Sudden difficulty or inability to cough may seem like a minor issue at first, but it can signal underlying health problems that require attention. Coughing is a protective reflex designed to clear the airways of mucus, irritants, and foreign particles. When this reflex is impaired—whether due to neurological issues, muscle weakness, or medication side effects—it increases the risk of respiratory complications, including infections and breathing difficulties. Understanding why you might not be able to cough effectively is essential for timely intervention and prevention of more serious conditions.
Understanding the Cough Reflex
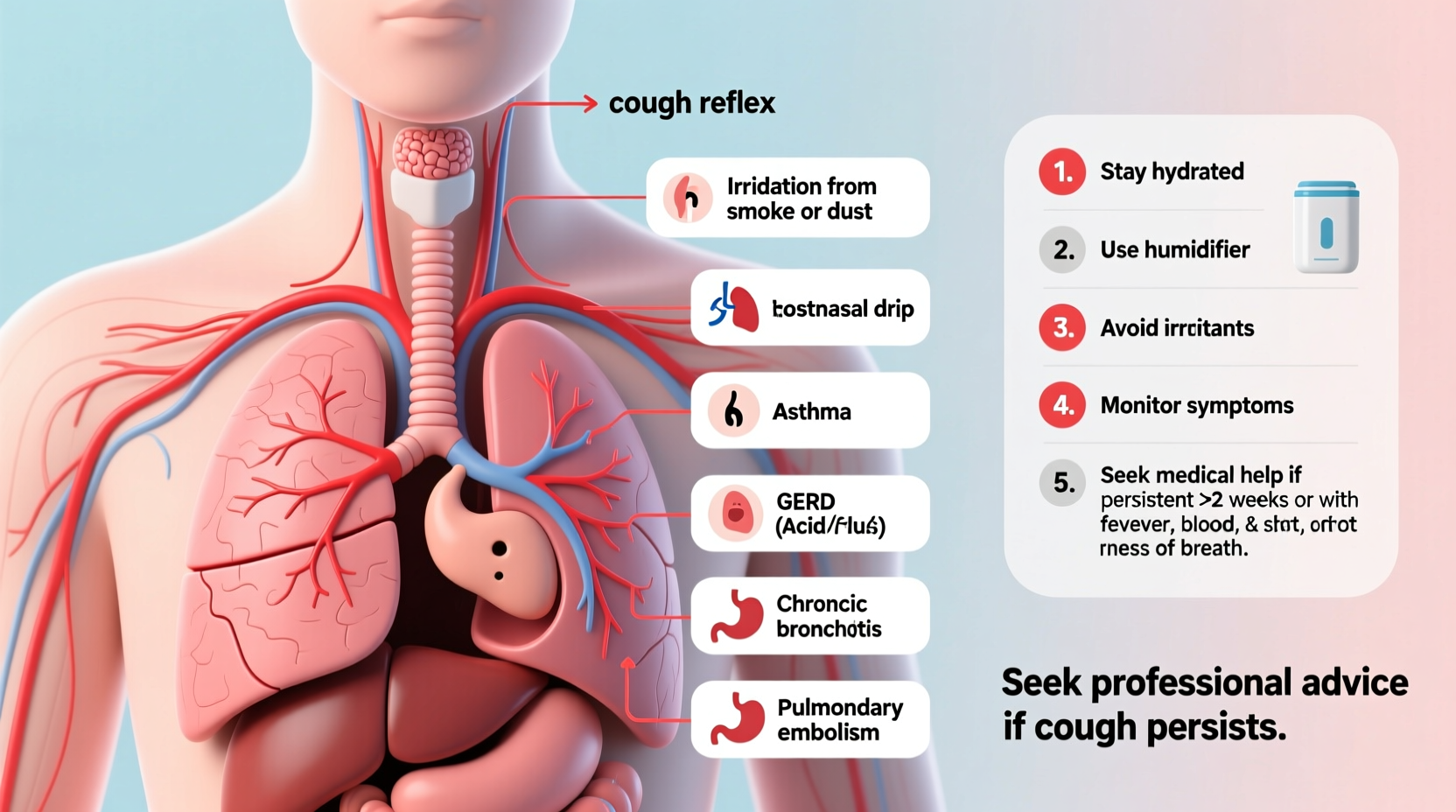
The cough reflex is a complex physiological process involving sensory nerves in the airways, the brainstem, and coordinated muscle contractions in the chest, abdomen, and diaphragm. When irritants such as dust, smoke, or excess mucus stimulate nerve endings in the trachea or bronchi, signals are sent to the medulla oblongata in the brain. This triggers a sequence: inhalation, closure of the glottis, buildup of pressure in the lungs, and forceful expulsion of air to dislodge the irritant.
Any disruption along this pathway—neural, muscular, or structural—can impair your ability to initiate or sustain an effective cough. A weak or absent cough does not always mean illness; sometimes, it reflects fatigue, dehydration, or even psychological factors. However, persistent suppression should never be ignored.
Possible Causes of Inability to Cough
Several medical and environmental factors can interfere with the cough mechanism. These range from temporary conditions to chronic diseases affecting the nervous or muscular systems.
Neurological Disorders
Diseases that affect nerve signaling can disrupt the brain’s ability to trigger a cough. Conditions such as Parkinson’s disease, multiple sclerosis (MS), amyotrophic lateral sclerosis (ALS), and stroke may damage the neural pathways responsible for the reflex. Brainstem injuries or tumors can also directly impair the cough center.
Muscle Weakness or Paralysis
Coughing requires strength in the diaphragm, intercostal muscles, and abdominal wall. Patients recovering from prolonged bed rest, neuromuscular disorders like myasthenia gravis, or those on mechanical ventilation often experience reduced cough efficacy. Spinal cord injuries above T6 can similarly compromise abdominal muscle engagement needed for forceful expulsion.
