Many men experience moments when they struggle to achieve or maintain a full erection. While occasional difficulty is normal, persistent issues can signal underlying health concerns or emotional stress. Erectile dysfunction (ED) is more than a bedroom problem—it’s often an early warning sign of cardiovascular disease, hormonal imbalance, or mental health challenges. Understanding why this happens is the first step toward effective solutions.
The Physiology of Erection: What Needs to Work
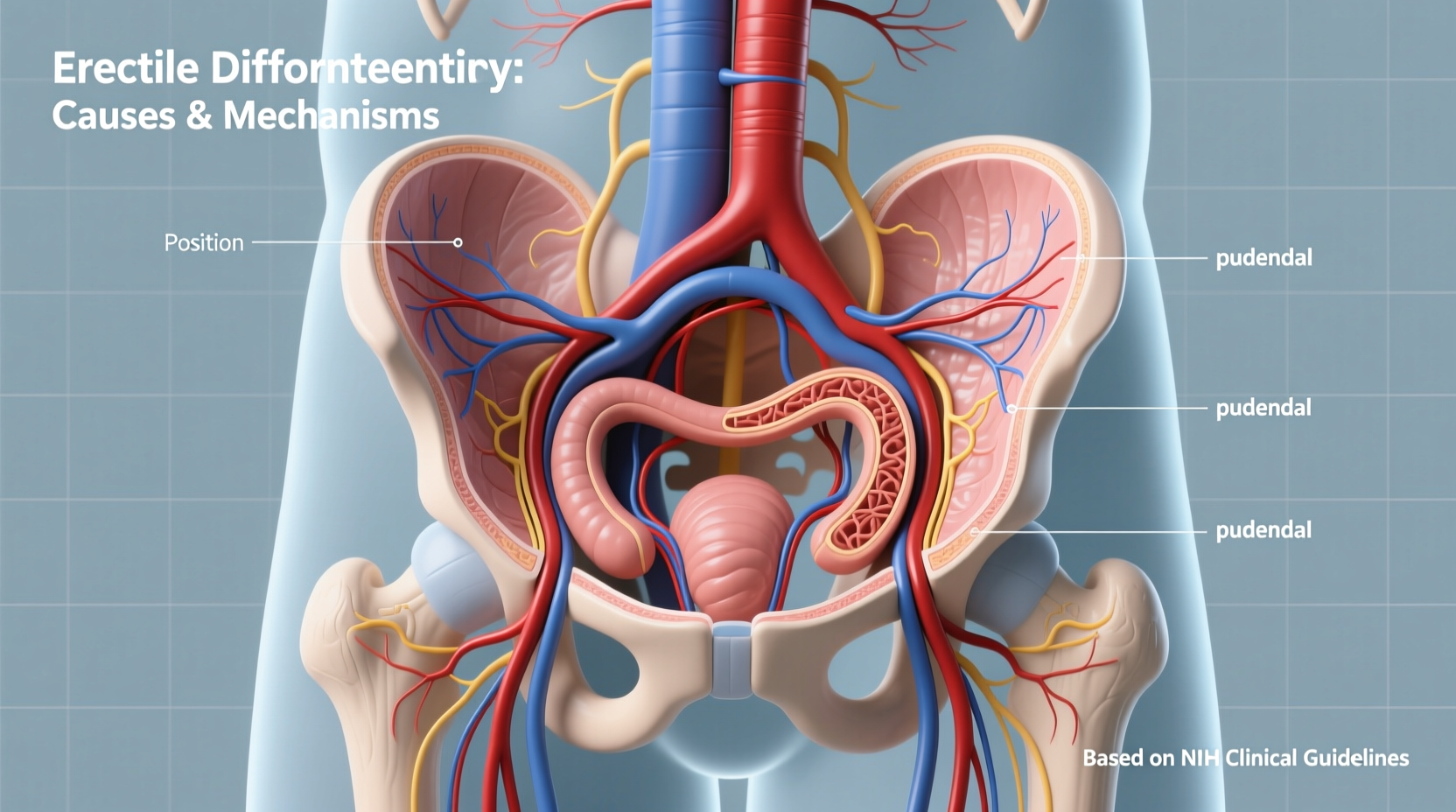
An erection isn’t just about arousal—it’s a complex process involving the brain, hormones, blood vessels, nerves, and muscles. When sexually stimulated, the brain sends signals through the nervous system to the penile tissue. Blood flows into the spongy chambers of the penis (corpora cavernosa), causing expansion and rigidity. For a full, sustainable erection, this vascular response must be strong and uninterrupted.
If any part of this chain fails—whether due to poor circulation, nerve damage, low testosterone, or psychological interference—the result may be incomplete or fleeting erections. It’s not always about desire; sometimes, the body simply can’t respond even when the mind is engaged.
“Erectile function is a window into overall cardiovascular health. When blood can’t flow properly here, it often means problems elsewhere.” — Dr. Alan Rosen, Urologist and Men’s Health Specialist
Common Physical Causes of Incomplete Erections
More than half of ED cases are rooted in physical conditions that impair blood flow or nerve signaling. These include:
- Cardiovascular disease: Atherosclerosis (narrowed arteries) reduces blood flow to the penis.
- Diabetes: High blood sugar damages nerves and blood vessels over time.
