Trying to conceive can be an emotional journey, especially when pregnancy doesn’t happen as quickly as expected. While many couples assume conception should occur within a few months, the reality is that fertility varies widely. Understanding the potential causes of infertility and knowing when to seek professional guidance can make all the difference in building your family.
Infertility affects about 1 in 6 couples globally, according to the World Health Organization. It’s not a reflection of failure or personal shortcoming—it’s a medical condition with identifiable causes and effective treatments. This article outlines the most common reasons why conception may be delayed, signs that it’s time to consult a specialist, and practical steps to improve your chances of success.
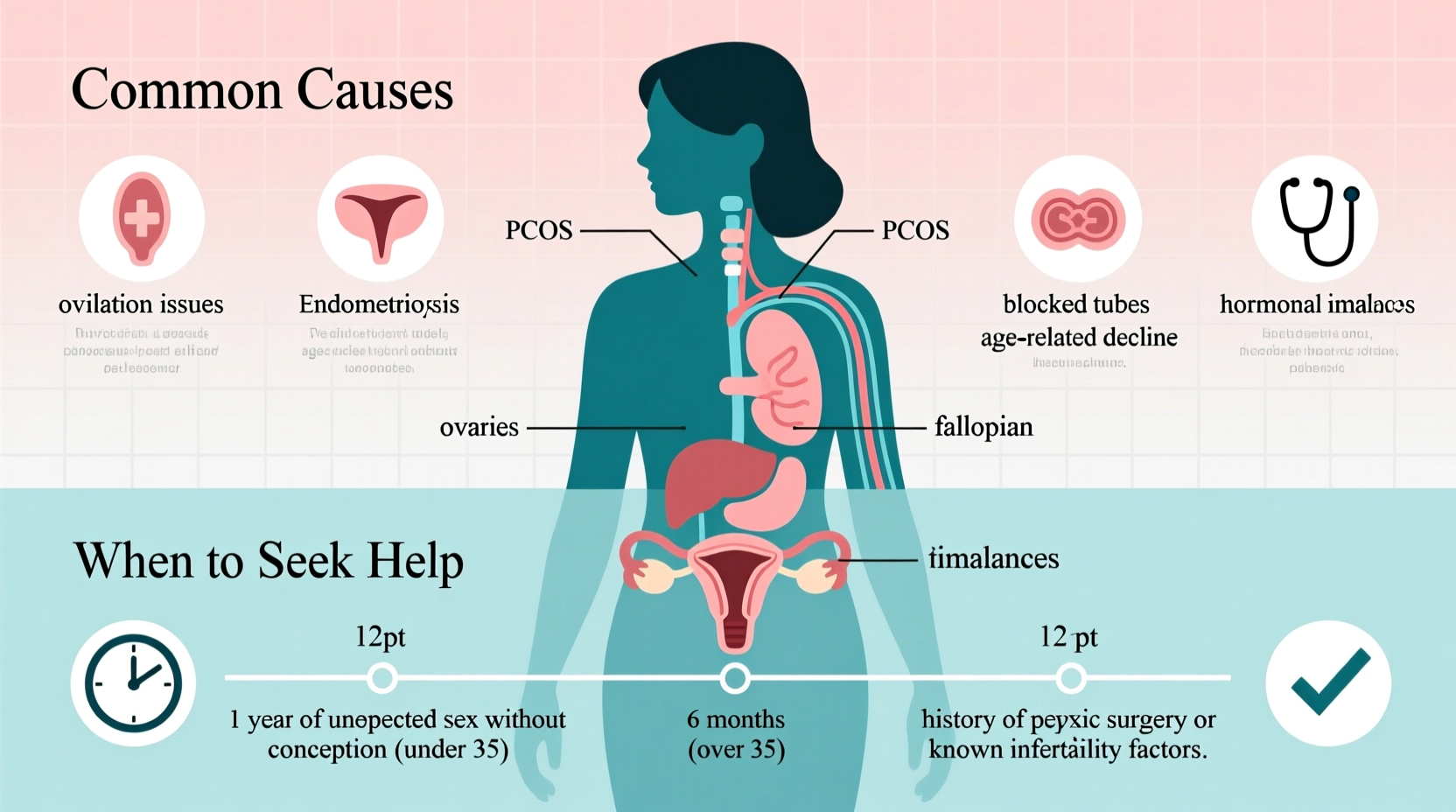
Common Medical Reasons You Can’t Get Pregnant
Infertility can stem from male factors, female factors, or a combination of both. In some cases, no clear cause is found—a situation known as unexplained infertility. Below are the most frequent biological barriers to conception.
Ovulation Disorders
Ovulation problems account for nearly 25% of female infertility cases. Irregular or absent ovulation prevents the release of mature eggs, making conception difficult. Common conditions include:
- Polycystic Ovary Syndrome (PCOS): Hormonal imbalances lead to irregular cycles and elevated androgen levels.
- Hypothalamic dysfunction: Stress, extreme weight loss, or excessive exercise disrupts hormone signals.
- Premature ovarian insufficiency: Ovaries stop functioning before age 40, reducing egg supply.
Tubal and Uterine Factors
Damaged or blocked fallopian tubes prevent sperm from reaching the egg. Causes include pelvic inflammatory disease (often from untreated STIs), endometriosis, or prior abdominal surgeries. Similarly, uterine abnormalities—such as fibroids, polyps, or scar tissue (Asherman’s syndrome)—can interfere with embryo implantation.
