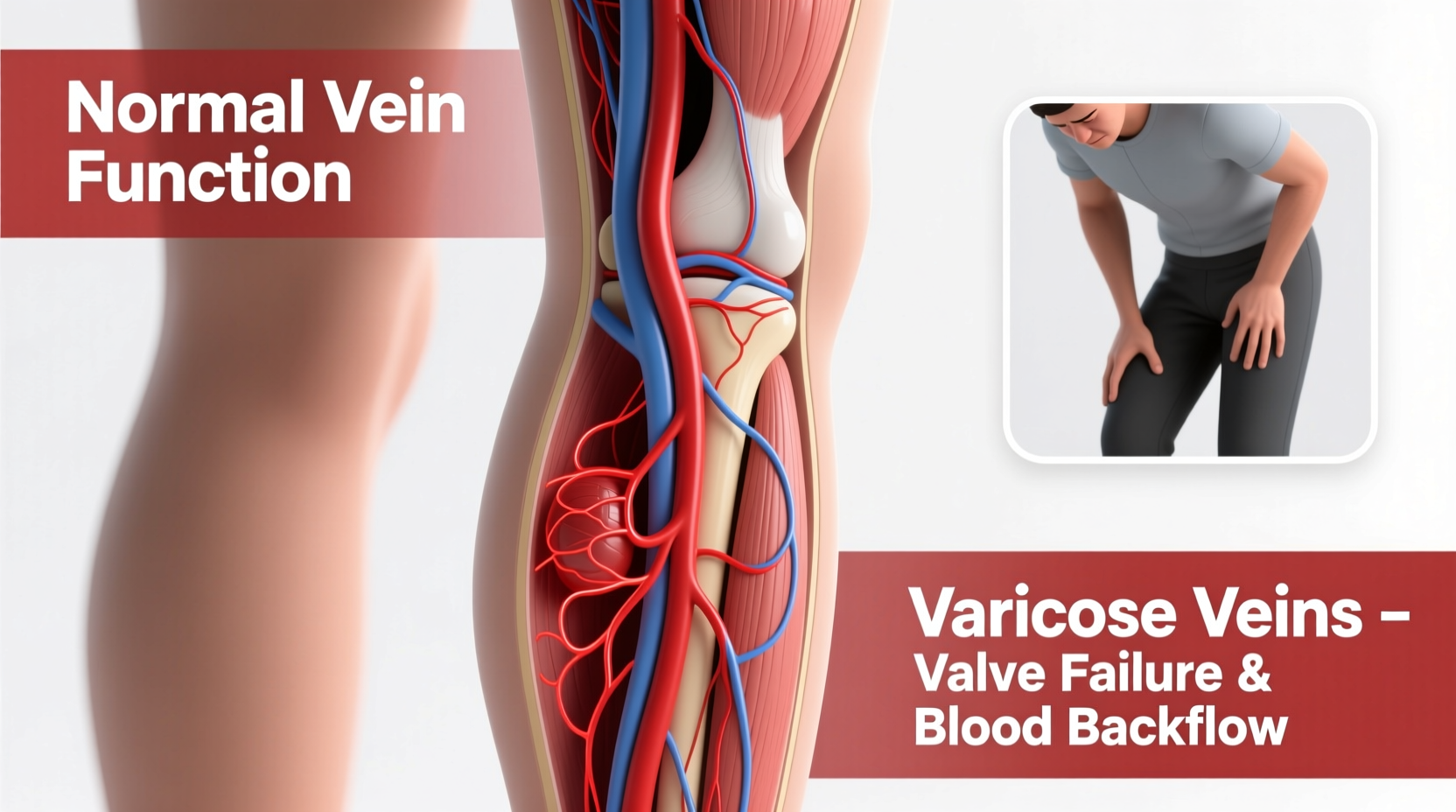
Varicose veins develop when the valves inside leg veins weaken or fail, allowing blood to flow backward and pool in the lower extremities. This pooling increases pressure in the veins, causing them to stretch, twist, and become visibly enlarged. Although they often appear just beneath the skin, their impact extends deeper into the circulatory system.
Over time, the increased venous pressure leads to tissue damage, inflammation, and reduced oxygen delivery to surrounding tissues. Left unchecked, this chronic condition—known as chronic venous insufficiency (CVI)—can progress to stages that significantly impair mobility and quality of life.
Common Health Risks of Untreated Varicose Veins
Many patients delay treatment because they assume varicose veins are only a visual issue. However, research shows that up to 30% of individuals with varicose veins will experience progressive symptoms without medical care. Below are some of the most significant health risks:
- Chronic Leg Pain and Heaviness: Persistent aching, throbbing, or cramping in the legs, especially after prolonged standing or sitting.
- Swelling (Edema): Fluid accumulation in the ankles and lower legs due to poor circulation.
