Body Mass Index (BMI) has long been a go-to tool in healthcare for quickly assessing whether someone is underweight, normal weight, overweight, or obese. It’s simple: divide your weight in kilograms by your height in meters squared. But while BMI offers a convenient snapshot, it falls short in capturing the full picture of an individual’s health. Relying solely on this number can lead to misclassification, unnecessary anxiety, or even missed diagnoses. Understanding why BMI isn’t perfect is essential for making informed decisions about personal health and interpreting medical advice.
What BMI Measures — And What It Doesn’t
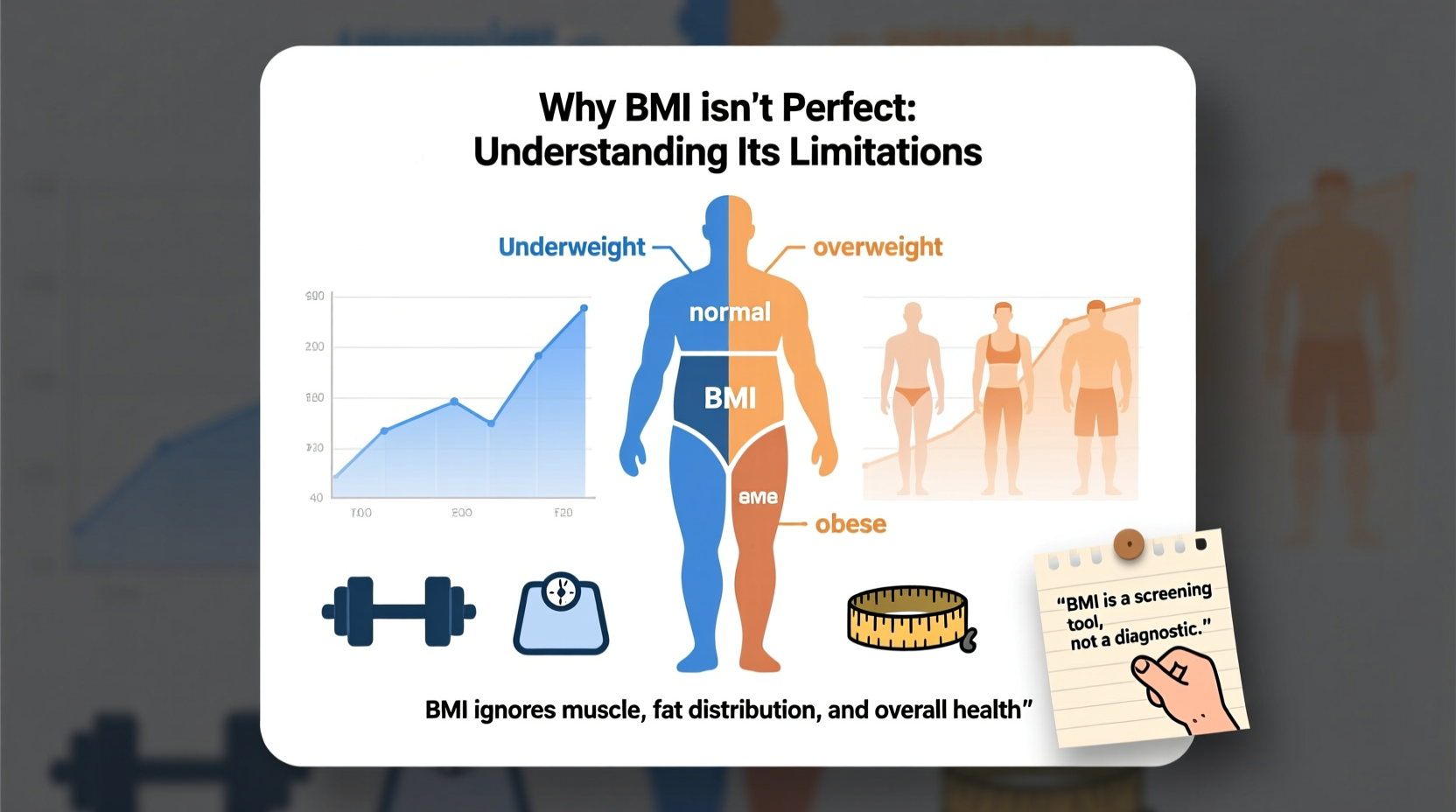
BMI was developed in the 19th century by Belgian mathematician Adolphe Quetelet as a statistical tool to study populations, not individuals. It correlates weight with height to estimate body fat at a population level. While useful for identifying trends across large groups, it doesn’t differentiate between muscle, fat, bone density, or water weight.
A professional athlete with high muscle mass may have a BMI in the “overweight” or even “obese” range, despite having low body fat and excellent cardiovascular health. Conversely, someone with a “normal” BMI might carry excess visceral fat — the kind surrounding internal organs — which increases risk for heart disease and diabetes, yet remain undetected by BMI alone.
Key Limitations of BMI
The flaws in using BMI as a universal health metric stem from several critical oversights:
- Ignores body composition: Muscle weighs more than fat, so muscular individuals are often misclassified as overweight.
- Doesn’t account for fat distribution: Abdominal fat (central obesity) is a stronger predictor of disease risk than overall weight.
- Fails across demographics: BMI thresholds don’t adjust for age, sex, ethnicity, or frame size, leading to inaccuracies.