- Low testosterone: Hormonal deficiency can reduce libido and hinder erectile quality.
- Hypertension and medications: Blood pressure drugs, especially beta-blockers, may interfere with erectile function.
- Obesity and metabolic syndrome: Excess fat contributes to inflammation and insulin resistance, both linked to ED.
- Smoking and alcohol abuse: Both constrict blood vessels and impair nerve responses.
Psychological Factors That Disrupt Performance
Mental health plays a powerful role in sexual function. Anxiety, depression, stress, and relationship conflicts can all disrupt the brain’s ability to initiate or sustain an erection. Performance anxiety is especially common: the fear of failing in bed creates a self-fulfilling cycle of stress and dysfunction.
Men who perform well during masturbation but struggle with partners often point to psychological roots. The presence of a partner introduces pressure, self-consciousness, or unresolved emotional tension that wasn’t there alone.
Other contributing factors include:
- Work-related stress affecting focus and relaxation
- Past traumatic sexual experiences
- Unrealistic expectations from porn or societal norms
- Lack of emotional intimacy in a relationship
Mini Case Study: Mark’s Experience
Mark, a 47-year-old accountant, began noticing he couldn’t get fully hard during sex with his wife. At first, he blamed fatigue. But when the issue persisted for months, he consulted a urologist. Tests revealed mild hypertension and borderline prediabetes—conditions he hadn’t known about. After starting lifestyle changes and medication for blood pressure, his erectile function improved significantly within 12 weeks. “I thought it was stress,” he said. “Turns out, my body was trying to tell me something important.”
Medications and Lifestyle: What Helps and What Hurts
Certain prescriptions and daily habits can either support or sabotage erectile health. Below is a comparison of common influences:
| Influence | Positive Impact | Negative Impact |
|---|---|---|
| Exercise (especially cardio) | Improves blood flow, boosts testosterone | None when done moderately |
| Smoking | None | Narrows blood vessels, reduces oxygen delivery |
| Alcohol (moderate vs. heavy) | Slight relaxation at low doses | Depresses nervous system, impairs arousal |
| Phosphodiesterase inhibitors (e.g., Viagra) | Enhances blood flow to the penis | Risk of side effects; not suitable for heart patients |
| Sleep quality | Supports hormone balance and recovery | Poor sleep lowers testosterone and increases stress |
Step-by-Step Guide to Addressing Erectile Concerns
If you’re struggling to get fully hard, follow this practical sequence to identify and resolve the cause:
- Track symptoms: Note frequency, context (alone vs. with partner), morning erections, and associated stressors.
- Visit a doctor: Request blood work (testosterone, glucose, cholesterol), blood pressure check, and possibly a referral to a urologist.
- Review medications: Ask whether any prescriptions you’re taking could contribute to ED.
- Improve lifestyle: Begin regular aerobic exercise, reduce alcohol, quit smoking, and prioritize sleep.
- Address mental health: Consider therapy for anxiety, depression, or relationship issues.
- Try medical treatment: Under supervision, test PDE5 inhibitors like sildenafil or tadalafil.
- Reassess after 8–12 weeks: Track progress and adjust approach as needed.
When to Seek Help—and Why You Shouldn’t Wait
Many men delay seeking help due to embarrassment or the belief that ED is an inevitable part of aging. But while incidence increases with age, it’s not a normal or unavoidable outcome. In fact, persistent ED can be an early marker of life-threatening conditions like heart disease. Studies show men with ED are at higher risk of heart attack or stroke within five years—often before other symptoms appear.
Early intervention improves outcomes. Whether through medication, therapy, or lifestyle change, most cases of ED are treatable. The sooner you act, the better your chances of restoring not just sexual function, but overall health.
Frequently Asked Questions
Is occasional difficulty getting hard normal?
Yes. Stress, fatigue, alcohol, or distraction can cause temporary issues. However, if it happens more than 25% of the time over several weeks, it may indicate a deeper problem.
Can anxiety really prevent a full erection?
Absolutely. The brain controls the start of the erectile process. If you’re anxious—about performance, relationships, or life in general—your nervous system may block the signal needed for full blood flow.
Do ED medications work for everyone?
No. While PDE5 inhibitors like Viagra help about 70% of men, they don’t work for those with severe nerve damage, certain hormonal imbalances, or who take nitrates for heart conditions. A doctor can help determine suitability.
Checklist: First Steps Toward Better Erectile Health
- ✅ Schedule a physical exam with blood tests (testosterone, glucose, lipids)
- ✅ Assess current medications with your doctor
- ✅ Start a walking routine (30 minutes, 5 days/week)
- ✅ Limit alcohol to moderate levels (1–2 drinks max)
- ✅ Quit smoking or seek support to stop
- ✅ Track morning erections for two weeks
- ✅ Open up to your partner about concerns
- ✅ Consider speaking with a therapist or counselor
Conclusion: Take Control of Your Sexual and Overall Health
Struggling to get fully hard doesn’t mean you’re broken—it means your body or mind is sending a signal worth listening to. Whether the root is physical, emotional, or a mix of both, effective solutions exist. Ignoring the issue risks missing critical health warnings and straining personal relationships. But taking action—starting with a conversation, a check-up, or a simple lifestyle shift—can lead to meaningful improvement.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?