- Skin Changes: Discoloration (often brownish staining), dryness, and thickening around affected veins—early signs of venous stasis dermatitis.
- Superficial Thrombophlebitis: Inflammation of a surface vein caused by a blood clot, leading to redness, warmth, and tenderness along the vein path.
- Bleeding from Thin Skin: Enlarged veins close to the skin surface can rupture with minor trauma, causing sudden and sometimes heavy bleeding.
- Deep Vein Thrombosis (DVT): Although less common, varicose veins increase the risk of DVT—a potentially fatal condition where a clot forms in a deep vein and may travel to the lungs (pulmonary embolism).
- Venous Ulcers: Open sores near the ankle that are difficult to heal, prone to infection, and often recur without addressing the root venous problem.
“Varicose veins are not just cosmetic. They represent abnormal blood flow and elevated venous pressure, which over time damages both skin and underlying tissues.” — Dr. Alan Pierce, Vascular Medicine Specialist
When Varicose Veins Turn Serious: A Real-Life Example
Maria, a 54-year-old schoolteacher from Ohio, first noticed twisted blue veins on her calves ten years ago. She dismissed them as a normal part of aging. Over time, her legs began to feel heavy by midday, and she developed persistent itching around her ankles. She attributed the swelling to “standing too much” and wore compression socks occasionally.
Five years later, a small wound near her ankle failed to heal. Within months, it expanded into a painful ulcer covered with darkened, hardened skin. Diagnosed with advanced venous insufficiency, Maria required endovenous laser treatment (EVLT) to close the malfunctioning saphenous vein, followed by months of wound care.
Her case illustrates how delaying treatment transforms manageable symptoms into debilitating conditions. Today, Maria walks without pain—but emphasizes that early diagnosis could have spared her two years of discomfort and medical intervention.
Do’s and Don’ts: Managing Varicose Vein Risks
| Do | Don't |
|---|---|
| Elevate your legs above heart level for 15–20 minutes several times a day | Stand or sit for hours without moving |
| Wear medical-grade compression stockings as prescribed | Rely solely on fashion support hose |
| Exercise regularly—walking and swimming improve calf muscle pump function | Ignore new symptoms like swelling, discoloration, or skin changes |
| Seek evaluation from a board-certified vascular specialist | Assume all vein clinics offer the same standard of care |
| Maintain a healthy weight to reduce pressure on leg veins | Smoke—nicotine damages blood vessels and impairs circulation |
Step-by-Step Guide to Reducing Long-Term Risks
Preventing complications starts with proactive management. Follow this timeline-based approach to protect your vascular health:
- Week 1: Self-Assessment
Check your legs for visible veins, swelling, or skin texture changes. Note any discomfort patterns (e.g., worse at night). - Week 2: Schedule a Vascular Screening
Visit a vein specialist for a duplex ultrasound to assess valve function and blood flow. - Month 1: Begin Conservative Care
Start wearing Class II compression stockings during waking hours and incorporate daily walking (30 minutes). - Month 2–3: Evaluate Treatment Options
If diagnosed with venous insufficiency, discuss minimally invasive treatments such as sclerotherapy, radiofrequency ablation, or EVLT. - Ongoing: Lifestyle Integration
Maintain activity, avoid prolonged immobility, elevate legs routinely, and monitor skin condition closely.
Frequently Asked Questions
Can varicose veins cause blood clots?
Yes. While superficial clots (thrombophlebitis) are more common, people with varicose veins have a higher risk of developing deep vein thrombosis (DVT), particularly if they’re sedentary, obese, or have a history of clotting disorders. Any sudden leg swelling, redness, or warmth requires immediate medical attention.
Are spider veins the same as varicose veins?
No. Spider veins are smaller, red or purple clusters near the skin surface and usually don’t cause significant symptoms. However, they can indicate early venous dysfunction. In contrast, varicose veins are larger, rope-like, and often signal underlying valve failure requiring evaluation.
Is surgery the only option for treatment?
No. Most modern treatments are minimally invasive and performed in-office under local anesthesia. Procedures like endovenous thermal ablation or foam sclerotherapy close faulty veins without surgery, with minimal downtime and high success rates.
Conclusion: Take Your Vein Health Seriously
Dismissing varicose veins as a cosmetic flaw ignores their role as warning signs of deeper vascular issues. The consequences of inaction—chronic pain, skin breakdown, ulcers, and even dangerous clots—are entirely preventable with timely care. Modern diagnostics and treatments make managing varicose veins safer, easier, and more effective than ever before.
Your legs carry you through life. Protecting their health isn’t vanity—it’s necessity. If you notice bulging veins, persistent aching, or skin changes, don’t wait for complications to arise. Seek expert evaluation today and take control of your circulatory well-being.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?