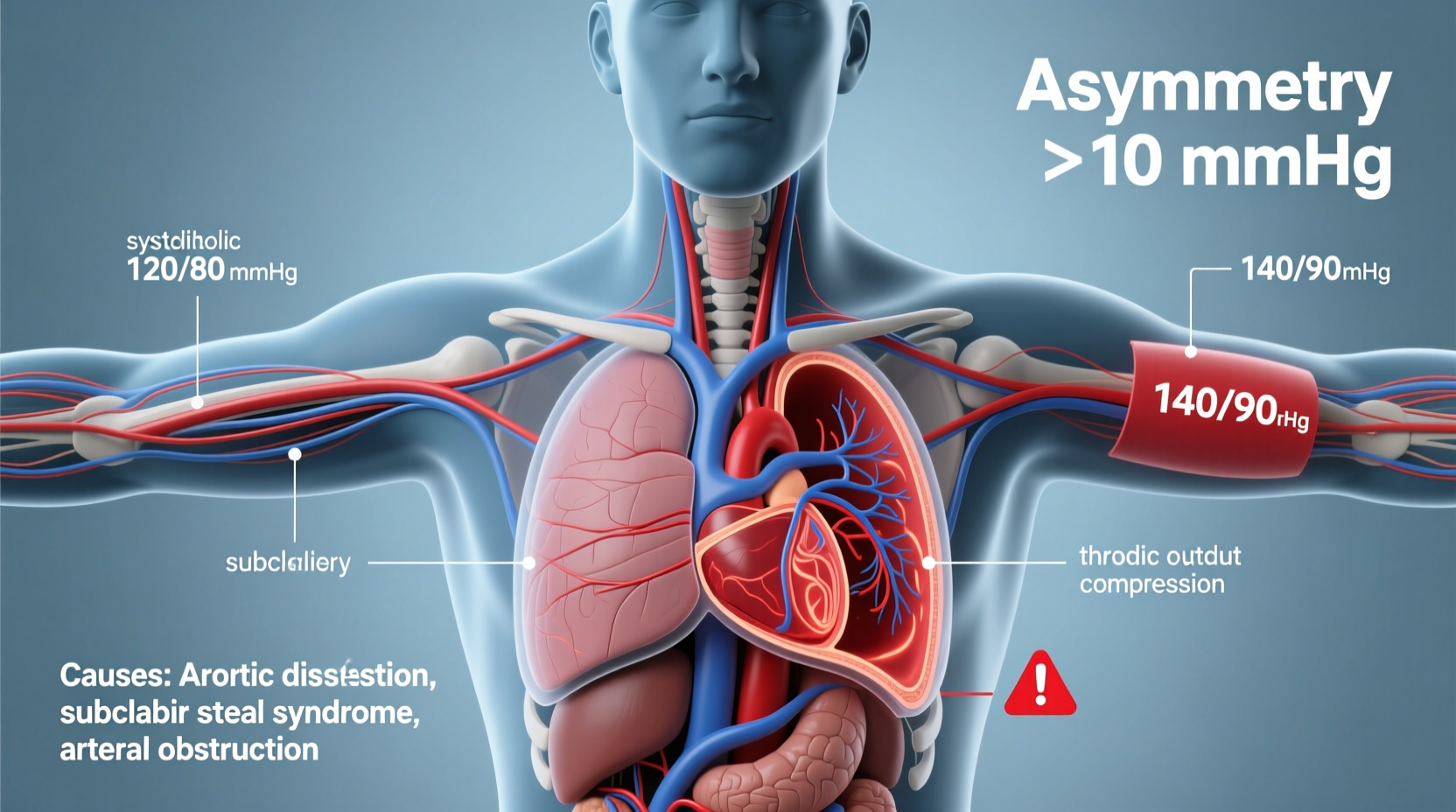
A small variation in blood pressure readings between your left and right arms is normal. However, a consistent and significant difference—typically 10 mm Hg or more in systolic pressure—can signal underlying health issues. While many people overlook this discrepancy during home monitoring or routine checkups, it can be an early warning sign of vascular disease, heart problems, or other serious conditions. Understanding why this occurs and knowing when to act can make a critical difference in long-term cardiovascular health.
Understanding Normal vs. Abnormal Differences
Blood pressure naturally fluctuates throughout the day due to activity, stress, posture, and even which arm is used for measurement. A difference of up to 5–10 mm Hg in systolic pressure (the top number) between arms is considered within the normal range. This minor asymmetry results from anatomical differences in the branching of arteries from the aorta.
However, when the gap consistently exceeds 10 mm Hg, especially in systolic pressure, it may indicate restricted blood flow in one arm’s arteries. A difference of 15 mm Hg or more is clinically significant and warrants medical evaluation. Diastolic differences (the bottom number) are less commonly concerning unless they exceed 10 mm Hg and are accompanied by other symptoms.
Common Causes of Significant Blood Pressure Differences
Several medical conditions can lead to a notable disparity in blood pressure readings between arms. These range from structural abnormalities to progressive vascular diseases.
- Peripheral Artery Disease (PAD): Narrowing or blockage of arteries—often due to atherosclerosis—can reduce blood flow to one arm, resulting in lower pressure on that side.
