As pregnancy progresses, many women notice changes in their sleep patterns and physical comfort—especially when trying to lie down. One common piece of advice from healthcare providers is to avoid lying on your back, particularly in the second and third trimesters. But why exactly is this position discouraged? Understanding the physiological changes during pregnancy, the risks associated with supine positioning, and safer alternatives can help expecting mothers make informed choices for themselves and their babies.
The Science Behind Back Sleeping Risks
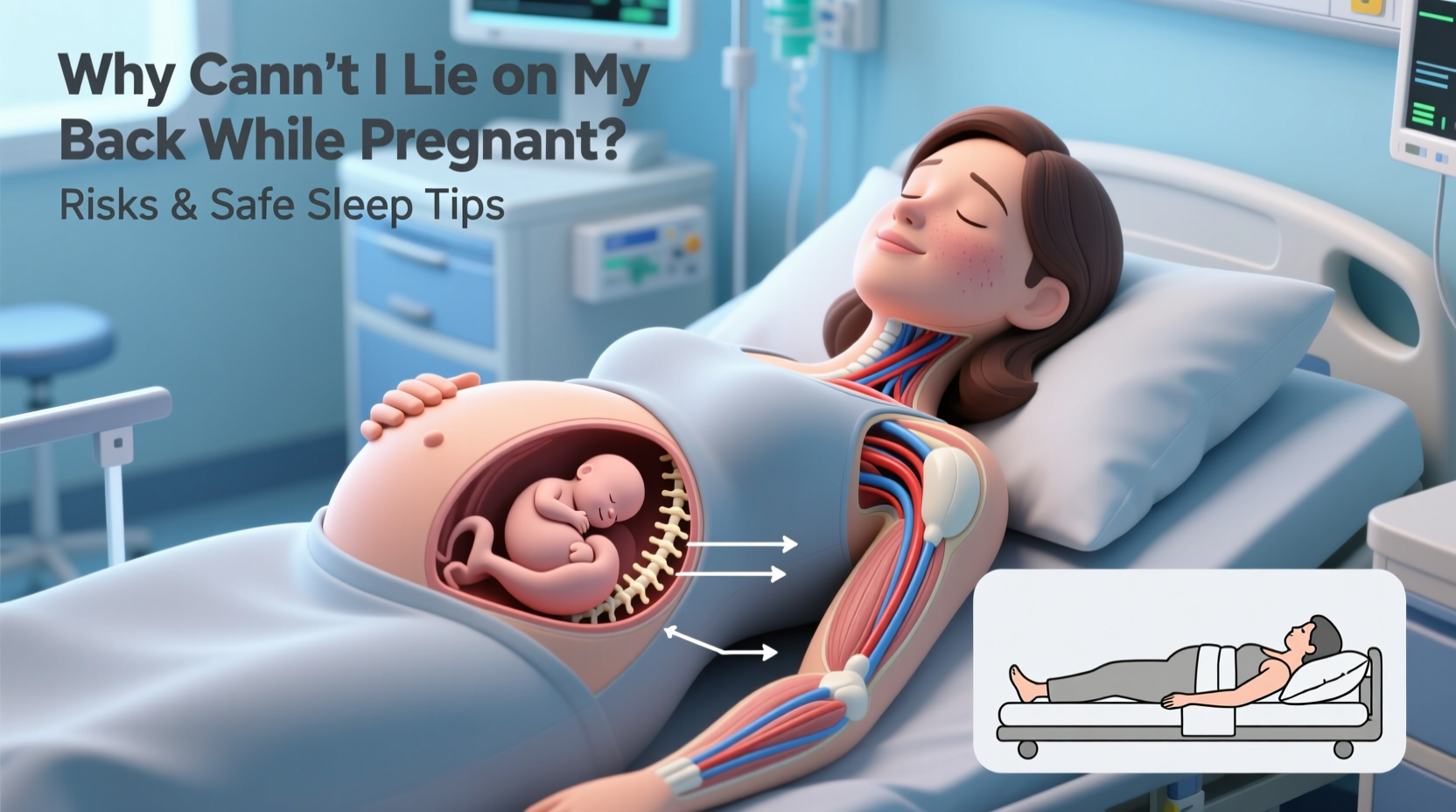
During pregnancy, especially after 20 weeks, the growing uterus shifts significantly in size and weight. When a pregnant person lies flat on their back, the full weight of the uterus can compress the inferior vena cava—a large vein that carries deoxygenated blood from the lower body back to the heart. This condition is known as supine hypotensive syndrome or aortocaval compression.
