Urinary retention—the inability to fully or completely empty the bladder—is a surprisingly common condition that affects both men and women, though it’s more prevalent in older adults. While an occasional delay in urination may not be alarming, persistent difficulty urinating can signal underlying health issues. Left untreated, urinary retention can lead to complications such as bladder damage, urinary tract infections (UTIs), or even kidney problems. Understanding the causes, recognizing early symptoms, and knowing when to act are essential steps toward effective management.
What Is Urinary Retention?
Urinary retention is categorized into two types: acute and chronic. Acute urinary retention occurs suddenly and is considered a medical emergency. It involves a complete inability to urinate despite a full bladder, often accompanied by severe discomfort or pain in the lower abdomen. Chronic urinary retention develops gradually. Individuals may feel they never fully empty their bladder, experience frequent urination, or have a weak urine stream without sharp pain.
The body relies on a complex coordination between the brain, spinal cord, nerves, and muscles to control urination. When any part of this system fails—due to obstruction, nerve dysfunction, or muscle weakness—urinary retention can occur.
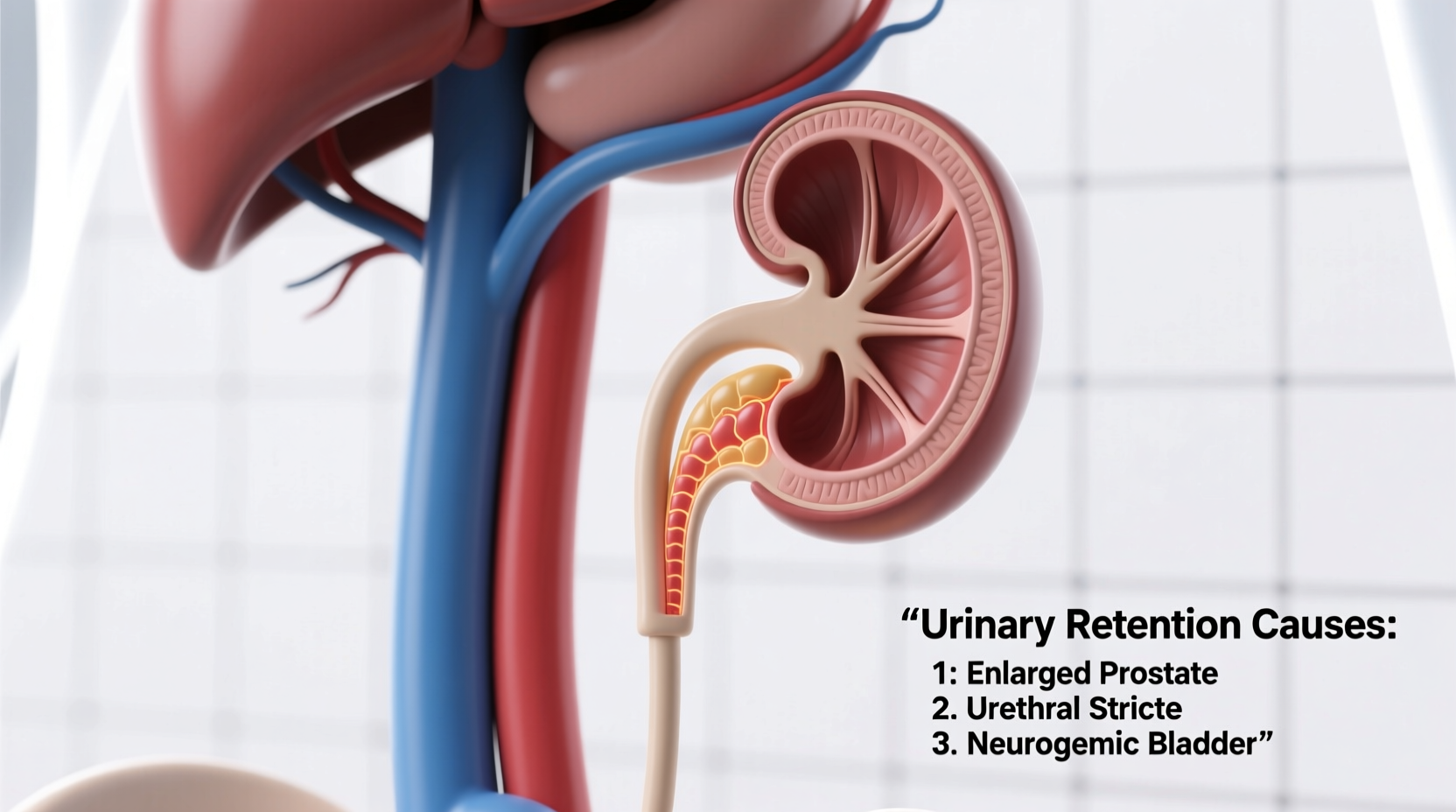
Possible Causes of Urinary Retention
Several factors can interfere with normal bladder function. The most common causes fall into three broad categories: physical obstructions, neurological issues, and medication side effects.