- Subclavian Artery Stenosis: A narrowing of the subclavian artery, which supplies blood to the arms, can cause reduced pressure in the affected arm. This condition may also trigger “subclavian steal syndrome,” where blood flow reverses in the vertebral artery during exercise.
- Takayasu’s Arteritis: A rare inflammatory disease affecting large arteries, including the aorta and its branches. It often leads to diminished pulses and blood pressure in one arm.
- Congenital Heart Defects: Some individuals are born with structural anomalies such as coarctation of the aorta, which can result in unequal blood distribution.
- Thoracic Outlet Syndrome: Compression of nerves and blood vessels between the collarbone and first rib may impair circulation and alter pressure readings.
- Previous Surgery or Trauma: Damage to major arteries from injury or surgical procedures (e.g., bypass grafts) can affect blood flow dynamics.
“Measuring blood pressure in both arms is a simple, non-invasive way to detect potential vascular disease early. A difference of 10 mm Hg or more should prompt further investigation.” — Dr. Richard Nair, Vascular Medicine Specialist
When to Seek Medical Attention
Not every variation requires immediate concern, but certain patterns demand professional follow-up. You should consult a healthcare provider if:
- You consistently observe a systolic difference of 10 mm Hg or more across multiple readings taken on different days.
- The arm with lower pressure feels colder, weaker, or has a faint or absent pulse.
- You experience dizziness, arm fatigue during activity, chest pain, or shortness of breath—especially during exertion.
- You have risk factors such as smoking, diabetes, high cholesterol, or a history of heart disease.
In clinical settings, doctors often use Doppler ultrasound, CT angiography, or MRI to evaluate arterial structure and identify blockages. Early diagnosis of conditions like subclavian stenosis can prevent complications such as stroke, claudication, or limb ischemia.
Step-by-Step Guide to Monitoring Blood Pressure at Home
Accurate self-monitoring helps detect discrepancies early. Follow this protocol for reliable results:
- Rest for 5 minutes before measuring. Sit quietly with your back supported and feet flat on the floor.
- Use the same validated upper-arm monitor for all readings. Wrist devices are less accurate and not recommended for detecting inter-arm differences.
- Take the first reading on your right arm. Record both systolic and diastolic values.
- Wait 1–2 minutes, then repeat on the left arm using the same position and cuff placement.
- Repeat the process twice more over the next few days to confirm consistency.
- Note the higher reading as your reference value for future checks—and always use that arm unless instructed otherwise.
- Contact your doctor if the systolic difference is ≥10 mm Hg on two separate occasions.
| Reading Difference (Systolic) | Interpretation | Action Required |
|---|---|---|
| < 5 mm Hg | Normal variation | None – continue routine monitoring |
| 5–9 mm Hg | Mild difference | Monitor over time; recheck weekly |
| ≥10 mm Hg | Potentially significant | Consult physician; consider vascular screening |
| ≥15 mm Hg | Clinically concerning | Seek evaluation within 1–2 weeks |
Mini Case Study: Detecting Subclavian Stenosis Early
John, a 58-year-old office worker with a history of hypertension and smoking, began monitoring his blood pressure at home after a routine checkup. Over three consecutive mornings, he noticed his left arm registered 138/82 mm Hg, while his right read 152/86 mm Hg—a 14-point systolic gap. Concerned, he brought this to his doctor’s attention.
Further examination revealed a weak radial pulse in the left arm. A Doppler ultrasound showed moderate stenosis in the left subclavian artery. With timely intervention—including medication adjustment and lifestyle changes—John avoided surgical intervention and stabilized his condition. His case underscores how routine bilateral measurements can uncover silent but serious vascular issues.
Frequently Asked Questions
Is it normal for blood pressure to be higher in one arm?
Yes, slight differences are normal. Most people have a dominant arm with marginally higher pressure due to greater muscle mass and usage. The key concern arises when the difference is consistently 10 mm Hg or more in systolic pressure.
Which arm should I use to measure blood pressure?
Initially, measure both arms. Use the arm with the higher reading for future monitoring, as guidelines recommend basing treatment decisions on the higher value. If there's no consistent difference, either arm is acceptable—just remain consistent.
Can anxiety cause different readings between arms?
Anxiety may elevate overall blood pressure, but it typically affects both arms equally. It’s unlikely to create a sustained inter-arm difference. True discrepancies are more likely due to structural or vascular factors rather than emotional state.
Prevention and Long-Term Management
While some causes of inter-arm differences are congenital or inflammatory, many stem from modifiable risk factors. Maintaining cardiovascular health reduces the likelihood of developing arterial disease:
- Control blood pressure, cholesterol, and blood sugar levels.
- Avoid tobacco use, which accelerates arterial damage.
- Exercise regularly to promote healthy circulation.
- Eat a balanced diet rich in fruits, vegetables, whole grains, and lean proteins.
- Schedule regular physical exams, especially if you're over 40 or have a family history of heart disease.
Conclusion: Take Discrepancies Seriously
A difference in blood pressure between arms may seem trivial, but it can be a vital clue to hidden cardiovascular disease. Ignoring consistent disparities could mean missing an opportunity to prevent serious complications like stroke, heart attack, or peripheral ischemia. By adopting a disciplined approach to monitoring and understanding when to seek help, you empower yourself with knowledge that supports long-term heart health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?