Medication Side Effects
Some medications suppress the cough reflex intentionally or unintentionally. Opioids (e.g., morphine, codeine) act on central nervous system receptors and reduce both the sensation of irritation and the motor response. Certain sedatives, antipsychotics, and muscle relaxants may also dull reflexes. Overuse of over-the-counter cough suppressants containing dextromethorphan can lead to diminished responsiveness over time.
Dehydration and Thickened Mucus
When the body lacks sufficient fluids, mucus becomes thick and sticky, making it harder to expel—even if the cough reflex is intact. Dehydration reduces mucosal lubrication in the airways, which can make the urge to cough less noticeable and less productive.
Post-Surgical or Anesthetic Effects
General anesthesia temporarily depresses many reflexes, including coughing. After surgery, especially procedures involving the chest or abdomen, patients may struggle to cough due to pain, residual anesthetic effects, or fear of incision strain. This is particularly dangerous because it raises the risk of postoperative pneumonia.
“An ineffective cough is one of the most underrecognized risks in respiratory care. It can silently lead to retained secretions and life-threatening infections.” — Dr. Lena Patel, Pulmonologist at Boston Respiratory Institute
What to Do If You Can’t Cough Effectively
If you notice a sudden or progressive decline in your ability to cough, especially when accompanied by congestion, shortness of breath, or fatigue, take immediate action. Here’s a step-by-step guide to assess and address the issue:
- Evaluate Symptoms: Note whether you feel mucus buildup, have a dry throat, experience shortness of breath, or feel fatigued. Also consider recent illnesses, surgeries, or new medications.
- Stay Hydrated: Drink warm fluids like herbal teas or broths to thin mucus and stimulate airway clearance.
- Practice Huff Coughing: Take a deep breath, then forcefully exhale in three quick “huffs” while keeping your mouth open. This technique helps move mucus upward without requiring a strong traditional cough.
- Use Assisted Techniques: Ask someone to apply gentle pressure to your abdomen during exhalation (if safe and comfortable) to boost expiratory force.
- Avoid Irritants: Stay away from smoke, strong perfumes, and cold dry air, which can further inflame already compromised airways.
- Seek Medical Evaluation: If symptoms persist beyond 48 hours or worsen, consult a healthcare provider. Diagnostic tools like spirometry, chest X-rays, or laryngoscopy may be necessary.
Tips for Improving Cough Function
- Use a humidifier in dry environments to keep airways moist.
- Perform daily breathing exercises such as diaphragmatic breathing to strengthen respiratory muscles.
- Consider pulmonary rehabilitation if you have a chronic lung or neuromuscular condition.
- Avoid suppressing natural coughs unless medically advised—your body uses them for protection.
- Review all medications with your doctor to identify potential suppressants.
Do’s and Don’ts When Experiencing Impaired Cough
| Do’s | Don’ts |
|---|---|
| Drink plenty of water and warm liquids | Ignore signs of mucus retention or wheezing |
| Try huff coughing techniques | Smoke or expose yourself to secondhand smoke |
| Use prescribed inhalers or nebulizers if applicable | Take opioid painkillers without discussing alternatives with your doctor |
| Seek evaluation after surgery if coughing is painful or impossible | Assume it's just a cold and will pass on its own |
Frequently Asked Questions
Can anxiety stop me from coughing?
While anxiety doesn’t typically block the physical cough reflex, it can alter your awareness of bodily sensations. Some people report feeling unable to initiate a cough during panic episodes due to hyperventilation or muscle tension. However, true reflex suppression is rare in anxiety alone.
Is it dangerous to not be able to cough?
Yes. An ineffective cough increases the risk of aspiration, pneumonia, and respiratory failure, especially in older adults or those with preexisting lung conditions. Retained secretions create a breeding ground for bacteria and can obstruct airways.
Can vocal cord dysfunction cause cough problems?
Absolutely. Vocal cord dysfunction (VCD), also known as paradoxical vocal fold motion, involves abnormal closure of the vocal cords during inhalation or exhalation. While it often causes breathing difficulties, it can also interfere with the coordination needed for effective coughing.
Real-Life Example: Recovering After Surgery
James, a 67-year-old recovering from abdominal surgery, noticed he couldn’t cough despite feeling mucus in his chest. Fearing pain at his incision site, he avoided deep breaths and suppressed any urge to cough. Within three days, he developed a low-grade fever and increasing shortness of breath. His nurse recognized early signs of atelectasis—partial lung collapse due to mucus blockage—and initiated incentive spirometry, hydration, and assisted huffing techniques. With prompt care, James avoided pneumonia and regained effective airway clearance within a week.
This case highlights how post-surgical patients are especially vulnerable when cough mechanisms fail. Proactive management is key.
Action Checklist: Responding to Cough Difficulties
- Monitor for symptoms: mucus buildup, fatigue, shallow breathing
- Increase fluid intake throughout the day
- Practice huff coughing every few hours if secretions are present
- Use a humidifier, especially at night
- Review current medications with a physician
- Contact a healthcare provider if no improvement in 2–3 days
- Seek emergency care if experiencing confusion, cyanosis (blue lips), or severe breathlessness
Conclusion
Your ability to cough is more than just a reflex—it’s a vital defense mechanism for respiratory health. Whether weakened by illness, medication, or physical limitation, a compromised cough demands attention. By recognizing the warning signs, applying supportive strategies, and seeking timely medical input, you can protect your lungs and maintain better overall well-being. Don’t wait until symptoms escalate. Listen to your body, take proactive steps, and prioritize respiratory resilience.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?