Male Factor Infertility
Up to 40% of infertility cases involve male reproductive issues. These typically relate to sperm quality, including:
- Low sperm count (oligospermia)
- Poor motility (asthenospermia)
- Abnormal morphology (teratospermia)
Contributing factors include varicoceles, infections, hormonal imbalances, genetic conditions, or lifestyle habits like smoking, excessive alcohol use, and prolonged heat exposure (e.g., hot tubs).
Age-Related Fertility Decline
Fertility naturally declines with age, particularly after 35. Women are born with a finite number of eggs, which decrease in quantity and quality over time. Men also experience a gradual decline in sperm health after 40, though less sharply than women.
When to Seek Help: A Timeline for Action
There’s no one-size-fits-all answer to when you should see a doctor, but guidelines exist based on age and risk factors. Delaying evaluation can reduce treatment effectiveness, especially if underlying conditions go undiagnosed.
“Couples under 35 should try for one year before seeking help. For women over 35, that window shortens to six months due to the accelerated decline in ovarian reserve.” — Dr. Rachel Nguyen, Reproductive Endocrinologist
Recommended Evaluation Timelines
| Age Group | Time to Try Before Seeking Help | Notes |
|---|---|---|
| Under 35 | 12 months | Regular, unprotected sex at least 2–3 times per week |
| 35–40 | 6 months | Earlier evaluation advised due to faster fertility decline |
| Over 40 | Immediately | Consider preconception testing even before trying |
| Known risk factors | Immediately | Endometriosis, PCOS, prior surgeries, or male reproductive history |
Step-by-Step Guide: What to Expect When Seeking Help
- Initial consultation: Review medical history, menstrual patterns, sexual frequency, and lifestyle factors.
- Blood tests: Check hormone levels (FSH, LH, AMH, thyroid, prolactin) to assess ovarian reserve and ovulation function.
- Semen analysis: Evaluates sperm count, motility, and morphology—required early in the process.
- Imaging: Transvaginal ultrasound checks for structural issues; hysterosalpingogram (HSG) examines tube patency.
- Diagnosis and treatment plan: Based on findings, options may include medication (e.g., clomiphene), IUI, or IVF.
Lifestyle and Environmental Influences
While medical issues are often central, daily habits can significantly impact fertility. Some modifiable factors include:
- Weight: Both underweight and overweight states can disrupt hormonal balance and ovulation.
- Diet: Diets high in trans fats, sugar, and processed foods are linked to lower fertility. Emphasize whole grains, lean proteins, healthy fats, and antioxidants.
- Smoking and alcohol: Smoking reduces ovarian response and increases miscarriage risk. Alcohol consumption above moderate levels negatively affects both male and female fertility.
- Stress: Chronic stress may alter hormone production and reduce sexual frequency, though its direct role in infertility remains debated.
Mini Case Study: Sarah and James’ Journey
Sarah, 37, and James, 39, had been trying to conceive for ten months without success. They tracked ovulation using kits and maintained regular intercourse during her fertile window. Concerned, they consulted a fertility specialist after eight months due to Sarah’s age.
Testing revealed normal ovarian reserve and patent tubes, but James’s semen analysis showed low motility. The diagnosis: mild male factor infertility. Their doctor recommended intrauterine insemination (IUI) with ovarian stimulation. After two cycles, Sarah became pregnant and gave birth to a healthy baby boy.
Their story highlights the importance of timely intervention—even when one partner appears to have no obvious issues. Male fertility is often overlooked, yet plays a crucial role.
Fertility Checklist: Actions to Take Now
Whether you’re just starting to try or have been unsuccessful for months, this checklist can help you prepare physically and emotionally:
- Track your menstrual cycle for at least three months to identify patterns.
- Use ovulation predictor kits or monitor cervical mucus changes.
- Have sex every other day during your fertile window (days 10–18 in a 28-day cycle).
- Both partners should undergo basic fertility screening if over 35 or if concerns exist.
- Adopt a fertility-friendly lifestyle: maintain healthy weight, quit smoking, limit alcohol, and reduce caffeine.
- Start taking prenatal vitamins with at least 400 mcg of folic acid.
- Discuss family medical history with your doctor—especially early menopause or genetic conditions.
Frequently Asked Questions
Can you be infertile even with regular periods?
Yes. Regular cycles don’t guarantee ovulation or optimal egg quality. Some women with PCOS or luteal phase defects menstruate regularly but do not ovulate effectively.
Does stress really affect fertility?
While acute stress is unlikely to cause infertility, chronic stress may influence hormones that regulate reproduction. More importantly, stress can reduce sexual frequency and delay seeking care. Managing stress through mindfulness, therapy, or support groups can improve overall well-being during the process.
How much does fertility treatment cost?
Costs vary widely. A round of Clomid with monitoring may cost $500–$1,500. IUI ranges from $800–$3,000 per cycle. IVF averages $12,000–$15,000 per cycle, not including medications. Insurance coverage varies by state and provider—check your plan early.
Take Control of Your Fertility Journey
Struggling to get pregnant doesn’t mean you won’t become a parent—it may simply mean you need support along the way. Advances in reproductive medicine have made it possible for countless individuals and couples to overcome infertility. The key is acting early, staying informed, and seeking compassionate care.
If you’ve been trying without success, don’t wait indefinitely. Use the timelines and checklist above to determine your next steps. Speak openly with your partner, reach out to a trusted healthcare provider, and remember—you’re not alone. Thousands walk this path every year, and many find their way to parenthood with the right help.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?