- Overlooks metabolic health: A person with normal weight but poor diet and sedentary lifestyle may still face high health risks.
- Can perpetuate weight stigma: Labeling someone “obese” based on BMI alone may discourage them from seeking care due to shame or bias.
“BMI is a starting point, not a diagnosis. We need to look beyond the number to understand true health.” — Dr. Fatima Cody Stanford, Obesity Medicine Physician at Harvard Medical School
How Ethnicity and Age Affect BMI Accuracy
Research shows that different ethnic groups have varying relationships between BMI and health risk. For example, South Asian populations tend to have higher body fat percentages at lower BMIs compared to White populations, increasing their risk for type 2 diabetes and cardiovascular disease even within the “normal” range.
Similarly, older adults often experience sarcopenia — loss of muscle mass — which can result in a stable or declining BMI while body fat increases. This shift may mask deteriorating metabolic health. Children and adolescents present another challenge; BMI must be interpreted using age- and sex-specific growth charts, adding complexity to its use.
| Population Group | BMI Interpretation Issue | Recommended Adjustment |
|---|---|---|
| South Asians | Higher risk at lower BMI | Use lower thresholds (e.g., ≥23 for overweight) |
| Black Americans | May have more lean mass | Combine with waist circumference |
| Elderly (>65) | Loss of muscle skews results | Assess strength, mobility, and nutrition |
| Athletes | High muscle mass inflates BMI | Use DEXA scans or body fat testing |
Real-World Example: The Misclassified Athlete
Consider Marcus, a 28-year-old firefighter who stands 5'10\" and weighs 210 pounds. His BMI calculates to 30.1 — placing him in the “obese” category. Despite rigorous physical training, healthy eating, and excellent bloodwork, his annual physical flags him for weight-related counseling. No one measures his body fat percentage (which is 14%) or considers his job’s physical demands.
This misclassification leads to frustration and undermines trust in his healthcare provider. Worse, it diverts attention from more meaningful health indicators like HDL cholesterol, resting heart rate, and aerobic capacity. Marcus’s case illustrates how rigid reliance on BMI can do more harm than good when applied without context.
Better Alternatives and Complementary Tools
To get a fuller picture of health, professionals increasingly recommend combining BMI with other assessments:
- Waist Circumference: A measurement above 35 inches for women or 40 inches for men indicates increased risk for metabolic syndrome.
- Waist-to-Hip Ratio: Compares waist size to hip size; values above 0.85 (women) and 0.90 (men) suggest central adiposity.
- Bioelectrical Impedance Analysis (BIA): Estimates body fat percentage using a small electrical current.
- Dual-Energy X-ray Absorptiometry (DEXA): Gold standard for measuring bone density, muscle mass, and fat distribution.
- Blood Biomarkers: Fasting glucose, triglycerides, HDL cholesterol, and HbA1c provide insight into metabolic function regardless of weight.
Checklist: Moving Beyond BMI
Use this checklist to assess your health more holistically:
- ✅ Measure your waist circumference annually
- ✅ Review blood pressure, lipid panel, and glucose levels with your doctor
- ✅ Track physical activity levels (aim for 150+ minutes of moderate exercise weekly)
- ✅ Evaluate diet quality — focus on whole foods, fiber, and balanced macronutrients
- ✅ Consider body composition testing if you're athletic or concerned about muscle-fat ratio
- ✅ Discuss mental well-being and sleep patterns — both impact metabolic health
Frequently Asked Questions
Is BMI completely useless?
No. For large-scale public health studies and initial screenings, BMI remains a practical and cost-effective tool. However, it should never be used in isolation to make clinical judgments about an individual’s health.
Can someone be “fat and fit”?
Yes. Research shows that individuals classified as overweight or mildly obese can have normal blood pressure, cholesterol, and insulin sensitivity — especially if they are physically active. Fitness level is often a stronger predictor of longevity than BMI alone.
Should I stop using BMI altogether?
You don’t need to discard it entirely, but treat it as one data point among many. Pair it with functional measures like energy levels, stamina, lab results, and body measurements for a more accurate assessment.
Toward a More Nuanced Approach to Health
The persistence of BMI in modern medicine reflects a desire for simplicity — but health is inherently complex. Reducing it to a single number ignores genetic diversity, lifestyle behaviors, socioeconomic factors, and psychological well-being. A growing movement known as “Health at Every Size” (HAES) advocates for focusing on sustainable habits rather than weight-centric goals, emphasizing respect, inclusivity, and evidence-based care.
Rather than fixating on whether your BMI falls into a “healthy” range, ask better questions: Are you strong enough to carry groceries up stairs? Do you feel energized during the day? Are your lab values improving? These indicators offer richer insights than any scale-derived formula.
“We must shift from weight-based judgments to function-based evaluations. Health isn’t a number — it’s how you live.” — Dr. Linda Bacon, Author of *Health at Every Size*
Take Action Today
Challenge the assumption that BMI tells the whole story. Talk to your healthcare provider about incorporating additional metrics into your checkups. Advocate for yourself by asking for body composition analysis or metabolic panels if you’re concerned. Most importantly, focus on building sustainable habits — nutritious eating, regular movement, quality sleep, and stress management — that support lifelong wellness, regardless of what the scale says.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?