1. Obstructive Causes
Blockages in the urinary tract prevent urine from flowing freely out of the bladder. In men, the most frequent cause is benign prostatic hyperplasia (BPH)—an enlarged prostate gland that compresses the urethra. Other obstructive conditions include:
- Prostate cancer
- Urethral strictures (narrowing of the urethra)
- Bladder stones
- Pelvic organ prolapse (in women)
- Tumors in the pelvic region
2. Neurological Disorders
The nervous system controls bladder contraction and sphincter relaxation. Damage to these pathways disrupts communication and leads to retention. Conditions associated with neurogenic bladder include:
- Diabetes (via diabetic neuropathy)
- Multiple sclerosis
- Spinal cord injuries
- Parkinson’s disease
- Stroke
3. Medication-Induced Retention
Certain drugs interfere with bladder muscle function or increase resistance in the urethra. Common culprits include:
- Antihistamines
- Decongestants (e.g., pseudoephedrine)
- Antidepressants (especially tricyclics)
- Antipsychotics
- Opioid painkillers
“Many patients don’t realize their cold medicine could be causing urinary retention—especially if they already have prostate issues.” — Dr. Alan Reyes, Urologist at Boston Medical Center
Who Is at Risk?
While anyone can experience urinary retention, certain groups face higher risks:
- Men over 50: Prostate enlargement significantly increases risk.
- Individuals with diabetes: Nerve damage from prolonged high blood sugar affects bladder control.
- Pelvic surgery patients: Procedures like hysterectomies or prostate surgeries may damage nearby nerves.
- People taking multiple medications: Polypharmacy raises the chance of drug-induced retention.
Additionally, immobility, severe constipation, and psychological stress can contribute to temporary retention episodes.
Recognizing the Symptoms
Symptoms vary depending on whether retention is acute or chronic:
| Symptom Type | Acute Retention | Chronic Retention |
|---|---|---|
| Onset | Sudden | Gradual |
| Pain Level | Severe lower abdominal pain | Mild discomfort or none |
| Urination Ability | Inability to urinate | Weak stream, frequent urges |
| Bladder Fullness | Palpable distension | May go unnoticed |
| Associated Risks | Kidney damage, infection | Recurrent UTIs, overflow incontinence |
Chronic cases are particularly dangerous because people may adapt to the symptoms, dismissing them as normal aging. However, ongoing retention can silently damage the bladder and kidneys over time.
Diagnostic Process and Medical Evaluation
If you’re struggling to urinate, your doctor will likely perform a series of assessments to determine the cause. These may include:
- Medical history review: Focus on medications, prior surgeries, and existing conditions like diabetes or BPH.
- Physical examination: Includes a digital rectal exam (DRE) in men to assess prostate size.
- Bladder scan: Uses ultrasound to measure post-void residual (PVR) volume—how much urine remains after urination. A PVR over 100–150 mL suggests retention.
- Urodynamic testing: Evaluates bladder pressure and flow rate during urination.
- Blood tests: Check kidney function and PSA levels (for prostate screening).
- Imaging: CT scans or MRI may identify tumors, stones, or structural abnormalities.
Mini Case Study: John’s Sudden Inability to Urinate
John, a 62-year-old man with mild BPH, took a decongestant for a cold. Within 12 hours, he felt increasing pressure in his lower abdomen and couldn’t urinate. He went to the ER, where a bladder scan revealed over 800 mL of retained urine. A catheter was inserted immediately to relieve the blockage. After discontinuing the decongestant and starting alpha-blockers for his prostate, John recovered fully. His case highlights how a seemingly harmless medication can trigger acute retention in at-risk individuals.
Treatment and Management Options
Treatment depends on the cause and severity:
- Catheterization: For acute cases, a temporary catheter drains the bladder. Some chronic patients require intermittent self-catheterization.
- Medications: Alpha-blockers (like tamsulosin) relax prostate and bladder neck muscles. 5-alpha reductase inhibitors shrink the prostate over time.
- Surgery: Procedures such as transurethral resection of the prostate (TURP) remove excess prostate tissue.
- Behavioral changes: Double voiding (urinating, waiting, then trying again), scheduled bathroom visits, and managing constipation help reduce symptoms.
Prevention Checklist
To reduce your risk of urinary retention, follow this actionable checklist:
- Review all medications with your doctor, especially antihistamines and decongestants.
- Stay hydrated but avoid excessive fluid intake before bedtime.
- Treat constipation promptly—bowel fullness can press on the bladder.
- Limit alcohol and caffeine, which can irritate the bladder.
- Men over 50 should have annual prostate screenings.
- Avoid holding urine for long periods.
- Monitor diabetes and maintain healthy blood sugar levels.
Frequently Asked Questions
Can anxiety cause urinary retention?
Yes. Severe anxiety or stress—especially in public restrooms—can trigger \"paruresis\" or shy bladder syndrome, where the person cannot initiate urination despite needing to. This is a functional rather than physical blockage and may require behavioral therapy.
Is urinary retention life-threatening?
Acute retention is a medical emergency. If urine cannot exit the bladder, pressure builds and can back up into the kidneys, causing hydronephrosis and potential kidney failure. Immediate treatment is critical.
Can women get urinary retention?
Yes. While less common than in men, women can develop retention due to pelvic organ prolapse, nerve damage from childbirth, or after pelvic surgery. Bladder outlet obstruction is rarer but possible.
Conclusion: Take Action Before It Escalates
Difficulty urinating should never be ignored. Whether it's a sudden blockage or a slow decline in bladder function, identifying the root cause early can prevent serious complications. Many causes of urinary retention are treatable, especially when caught in time. Don’t dismiss symptoms as part of aging or stress. Speak with a healthcare provider, review your medications, and take proactive steps to support urinary health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?