Trying to conceive can be an emotional journey, especially when pregnancy doesn’t happen as quickly as expected. While many couples assume conception will occur within a few months, the reality is that infertility affects about 1 in 6 couples worldwide. Understanding the reasons behind difficulty conceiving, recognizing potential symptoms, and knowing when to consult a specialist are critical steps toward building a family.
Understanding Fertility: The Basics
Fertility depends on a complex interplay of hormones, anatomy, and timing. For conception to occur, several conditions must align: ovulation must happen regularly, sperm must be healthy and mobile, the fallopian tubes must be open, and the uterine lining must support implantation. Disruptions in any of these areas can delay or prevent pregnancy.
It’s important to remember that infertility is not solely a “woman’s issue.” Approximately one-third of cases stem from female factors, one-third from male factors, and the remaining third involve combined issues or remain unexplained.
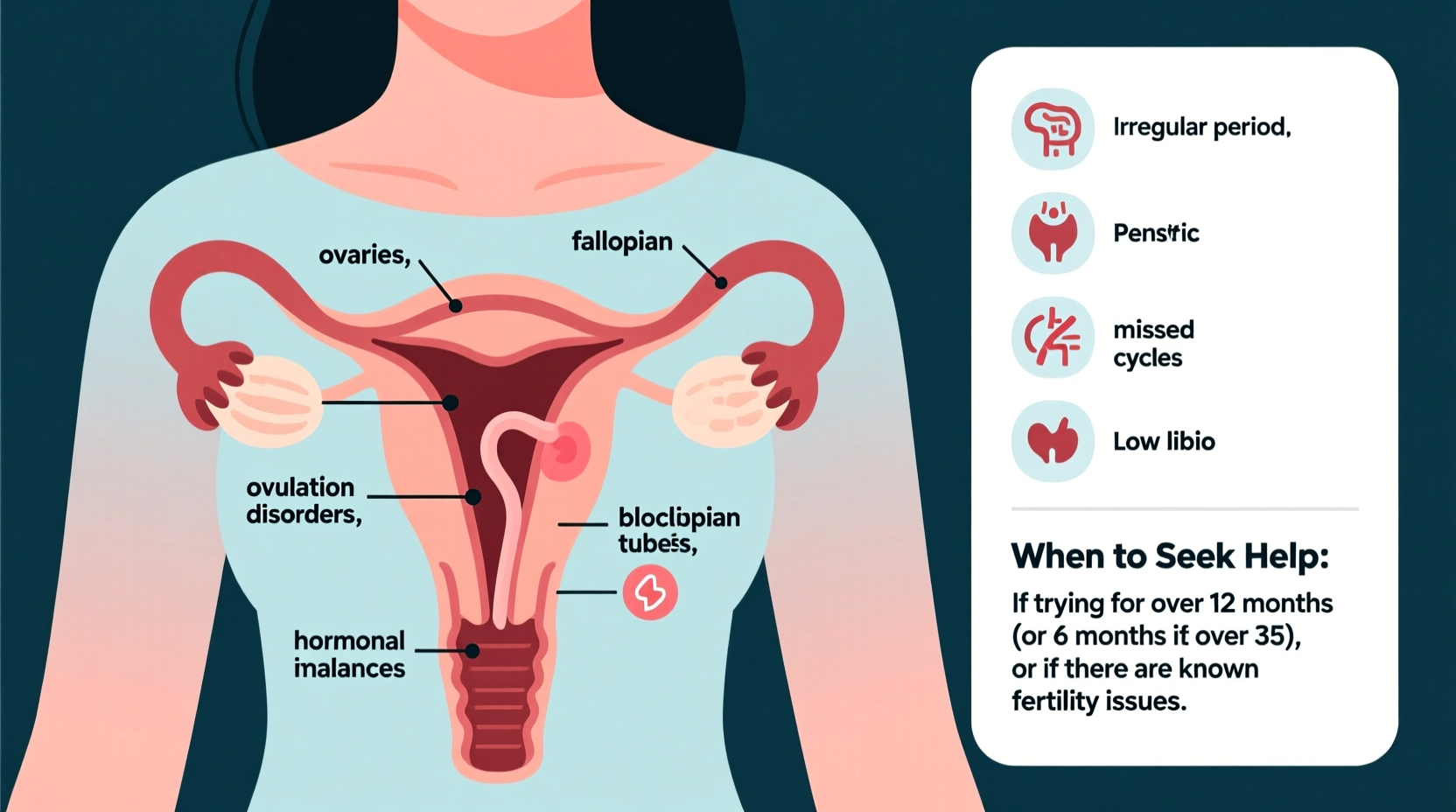
Common Causes of Female Infertility
Several medical and lifestyle factors can interfere with a woman’s ability to conceive:
- Ovulation disorders: Conditions like polycystic ovary syndrome (PCOS), hypothalamic dysfunction, or premature ovarian insufficiency disrupt regular egg release.
- Tubal blockages: Infections such as pelvic inflammatory disease (PID) or endometriosis can damage or block fallopian tubes, preventing sperm and egg from meeting.
- Uterine or cervical abnormalities: Fibroids, polyps, or congenital malformations may interfere with implantation or sperm passage.