Compression of the vena cava reduces blood return to the heart, which in turn lowers cardiac output. This can lead to:
- Dizziness or lightheadedness
- Nausea
- Shortness of breath
- Low blood pressure
- Reduced oxygen flow to the fetus
Studies have shown that reduced uterine blood flow due to back-lying positions may be linked to adverse outcomes, including lower birth weight and increased risk of stillbirth in later pregnancy. A 2019 study published in *The Lancet* found that women who went to sleep on their back in the third trimester had a higher risk of late stillbirth compared to those who slept on their side.
“After mid-pregnancy, sleeping on the back can compromise maternal circulation and fetal oxygenation. Side-sleeping, especially left-side, is strongly encouraged.” — Dr. Jane Harding, Professor of Neonatal Physiology, University of Auckland
When Does It Become Dangerous?
While occasional rolling onto the back during sleep is unlikely to cause harm, prolonged periods in this position—especially during deep sleep—are concerning. The risk increases significantly after week 28, when the uterus is large enough to exert meaningful pressure on major blood vessels.
It's important to note that it’s not just about how you fall asleep, but also your final sleep position. Research suggests that the position you go to sleep in matters most—not necessarily the position you wake up in, since movement during the night is normal.
Safer Sleep Positions During Pregnancy
The safest and most recommended sleep position during pregnancy is side-lying, preferably on the left side. This position maximizes blood flow to the placenta, kidneys, and uterus because it avoids compression of the inferior vena cava and supports optimal circulation.
However, right-side sleeping is also acceptable if left-side proves uncomfortable. The goal is to remain off the back and avoid flat supine positions.
Supportive Strategies for Side Sleeping
Maintaining a side-sleeping posture throughout the night can be challenging. Consider these practical adjustments:
- Use a full-body pregnancy pillow to support the belly, back, and legs.
- Place a pillow between the knees to align the spine and reduce hip strain.
- Elevate the upper body slightly with an incline pillow if experiencing heartburn.
- Try a small rolled towel under the right hip to encourage left tilt.
Do’s and Don’ts of Pregnancy Sleep
| Do’s | Don’ts |
|---|---|
| Do sleep on your side (left preferred) | Don’t lie flat on your back after 20 weeks |
| Do use supportive pillows for alignment | Don’t ignore persistent dizziness or shortness of breath at night |
| Do get up slowly to prevent blood pressure drops | Don’t sleep on soft, sinking mattresses that make repositioning hard |
| Do maintain a consistent sleep schedule | Don’t consume caffeine late in the day |
Real-Life Example: Sarah’s Third Trimester Adjustment
Sarah, a first-time mother at 32 weeks, began waking up frequently with a racing heart and nausea. Her midwife asked about her sleep habits and discovered she was falling asleep reclined on the couch—often drifting into a flat-back position. After switching to side-sleeping in bed with a C-shaped pregnancy pillow, her symptoms resolved within days. An ultrasound later confirmed improved amniotic fluid levels and steady fetal growth, reinforcing the impact of positional changes on circulation and fetal well-being.
Step-by-Step Guide to Transitioning to Safer Sleep
Changing long-standing sleep habits takes time. Follow this timeline to ease into a healthier routine:
- Week 1: Begin by consciously lying on your side when going to sleep. Use reminders like sticky notes on the nightstand.
- Week 2: Introduce a body pillow or wedge to make side-sleeping more comfortable.
- Week 3: Practice getting into your ideal sleep position during naps to build muscle memory.
- Week 4: Assess comfort and adjust pillow placement. Consider a firmer mattress if sinking makes rolling difficult.
- Ongoing: Monitor how you feel upon waking. Energy levels, absence of dizziness, and fetal movement are good indicators of proper circulation.
Frequently Asked Questions
Can I lie on my back for short periods during the day?
Yes, brief periods—such as during a massage or prenatal exam—are generally safe, especially if you’re not feeling dizzy or unwell. However, avoid extended rest or napping on your back after 20 weeks. Always listen to your body; discomfort is a sign to reposition.
What if I naturally roll onto my back at night?
Movement during sleep is normal. The critical factor is your starting position. Research shows that going to sleep on your side significantly reduces risks, even if you shift positions later. Focus on setting up your environment to discourage back-sleeping, such as using supportive pillows.
Is left-side sleeping really better than right-side?
Left-side sleeping is preferred because it enhances circulation to the heart, kidneys, and uterus by keeping pressure off the inferior vena cava, which runs along the right side of the spine. However, right-side sleeping is still much safer than back-sleeping and is acceptable if left-side causes discomfort.
Final Thoughts and Action Plan
While the idea of completely changing how you sleep might seem daunting, the benefits to both maternal comfort and fetal health are well worth the effort. The human body adapts remarkably during pregnancy, and with a few strategic adjustments, safer sleep becomes second nature.
You don’t need perfection—just awareness and consistency. Start tonight: position yourself on your side, use supportive tools, and create a bedtime routine that prioritizes your well-being. Small changes now can have lasting impacts on your pregnancy journey.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?