- Endometriosis: This condition occurs when tissue similar to the uterine lining grows outside the uterus, causing inflammation, scarring, and impaired organ function.
- Age-related decline: Fertility begins to decline gradually after age 30 and more rapidly after 35 due to reduced egg quantity and quality.
Male Infertility: Often Overlooked but Equally Important
Men contribute to nearly half of all infertility cases. Common causes include:
- Low sperm count or poor motility: Sperm may be too few in number or unable to move effectively toward the egg.
- Seminal duct obstruction: Blockages in the tubes that carry sperm can result from infections, surgery, or congenital defects.
- Hormonal imbalances: Issues with the pituitary gland or testes can affect testosterone and sperm production.
- Lifestyle factors: Smoking, excessive alcohol use, obesity, and prolonged exposure to heat (e.g., hot tubs, tight underwear) negatively impact sperm health.
- Varicocele: Enlarged veins in the scrotum increase temperature and impair sperm development.
“Infertility evaluation should always include both partners. Assuming it’s a female issue delays diagnosis and treatment.” — Dr. Lena Patel, Reproductive Endocrinologist
Symptoms That May Signal Fertility Issues
Some signs may indicate underlying fertility problems, though many causes have no obvious symptoms. Pay attention to:
- Irregular or absent menstrual periods
- Painful periods, which may suggest endometriosis
- Heavy or unusually light bleeding
- Hormonal changes like acne, hair loss, or unwanted facial hair (possible PCOS)
- Pain during sex (dyspareunia), potentially linked to endometriosis or scarring
- History of pelvic infections or sexually transmitted diseases
- Erectile dysfunction or pain during ejaculation in male partners
However, many individuals with fertility challenges experience completely normal cycles and no physical symptoms. This is why timing and proactive evaluation matter.
When to Seek Medical Help
The general guideline is:
| Age Group | Recommended Timeframe to Seek Help |
|---|---|
| Under 35 | After 12 months of unprotected, regular intercourse without conception |
| 35 or older | After 6 months of trying |
| Known risk factors (e.g., endometriosis, PCOS, prior surgeries) | Immediately or within 6 months |
If you’ve had recurrent miscarriages (two or more), evaluation is recommended regardless of age or duration of trying.
Step-by-Step: What to Expect When Seeking Help
- Initial consultation: A reproductive specialist will review medical history, menstrual patterns, sexual frequency, and lifestyle factors.
- Blood tests: Hormone levels (FSH, AMH, TSH, prolactin) are checked to assess ovarian reserve and thyroid function.
- Imaging: A transvaginal ultrasound evaluates the uterus and ovaries; a hysterosalpingogram (HSG) checks for tubal patency.
- Semen analysis: The male partner provides a sample to evaluate sperm count, motility, and morphology.
- Further testing (if needed): Laparoscopy for suspected endometriosis, genetic screening, or specialized sperm function tests.
Real-Life Example: Sarah and Mark’s Journey
Sarah, 37, and Mark, 39, tried for a baby for ten months without success. Sarah had regular cycles but was diagnosed with mild endometriosis in her twenties. At her OB-GYN’s suggestion, they sought help early. Testing revealed that while Sarah’s tubes were clear, Mark had low sperm motility due to a varicocele. After corrective surgery and six months of timed intercourse, they conceived naturally. Their story highlights the importance of not waiting too long—and how male factors can play a decisive role.
Actionable Checklist: Steps to Take Now
Whether you’re just starting to try or have been trying for months, this checklist can help you stay proactive:
- Track your menstrual cycle using a calendar or app to identify patterns.
- Have sex every 2–3 days throughout the month to maximize chances around ovulation.
- Avoid smoking, limit alcohol, maintain a healthy weight, and reduce stress.
- Start taking a prenatal vitamin with at least 400 mcg of folic acid.
- Encourage your partner to avoid hot tubs, saunas, and tight underwear.
- Schedule a preconception checkup with your doctor.
- Discuss family history of infertility or genetic conditions with both sides.
Frequently Asked Questions
Can stress really prevent me from getting pregnant?
While everyday stress is unlikely to cause infertility, chronic, severe stress may disrupt hormone balance and ovulation. Managing stress through mindfulness, exercise, or counseling supports overall reproductive health—but it’s rarely the sole cause of infertility.
I have regular periods. Does that mean I’m definitely ovulating?
Not always. Some women experience “anovulatory cycles” where bleeding occurs without ovulation. Tracking basal body temperature or using ovulation predictor kits can confirm whether ovulation is happening.
Are fertility treatments my only option if I can’t conceive naturally?
No. Many couples achieve pregnancy with relatively simple interventions like medication to induce ovulation (e.g., clomiphene citrate), intrauterine insemination (IUI), or lifestyle adjustments. IVF is typically reserved for more complex cases.
Final Thoughts: You’re Not Alone
Struggling to conceive is more common than many realize, and help is available. Early evaluation empowers you with knowledge and options. Whether the cause is hormonal, structural, or related to sperm health, modern medicine offers effective solutions. Don’t hesitate to advocate for yourself—timing matters, and so does support.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?